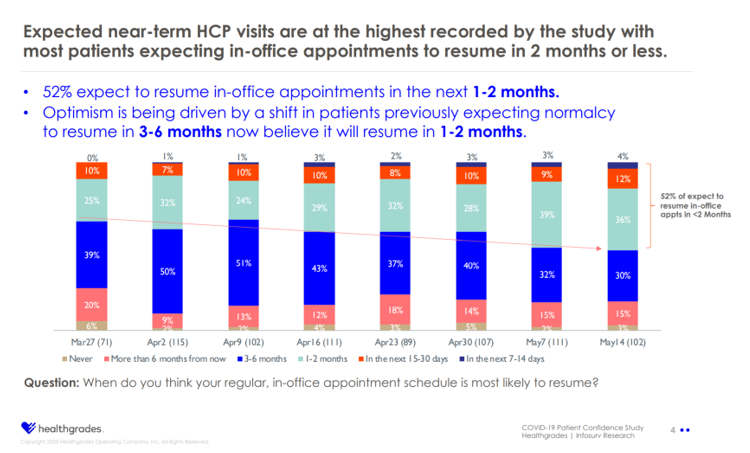
 By May 14th, 2020, one-half of consumers in the U.S. expected they would schedule a medical appointment in the next two months.
By May 14th, 2020, one-half of consumers in the U.S. expected they would schedule a medical appointment in the next two months.
“As the country emerges from COVID-19, we’re watching consumer confidence shift back to where it was prior to the onset of this crisis,” noted Dr. Brad Bowman, Chief Medical Office at Healthgrades.
The company published the COVID-19 Patient Confidence Study, a survey launched in late March. Since the first poll was conducted on March 27th, Healthgrades has conducted the study weekly among 200 patients age 18 and over to gauge peoples’ “confidence” in making typical health care decisions through the pandemic. This post summarizes the study results published as of 21st May 2020, assessing eight weeks of health consumers’ behaviors and perceptions during two months in the COVID-19 era.
 By mid-May, consumers’ expected visits to health care providers reached the highest level since the first poll in the Healthgrades study. At the same time, patients’ Healthgrades found the lowest percentage of patients delaying discussing a condition with a health care provider since the start of the research in late March.
By mid-May, consumers’ expected visits to health care providers reached the highest level since the first poll in the Healthgrades study. At the same time, patients’ Healthgrades found the lowest percentage of patients delaying discussing a condition with a health care provider since the start of the research in late March.
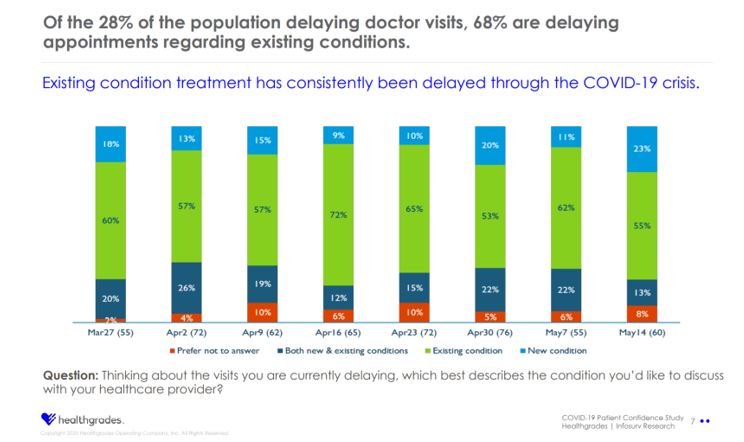
Over one in four patients did delay a visit to a doctor; two-thirds of these patients delayed an appointment regarding an existing condition, shown in the second bar chart. Healthgrades notes that existing condition treatment has consistently been delayed through the coronavirus pandemic.
On the up-side, patients have grown more comfortable visiting a primary care provider by mid-May, and patients’ interest in seeing a specialist also rebounded with 52% of patients comfortable getting an appointment.
