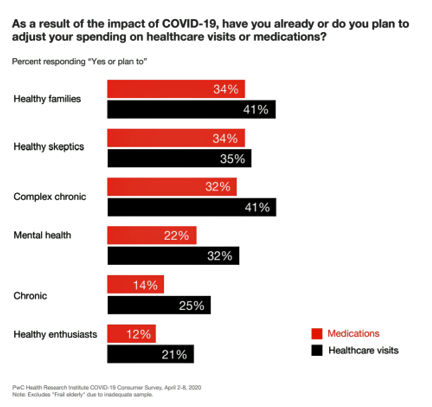
Patients in the U.S. are self-rationing care in the era of COVID-19 by cutting spending on health care visits and prescription drugs. The coronavirus pandemic’s impact on health consumers’ spending varies depending on whether the household is generally a healthy family unit, healthy “enthusiasts,” dealing with a simple or more complex chronic conditions, or managing mental health issues.
 PwC explored how COVID-19 is influencing consumers’ health care behaviors in survey research conducted in early April by the Health Research Institute. The findings were published in a May 2020 report, detailing study findings among 2,533 U.S. adults polled in early April 2020.
PwC explored how COVID-19 is influencing consumers’ health care behaviors in survey research conducted in early April by the Health Research Institute. The findings were published in a May 2020 report, detailing study findings among 2,533 U.S. adults polled in early April 2020.
Differences across the six consumer health-profile segments, the greatest spending adjustments have been made to healthcare visits among healthy families and people managing complex chronic conditions. Imagine each end of this spectrum: for healthy families, perhaps healthy child visits for vaccinations or general physicals for Mom or Dad. For families dealing with complex chronic conditions such as the trifecta of diabetes, high blood pressure and obesity, putting off visits for check-ups on foot health, heart function, or weight management.
The red bar shows prescription drug spending changes, most notable for healthy families, healthy skeptics, and those with complex chronic conditions.
“Delaying procedures, reducing spending on preventive care and chronic care, and decreasing adherence to medications may have negative long-term impacts on health status, although the extent is unknown,” PwC notes.
People with complex chronic conditions, already diagnosed with more than one medical challenge, are at high-risk in the COVID-19 pandemic for self-rationing care, and from having appointments cancelled by doctor’s offices and hospital outpatient departments locked down, in the short-term, for providing face-to-face care or for being intensely-focused inpatient coronavirus providers.
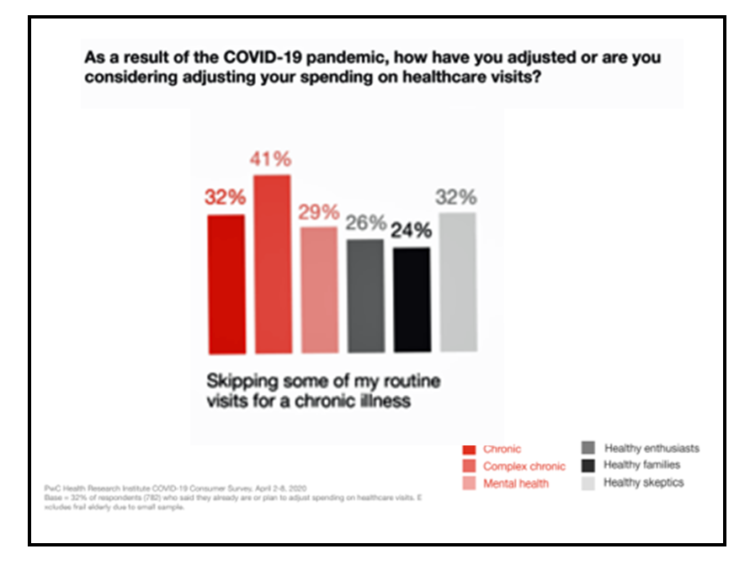
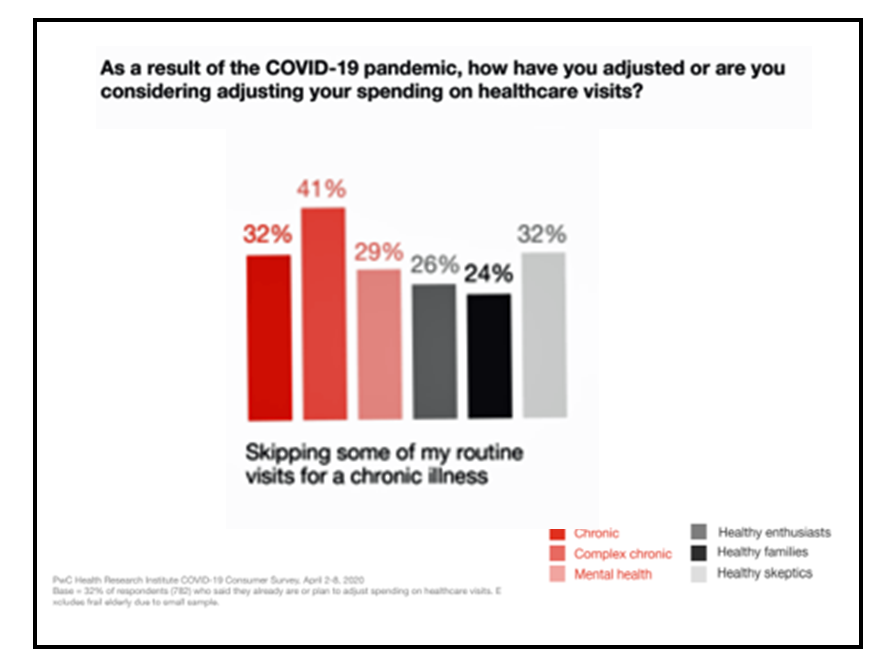 The second bar chart clearly illustrates the dilemma of the person dealing with complex chronic medical issues: 41% of these folks were skipping some routine visits for chronic illness, of which they have more than one.
