 Today kicks off the first all-virtual conference of the ATA, the American Telemedicine Association. ATA’s CEO Ann Mond Johnson and team turned on a dime over the past few months, migrating the already-planned live conference scheduled in early May to this week, all online.
Today kicks off the first all-virtual conference of the ATA, the American Telemedicine Association. ATA’s CEO Ann Mond Johnson and team turned on a dime over the past few months, migrating the already-planned live conference scheduled in early May to this week, all online.
I’ll be midwifing a panel this afternoon at 440 pm Eastern time, initially focused on how health care can garner patient loyalty. That theme was given to us in the fourth quarter of 2019, when initial planning for ATA 2020 had begun.
What a difference a few months make. Not only has ATA pivoted to an all-virtual platform, but our panel participants met up a few weeks ago and we’ve updated our theme for our brainstorm. It’s now called, “Onward Together: Prioritizing Equality, Safety, Trust, and Partnership in All Care.”
Our panel includes Adrienne Boissy, MD, Chief of Patient Experience at The Cleveland Clinic; Grace Cordovano, PhD, Enlightening Results; Joseph DeVivo, CEO of InTouch Health (recently acquired by Teladoc); and Abner Mason, CEO and Founder of ConsejoSano.
 I’ll set the context for our discussion with a few key data points describing consumers-patients-caregivers being re-shaped through the COVID-19 pandemic. These elements all impact our perceptions of safety, trust, access, equity, and empowerment for health care.
I’ll set the context for our discussion with a few key data points describing consumers-patients-caregivers being re-shaped through the COVID-19 pandemic. These elements all impact our perceptions of safety, trust, access, equity, and empowerment for health care.
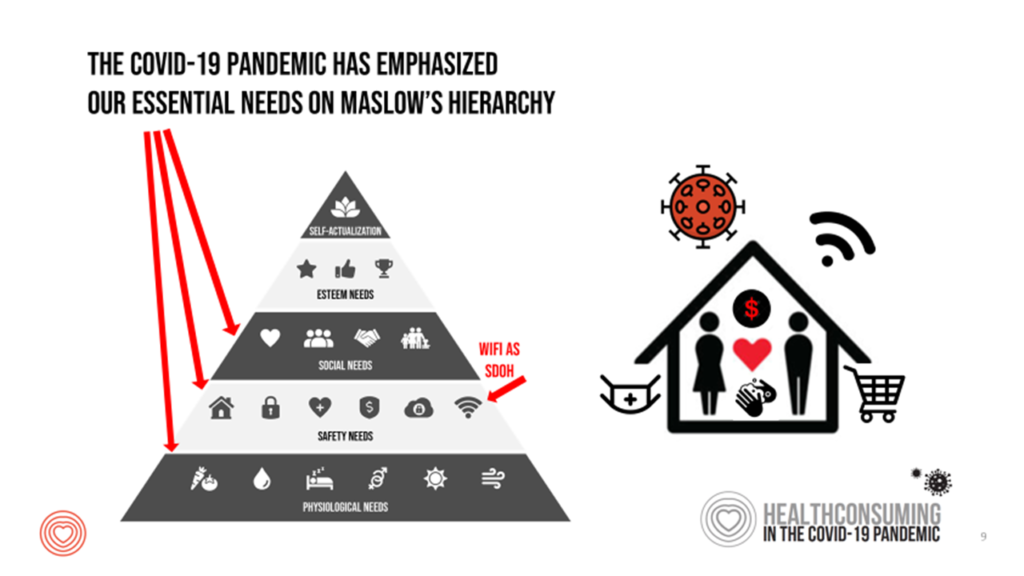
My over-arching theme for COVID-era health consumers is that our personal Maslow’s Hierarchies of Needs have pushed all of us down to the basic essentials of physiological, safety and social needs.
How many of us felt really great scoring toilet tissue and hand sanitizer in February and March, 2020? Nielsen’s consumer retail work on how people hacked their pandemic pantries pointed this out as the slope of the U.S. coronavirus case curve was sharply increasing and grocery store shelves emptied out, supply chains quickly re-orienting.
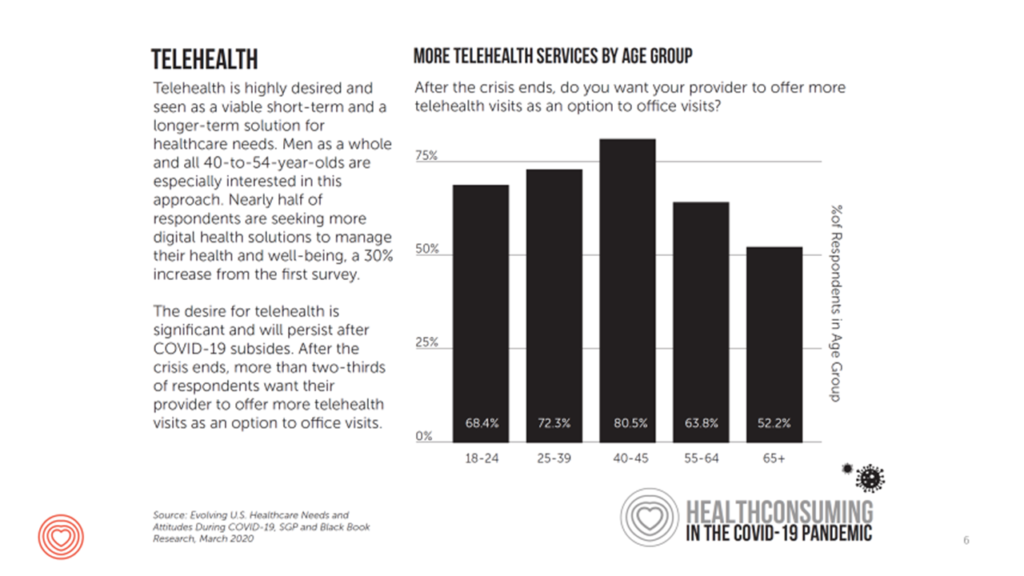 Part of that physiological and safety need drove millions of U.S. patients toward telehealth — the focus of the ATA conference all week long. This is one of the bright spots of the COVID-19 pandemic in the U.S. (and indeed, in countries already impacted by the crisis).
