 Doctors maintain their top status as U.S. patients’ most-trusted source of coronavirus information. However, as patients continue to be concerned about exposure to COVID-19, 3 in 5 are concerned about being at-risk to the virus in their doctor’s office, according to research from the Alliance of Community Health Plans (ACHP) and AMCP, the Academy of Managed Care Pharmacy.
Doctors maintain their top status as U.S. patients’ most-trusted source of coronavirus information. However, as patients continue to be concerned about exposure to COVID-19, 3 in 5 are concerned about being at-risk to the virus in their doctor’s office, according to research from the Alliance of Community Health Plans (ACHP) and AMCP, the Academy of Managed Care Pharmacy.
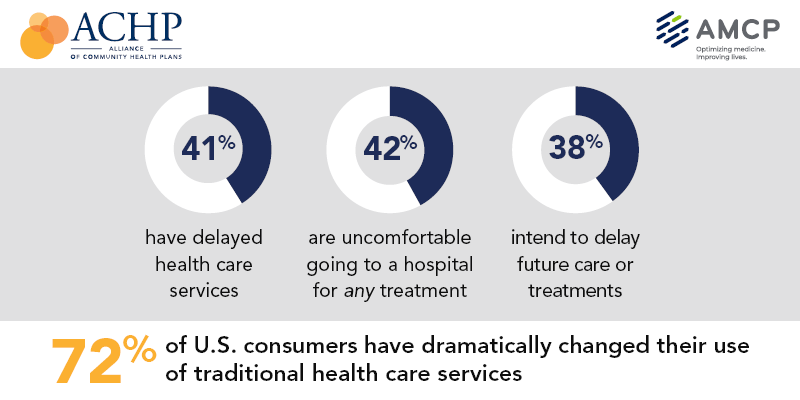
Patients’ concerns of COVID-19 risks have led them to self-ration care in the following ways:
- 41% have delayed health care services
- 42% felt uncomfortable going to a hospital for any medical treatment
- 45% felt uncomfortable using an urgent care or walk-in clinic, and,
- 38% intended to delay future care, treatment, and procedures.
ACHP and AMCP polled 1,263 U.S. adults 18 to 74 years of age in the first week of May 2020.
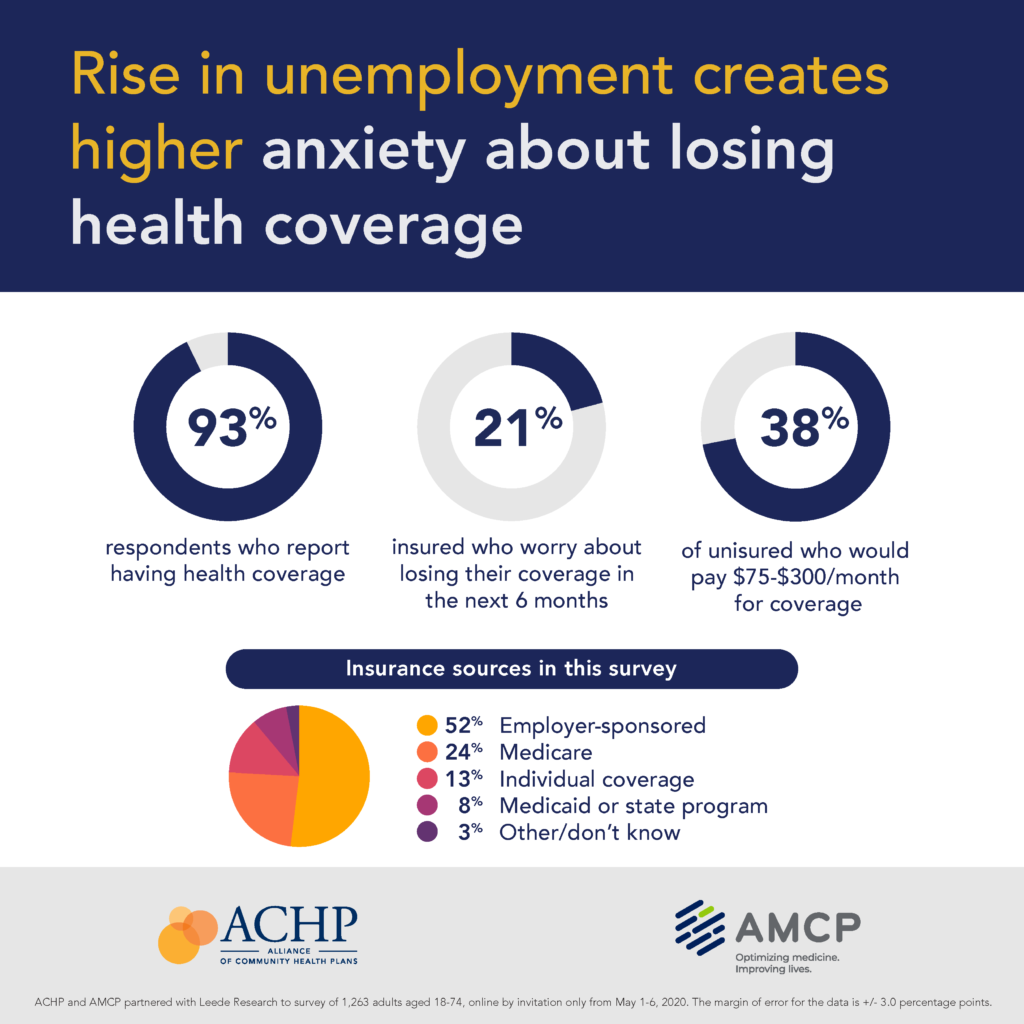 There are other forms of fear taking hold of the COVID-19 era health consumer: namely, financial anxiety in the wake of the pandemic. Nearly every respondent in the study reported having health insurance coverage.
There are other forms of fear taking hold of the COVID-19 era health consumer: namely, financial anxiety in the wake of the pandemic. Nearly every respondent in the study reported having health insurance coverage.
Among those covered with insurance, one-half had employer-sponsored insurance, 1 in 4 Medicare, and 13%, individual cover. Another 8% had Medicaid or a state health insurance program.