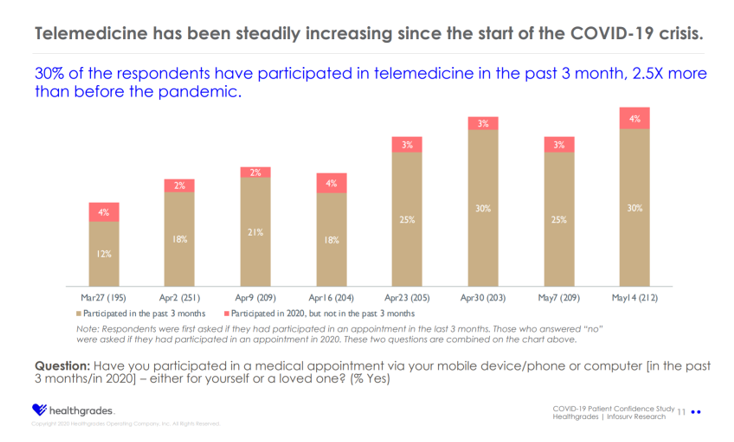
As other studies have found in the pandemic, telehealth has been a novel and welcome work-flow for both patients and clinicians, both sides seeking to manage risks of exposure to the coronavirus.
One-third of consumers had participated in a telemedicine visit in the past three months looking back from 14th May, the third chart illustrates. This telemedicine volume was 2.5 times more than before the pandemic emerged. In this study, “telemedicine” was coined as, “a medical appointment via your mobile device/phone or computer.”
Note that the Healthgrades.com website enables consumers to search among over 400,000 providers that could offer a telehealth appointment.
 Health Populi’s Hot Points: While some consumers across the U.S. are keen to “get on with ‘normal’ life” now in the re-opening of local economies throughout the country, many consumers are wary with concerns about a re-emergence of the COVID-19 virus in the autumn-into-winter season, and potential for the “flattened curves” to spike upward.
Health Populi’s Hot Points: While some consumers across the U.S. are keen to “get on with ‘normal’ life” now in the re-opening of local economies throughout the country, many consumers are wary with concerns about a re-emergence of the COVID-19 virus in the autumn-into-winter season, and potential for the “flattened curves” to spike upward.
We see segments of folks ranging from the FOMO “fear of missing out” people congregating in swimming pools without masks, up close and personal, over the Memorial Day weekend; and, millions of others facing “FOLH” — “fear of leaving home,” with the angst of quarantine and risk-managing concerns of keeping the coronavirus away.
That’s the telehealth opportunity, and especially for people postponing care who have been dealing with chronic medical conditions since March but many avoiding seeking medical care.
In the second chart, above, we learned that, of the 28% of people delaying visits to doctors, two-thirds delayed appointments for pre-existing conditions.
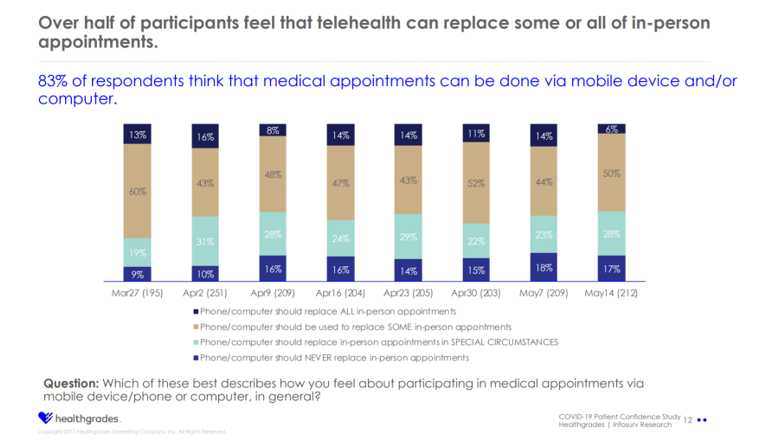
 Looking now at the last bar chart, the overall statistic is that one-half of consumers believe telehealth can replace some or all in-person medical appointments.
Looking now at the last bar chart, the overall statistic is that one-half of consumers believe telehealth can replace some or all in-person medical appointments.
What about the other half of consumers who do not believe in virtual visits for their care? Here’s where we must get smarter about patients’ wants, values, and life-flows to meet folks “where they are.”
What are the barriers and beliefs about telehealth that could limit its adoption by people managing chronic conditions? The obstacles can range across many issues — language, social mores, access to technology (whether a smartphone/hardware or connectivity), digital literacy, financial (payment or insurance barriers), or simply….a human touch that a patient may not perceive in a digital experience.
Call on the empathic UX designers, the ethnographic researchers, the health economists, the case managers! And remember the sage advice from one of my favorite classic JAMA essays: “Value-based payment requires valuing what matters to patients.”




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...