The coronavirus pandemic has re-shaped patients into consumers, concerned about managing the risk of contracting the virus, millions of people experiencing months of sheltering, working, learning, and cooking at home.
Combine these new life-flows with conflicting information about the nature, severity, and life-span of COVID-19:
- From three levels of government leaders: The President and the Executive Branch at the Federal Level, Governors of States, and Mayors of cities;
- Public health agencies, especially the U.S. Centers for Disease Control and the World Health Organization;
- Mass media; and,
- Social media.
Re-entering life in the “next normal” requires a large dose of trust, addressed in COVID-19 and the New Consumerism: the Critical Importance of Humanity and Building Trust, from Press Ganey.
[FYI, Press Ganey, a leading health care patient experience organization, has created an impressive library of resources addressing the pandemic, linked here.]
How do health care providers build trust? Press Ganey asks.
“By embracing high reliability in the safety, technical quality, coordination, and experience of care and nurturing an engaged workforce that is committed to zero harm and a holistic concept of excellence,” PG answers.
But in the thick of the pandemic, patient trust is being tested, the report sets out.
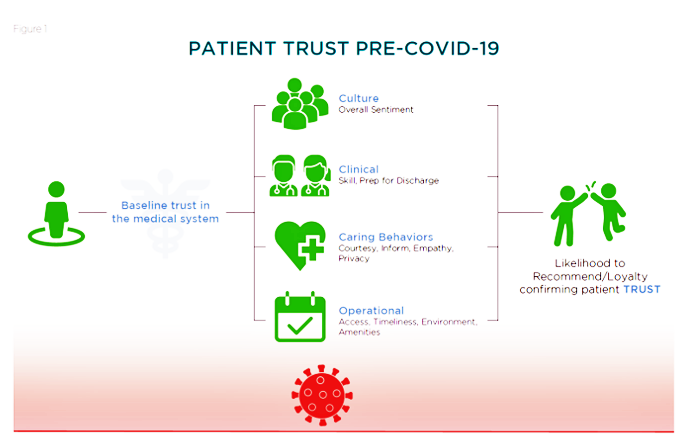
The first diagram portrays patient trust before the pandemic. Pre-COVID-19, the consumer had a trust baseline which Press Ganey shows was further shaped by the person’s experience in the health system. That re-shaping happened through experiences of the hospital’s clinical functions, caring behaviors, operations, and overall culture. If these four experience-flows were positive, the patient would be discharged from hospital more likely to recommend the provider to friends, family, and social networks…generating trust.
The center column illustrates that care providers – doctors, nurses, allied health professionals, the parking lot attendants and cafeteria staff — all communicate signals of trust. Thus, Press Ganey asserts, “patients’ trust in their health care is intertwined with caregivers’ trust in their organizations.”
That’s the pre-pandemic consumer trust scenario. Now, let’s time travel to “now:” “COVID-19 Raises the Bar,” Press Ganey observes. Consumer trust in health care is challenged in two ways:
- The virus has engendered a deep sense of vulnerability for each of us, especially as the disease is not well understood, with treatments and a vaccine still elusive; and,
- The “familiar cues” that patients are in good hands are unfamiliar. Providers masks and in protective gear, waiting in an automobile or physically-distanced queue to gain access to a doctor’s office, or convening with a doctor via a virtual telehealth visit or encrypted email are all new-new life-flows for a health consumer.
 We may admire care providers, Press Ganey notes, “but admiring caregivers does not mean patients trust that their needs will be met safely and well.”
We may admire care providers, Press Ganey notes, “but admiring caregivers does not mean patients trust that their needs will be met safely and well.”
To gain insights on health consumer trust, the company analyzed millions of patient encounters among people who had been hospital inpatients, been admitted to emergency departments, seen clinicians in ambulatory care practices, and experienced telemedicine visits over six weeks between March and April 2020.
Press Ganey uncovered a roster of ways that eroded patient trust in these encounters: perceived lack of cleanliness, delays/waits, process failures, and lack of proficiency in procedures, among them.
The bottom line in this is that to build trust, health care providers should deliver care “humane at its core,” in the words of Press Ganey: compassionate, coordinated, and safe.