The second bar chart clearly illustrates the dilemma of the person dealing with complex chronic medical issues: 41% of these folks were skipping some routine visits for chronic illness, of which they have more than one.
32% of people with one chronic condition were adjusting spending on health care visits due to COVID-19.
People with complex chronic conditions also adjusted these personal medical work-flows:
- 35% skipped annual physicals and well visits
- 23% skipped recommended lab tests or screenings
- 21% skipped elective procedures.
- 34% “thought twice” before asking their doctor for a prescription when they felt sick
- 34% looked for more over-the-counter medications
- 29% “stretched” some medications by skipping doses to save money
- 22% spent more to fill scripts for a longer period of time (90 days vs. 30 days).
Notably, 32% of families or people with complex chronic conditions, and 37% of those with one chronic condition, received health care treatment for the first time through a video telehealth visit.
Health Populi’s Hot Points: The positive finding in this research is that one-third of people dealing with at least one chronic condition sought health care through virtual means, telehealth, in the pandemic. A big question among those of us engaging in health care planning and forecasting “right now” is whether the fast uptake of virtual care services will persist after the coronavirus is managed via vaccine or aggressive, effective treatments — whether via texting by phone, using patient portals for asynchronous messaging to clinicians, health systems’ own telemedicine systems or direct-to-consumer telehealth companies.
Payors, both commercial and public sector (Medicare, Medicaid), have relaxed rules and regulations for telehealth across platforms (from purpose-built telemedicine programs to HIPAA-relaxed approvals for using FaceTime, Zoom, and other commercial channels), and have various plans to pay for virtual care visits between clinicians and patients.
Virtual care has aligned the interests of both clinicians and patients, both sides of the supply-and-demand care equation seeking to risk-manage exposure to the clever COVID-19 virus.
 The concerning learning here is that the self-rationing, or postponing, health care behaviors of millions of patients dealing with chronic conditions can exacerbate those issues, from foot health to vision health, delayed diagnoses for acute conditions, or un-managed care that will occasion an inpatient admission later in 2020.
The concerning learning here is that the self-rationing, or postponing, health care behaviors of millions of patients dealing with chronic conditions can exacerbate those issues, from foot health to vision health, delayed diagnoses for acute conditions, or un-managed care that will occasion an inpatient admission later in 2020.
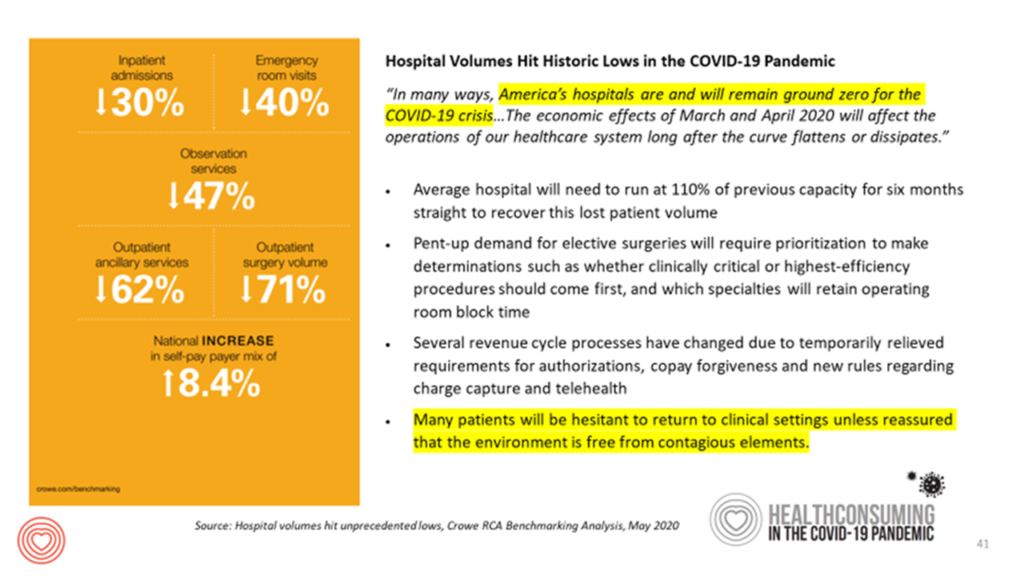
This scenario is in the sites of those of us working with hospitals to plan ahead for the fourth quarter of 2020 and first quarter of 2021 when two issues could converge:
- The second wave of COVID-19 infectious in the late autumn into the winter season; and,
- A wave of chronically ill people who postponed care earlier in 2020 who then need more acute, inpatient, and technology-dependent outpatient care that can’t be delivered via virtual modes.
In scenario planning mode, consider this worst-or-tough case scenario in light of what Crowe RCA calculated in a recent report on the financial impact of COVID-19 on hospitals: the average U.S. hospital will have to run at 110% of previous capacity for sixth months straight to recover the patient volume “lost” during the pandemic due to patients avoiding care as we see in the PwC data.
This scenario further bolsters the rationale for ensuring that telehealth and virtual care flows continue to become integrated into work-flows and health care throughout the U.S. to assure that precious and scarce inpatient capacity be available for the inevitable influx of both COVID-19 patients and people postponing necessary care that, for some, will be more intense than might have been needed upstream and earlier in 2020.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...