One in 5 of people with health insurance were concerned about losing their health plan in the next six months as the coronavirus heats up, recedes, and may re-emerge in the fourth quarter of 2020 into 2021.
That anxiety comes from the fact that most folks in this study believed it likely there would be a resurgence of COVID-19 in the fall or winter. Thus, 38% of people would delay an elective procedure and 27% would delay a diagnostic test in a hospital setting for at least six months.
There’s one test most Americans want to access: 64% of people want to be tested for COVID-19, but one-third are concerned about their ability to get the test.
Intriguingly, most patients would be comfortable getting that coronavirus test in their doctor’s office, which many would still be uncomfortable accessing other care from their personal physicians in the bricks-and-mortar office.
What’s the work-around to ensure that patients can access care from their personal physicians?
 Why it’s telehealth, of course, which has experienced hockey-stick growth in the U.S. (and around the globe) over the past three months.
Why it’s telehealth, of course, which has experienced hockey-stick growth in the U.S. (and around the globe) over the past three months.
Just this week, American Well announced an influx of $194 million dollars from investors recognizing the current value and ongoing relevance of virtual care in and beyond the pandemic.
As CEO and Co-Founder Dr. Ido Schoenberg said about the event, “No one ever modeled this level of growth…We had to ramp up the technology and upgrade both our hardware and software — and in addition to that, we had to onboard an enormous amount of providers,” now numbering over 50,000 licensed clinicians in the Amwell network.