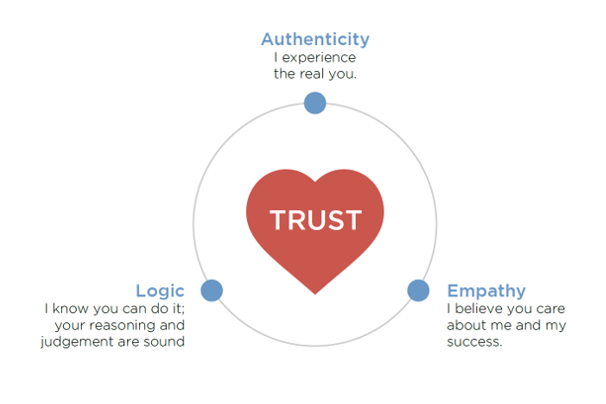
 The heart-triangle diagram conveys Press Ganey’s simple model for inspiring trust, built on three factors:
The heart-triangle diagram conveys Press Ganey’s simple model for inspiring trust, built on three factors:
- Authenticity = “I experience the real you”
- Logic = “I know you can do it: your reasoning and judgement are sound,” and
- Empathy = “I believe you care about me and my success.
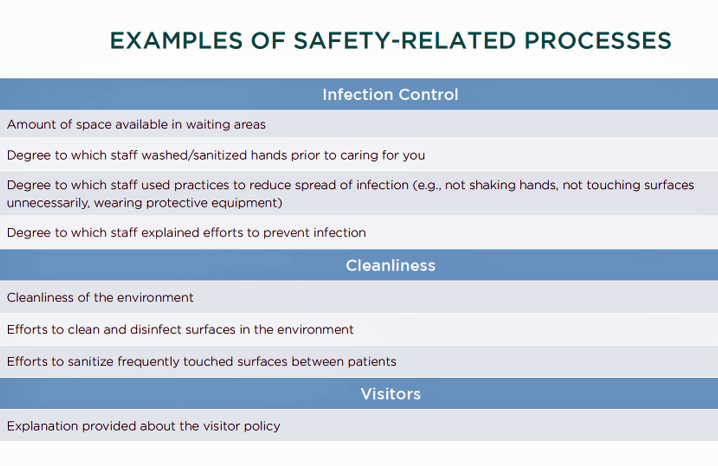
Re-opening health care in this next-normal requires addressing consumers’ real fears about the risks of contracting the coronavirus. Providers can be transparent about measures and metrics for safety, such as public reporting of provider transmission rates, limiting use of waiting areas by patients or family (thus, the waiting-in-car scenario), public reporting of PPE supplies, video examples of cleaning processes, and videos of physician leaders discussing health risks and procedures on the hospital’s website and in social media.
COVID-19 indeed raised the bar for trust between patients and health care providers. Both sides of this caregiving equation, the demand and supply sides, have rational fears about risks of the virus, and concerns for lives and livelihoods as the U.S. strives to get through the pandemic. Trust is the social capital required for us to come together for health care, for individuals, communities, and the individual heroic caregivers committed to the art and science of healing.
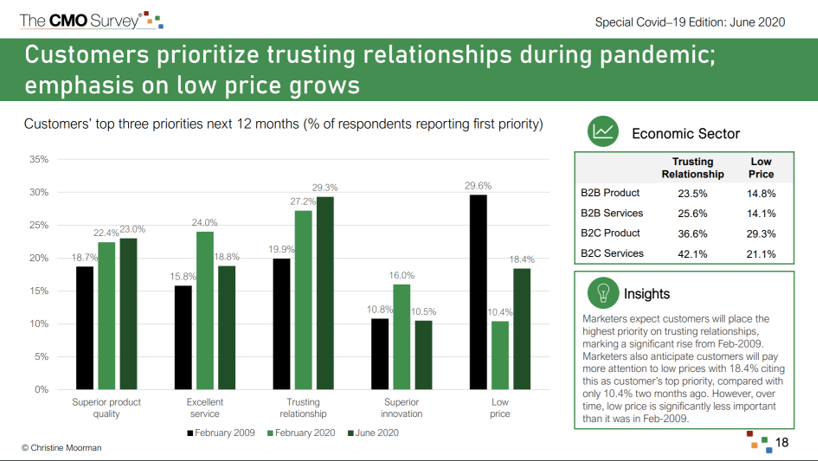 Health Populi’s Hot Points: The CMO Survey, conducted by the Duke Fuqua School of Business in collaboration with Deloitte and the American Marketing Association, found that consumers place trust very high as a result of the pandemic, shown in the chart from the study.
