Health care providers stood up virtual health care services with lightning speed as the coronavirus pandemic emerged in the U.S. Telehealth and its various flavors enabled both patients and providers to manage the risk of contracting the virus, especially at a time when little was known about the nature of transmission, treatment and prevention — except for washing hands, covering one’s face, and isolating when showing symptoms.
In Electronic Consultations (eConsults): A Triple Win for Patients, Clinicians, and Payers, the Milbank Memorial Fund explores the evidence supporting the growth of asynchronous electronic consultation encounters between patients and clinicians.
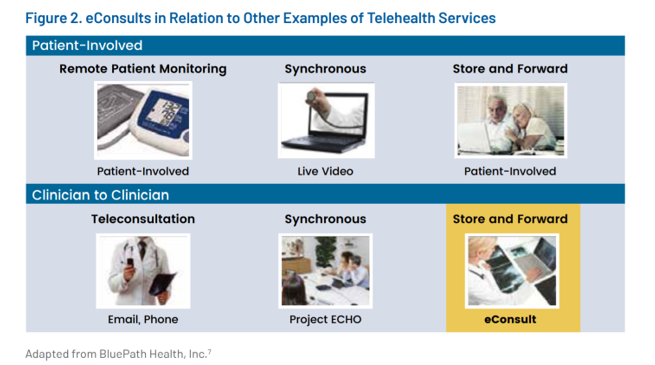 Note that this report focuses on asynchronous meet-ups, distinguished from other kinds of telehealth services shown in the first graphic.
Note that this report focuses on asynchronous meet-ups, distinguished from other kinds of telehealth services shown in the first graphic.
eConsults are defined as, “directed communication between providers over a secure electronic medium, that involves sharing of patient-specific information and discussing clarification or guidance regarding clinical care,” Milbank describes from a seminal research paper led by Dr. Varsha Vimalananda.
As such, eConsults are distinguished from patient-facing telehealth applications such as remote health monitoring. These visits are strictly those conducted between clinicians, specialists and other licensed professionals sharing and discussing patient information.
 Key findings were that eConsults:
Key findings were that eConsults:
- Increased patients’ access to health care services while driving more efficiency in the health care resource use
- Were a safe, cost-effective approach to care delivery
- Drove patient and clinician satisfaction
- Had significant variation in outcomes
- Can involve complex, costly, and time-consuming implementation, and,
- Reimbursement models depend on health care delivery system design.
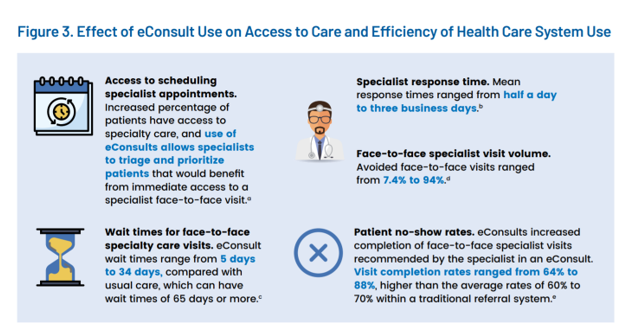
The second chart illustrates several areas of efficiency that eConsults manifested including faster access to specialist opinions, better access to specialists, and reduced patient no-shows for visits to clinicians.
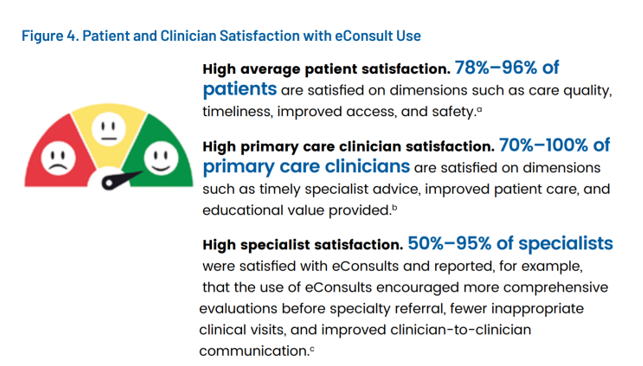
eConsults also drove greater clinician and patient satisfaction — for the latter, especially interesting because these were not face-to-face real-time (synchronous) encounters.
The third chart presents various ranges of satisfaction for patients, primary care providers, and specialists.
Milbank concluded that there is strong support for the use of eConsults to scale health care without sacrificing quality, patient, or clinician satisfaction. The report also suggests that expanding eConsults could lower overall health care costs both in terms of the encounter time as well as reducing patient travel time and duplication of tests and procedures.
The paper gathered evidence from interviews with leaders at eConsult programs, along with reviews of 36 studies and four other reviews of many studies (eg., meta-analyses).
Health Populi’s Hot Points: The Milbank Memorial Fund subtitled this report, “a triple win for patients, clinicians, and payers.”
The report included several data points relevant to payers and health care costs: for example, eConsults were found to reduce the total cost of care from 36% to as high as 83%. When considering costs saved in virtual care programs, in general, it’s important to think like an economist, inventorying the broad range of items that are cost-creating. These can include labor costs, time costs for both clinicians and patients (including both travel and time off from work), procedures (including savings conserved avoiding duplication or re-testing), facility charges, and others.
Among key lessons learned from the pandemic, the virtues of virtual care will be longstanding. Let’s listen and take heed from them in re-imagining a more resilient, sustainable health care system for U.S. health citizens and providers alike.




 Thank you,
Thank you,  As a proud Big Ten alum, I'm thrilled to be invited to
As a proud Big Ten alum, I'm thrilled to be invited to  I was invited to be a Judge for the upcoming CES 2025 Innovation Awards in the category of digital health and connected fitness. So grateful to be part of this annual effort to identify the best in consumer-facing health solutions for self-care, condition management, and family well-being. Thank you, CTA!
I was invited to be a Judge for the upcoming CES 2025 Innovation Awards in the category of digital health and connected fitness. So grateful to be part of this annual effort to identify the best in consumer-facing health solutions for self-care, condition management, and family well-being. Thank you, CTA!