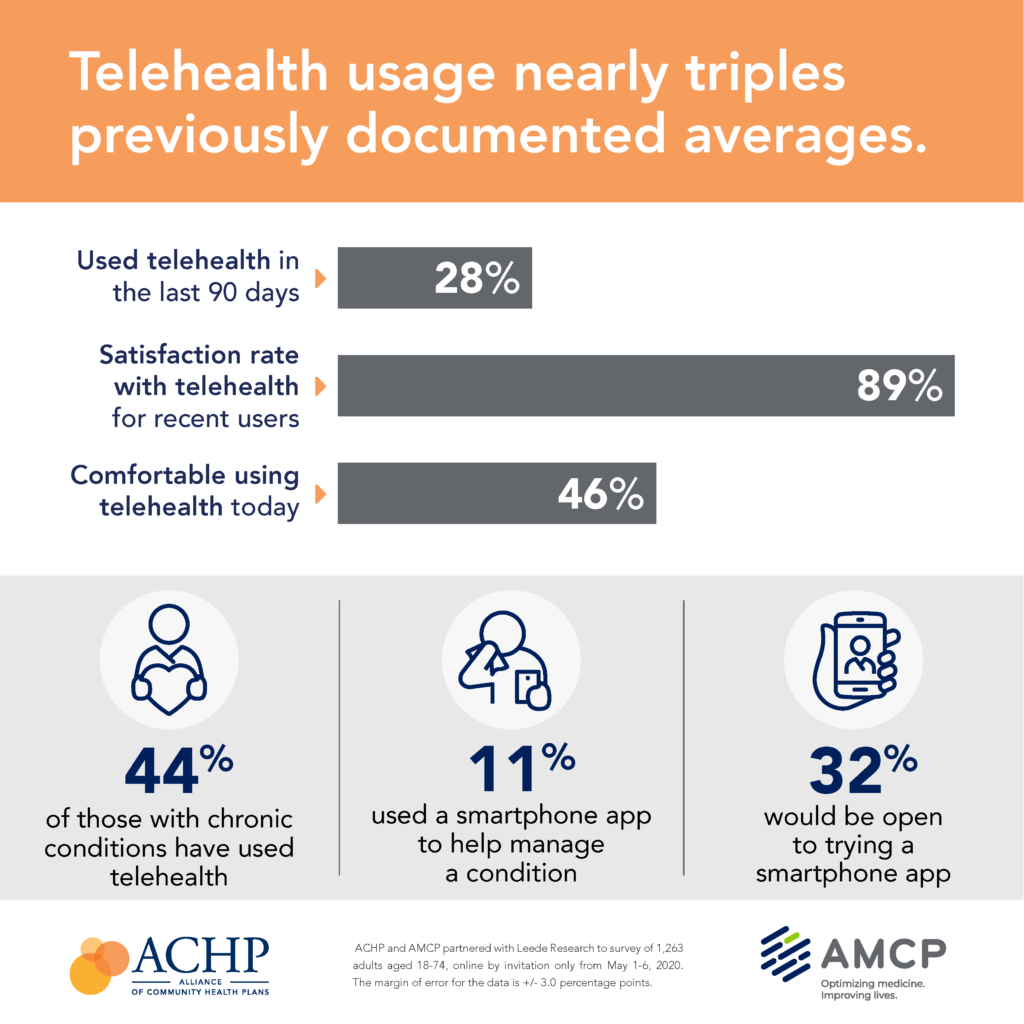
Some one in 4 survey respondents used telehealth in the past 3 months (about the first 90 days of the pandemic), with a vast majority of people satisfied with their virtual healthcare visit. One-half of people said they were comfortable using the technology, shown in the third graphic from the ACHP/AMCP survey.
Health Populi’s Hot Points: It’s interesting to note that one of the investors in this round of Amwell financing was Takeda, the biopharmaceutical company.
As the Chief Digital & Information Office of Takeda, Karl Hick, said in the deal’s press release, “Patient journeys will be transformed through new settings of care as we emerge from COVID-19. Amwell has developed a highly scalable and agile technology platform that we believe can directly improve patient access and outcomes.”
Through and after the pandemic, telehealth will continue gains respect and acceptance as an integral “front-door” for patient health care. Telehealth will blur into the health/care ecosystem and become part of patients’ experience the way we saw “e-business” blend into “just” doing business. Think of this as omnichannel health care — as ecommerce is gaining consumers’ share of dollar in the pandemic in an omnichannel retail world that’s been dramatically disrupted and, now, being re-shaped, by COVID-19.
We can expect telehealth to be that front door for many aspects of patient care — especially mental and behavioral health, care for people managing chronic conditions, and patient life-flows that can be done via self-care at home — the new hub for health as patients become increasingly mindful of health and virus risks, and ever more demanding for convenience wearing their hats as payors.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...