Health Populi’s Hot Points: The CMO Survey, conducted by the Duke Fuqua School of Business in collaboration with Deloitte and the American Marketing Association, found that consumers place trust very high as a result of the pandemic, shown in the chart from the study.
Note the differences across the four economic sectors on which the research focused: B2C services garnered the highest proportion of customers citing a trusting relationship would be a priority in the next 12 months.
Trusting relationships as a top-three factor grew by 50% over the proportion of people who cited in in February 2009 at the throes of the Great Recession.
Health citizens in the U.S. differ from those in other countries in the developed world in many ways — but in health care, most notably as key payors in the transaction of getting medical care. In the COVID-19 pandemic, cost has played a role in patients-as-consumers seeking care…or not.
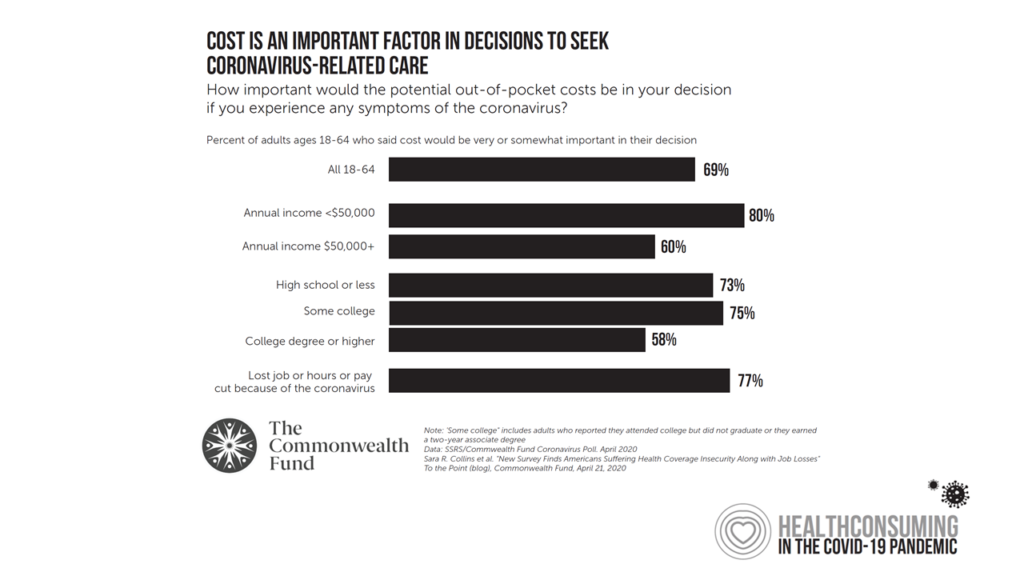 The Commonwealth Fund found that, in the midst of the pandemic and concerns about physical risks, health consumers also had concerns about “fiscal” risks — the cost of care, shown in this chart which displays data from the Fund’s survey conducted in April 2020.
The Commonwealth Fund found that, in the midst of the pandemic and concerns about physical risks, health consumers also had concerns about “fiscal” risks — the cost of care, shown in this chart which displays data from the Fund’s survey conducted in April 2020.
Most Americans, regardless of income, were concerned about costs for COVID-19 related care. Needless to say, the majority of people who had lost a job or had hours cut due to the pandemic were even more concerned about the cost of coronavirus care.
The economic recession in the U.S. in 2020 is quite different from the Great Recession of 2008: this national financial decline has hit Main Street harder than Wall Street, women harder than men, and people of color more acutely. As hospitals and health systems work to gain patient trust, the health care financial pillar will also play a major role in restoring patient confidence in returning to the traditional healthcare system.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...