Part of that physiological and safety need drove millions of U.S. patients toward telehealth — the focus of the ATA conference all week long. This is one of the bright spots of the COVID-19 pandemic in the U.S. (and indeed, in countries already impacted by the crisis).
As the third chart illustrates (which I’ll use in my intro today), as early as March 2020, patients 65 years of age and older in the U.S. wanted their health care providers to offer more virtual care services as an option to in-person office visits.
To bolster this telehealth-supportive moment, last week, Dr. Joseph Kvedar, President of the ATA, testified to a Senate HELP Committee on how telehealth has boosted health care delivery and safety during the pandemic. That committee represented a bipartisan group of legislators thus far supportive of telehealth; they will be considering the range of issues to resolve post-pandemic, from payment parity to regulation, licensure, and access to broadband connectivity.
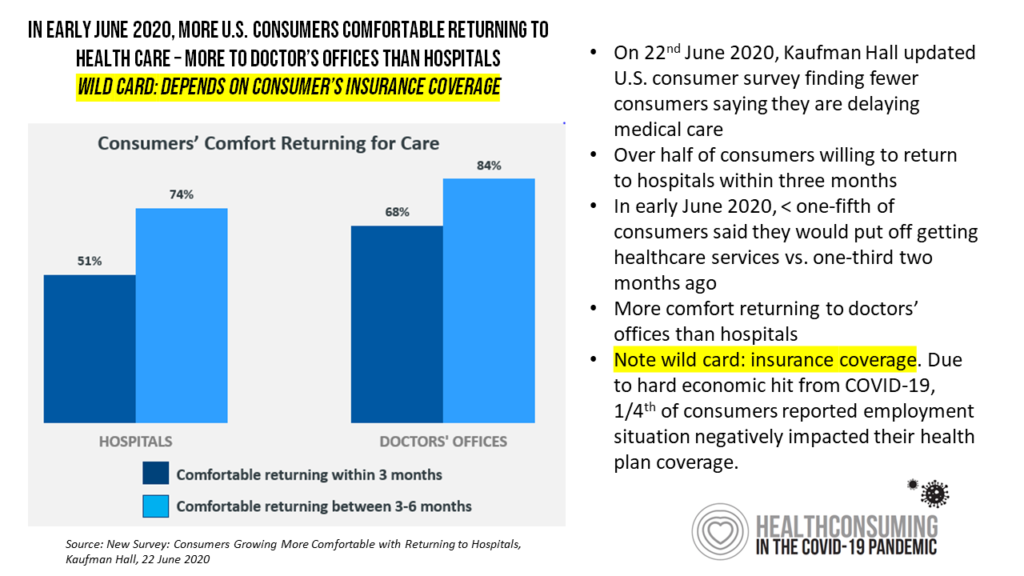 Given the virtual format of the ATA conference and the need for me to submit content to the conference two weeks ago, I have an update to share here with a new, encouraging data point from Kaufman Hall’s June 2020 consumer research. This is shown in the last slide with the blue bars.
Given the virtual format of the ATA conference and the need for me to submit content to the conference two weeks ago, I have an update to share here with a new, encouraging data point from Kaufman Hall’s June 2020 consumer research. This is shown in the last slide with the blue bars.
By early June, more consumers were planning to return to doctors’ offices and hospitals within three to six months from June — more open to physician offices than hospitals, but a promising opening up to scheduling appointments in the health care system.
The limiting factor — or wild card, as Kaufman Hall put it in their blog today — is whether the consumer-patient had health insurance. With the great lockdown, the U.S. economy shed millions of jobs — many tied to health insurance coverage. Those patients without health plan coverage would be less likely to return to medical care settings, as many as 1 in 4 U.S. consumers.
In the U.S., a person’s health care access is largely tied to their employment status, and further, whether that is a large employer (more likely to provide health insurance) than a small company. So, access to telehealth in America isn’t just a “build it and they (patients) will come” scenario. We must be mindful that an on-ramp to telehealth is access (via health insurance or coverage in another way), and of course, WiFi or other sort of connectivity – a basic social determinant of health for survival in the pandemic. Indeed, cost of health care has been a factor in some people not seeking health care in the age of COVID, and lack of connectivity a barrier to returning to school-from-home, tele-work, and accessing telehealth as well.
I know my panel-team and I are all looking forward to moving Onward, Together, this afternoon — and ongoing…





 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...