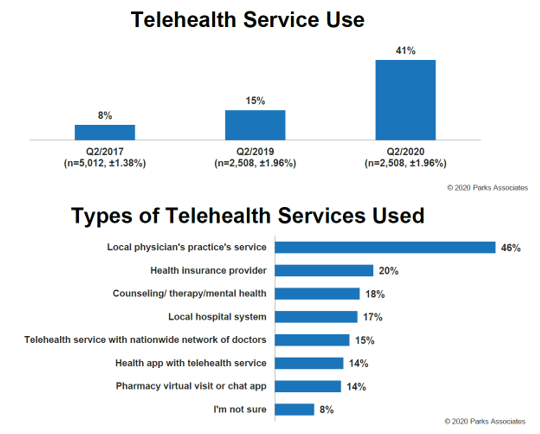
In the U.S., the use of telehealth services tripled in the past year, as healthcare providers limited patients from in-person visits for care and patients sought to avoid exposure to the coronavirus in medical settings.
With this alignment of virtual care supply-and-demand, it is like telehealth will see “permanent usage increases,” according to Parks Associates’ survey report, COVID-19 – Impact on Telehealth Use and Perspectives.
 Parks Associates fielded this study the second half of May 2020, surveying 5,008 heads-of-broadband households balancing the sample of respondents for age, gender, income, and education.
Parks Associates fielded this study the second half of May 2020, surveying 5,008 heads-of-broadband households balancing the sample of respondents for age, gender, income, and education.
The report reminds us for context that at the time the poll was conducted, 40 million Americans were unemployed, New York’s COVID cases were on the decline, and states had begun to lift some lockdown measures.
What’s new in this fast-pivot to virtual care is the type of telehealth services used, shown in the first chart from the report. One-half of patients accessed a local physician’s practice service in the second quarter of 2020. This was a major shift in telehealth “service channel,” Parks points out, from accessing a platform from a company specializing in telehealth with a nationwide network of doctors to using a local provider’s service.
Statistically, this was an inverse-shift:
- In the previous year, the second quarter of 2019, 15% of telehealth encounters happened through a local physician’s practice, versus 46% in Q2 2020; and,
- In the second quarter of 2020, 41% of telehealth occurred through a telehealth company with a nationwide network of doctors, versus 13% in Q2 2020.
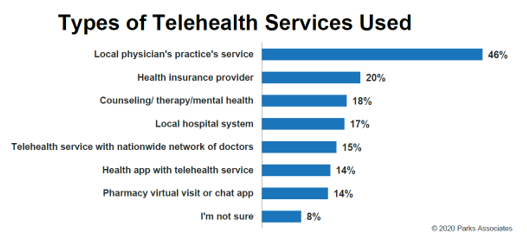
 The second chart compares health consumers’ perceptions of telehealth concepts, whether locally-sourced virtual care services through a physician or a hospital system, or via a national platform. More people who experienced COVID-19 symptoms uniformly favored all approaches compared with consumers who had no symptoms from the virus. But even so, roughly 50% of people experiencing no symptoms still found the various telehealth concepts attractive.
The second chart compares health consumers’ perceptions of telehealth concepts, whether locally-sourced virtual care services through a physician or a hospital system, or via a national platform. More people who experienced COVID-19 symptoms uniformly favored all approaches compared with consumers who had no symptoms from the virus. But even so, roughly 50% of people experiencing no symptoms still found the various telehealth concepts attractive.
Slightly more consumers favored locally-borne virtual care versus a nationwide network. But it’s a relatively small difference, the statistics show.
One of the most compelling telehealth access scenarios in the first months of pandemic will be told by consumers accessing virtual care for teletherapy and counseling. One of the public health hallmarks of the pandemic era has been stress, documented by the American Psychological Association’s Stress in America survey. Use of tele-mental health has been particularly high among younger people (more likely under 44 years old), patients having COVID-19, knowing someone with the coronavirus, and people who had lost their jobs.
Even with this warm reception, by May 2020, consumers’ experiences with telehealth were not uniformly streamlined: one-third of U.S. broadband households tried to use a telehealth service by then, but one-third had technical issues or wait times that compelled people to cancel the visit.
Health Populi’s Hot Points: Familiarity with virtual care breeds demand, based on the Parks Associates study. When patients successfully used a telehealth service, they would likely use it again the next time they are sick or when a child in the household is sick.
There’s an interesting and important nuance in this study which has implications for health systems’ planning beyond the pandemic era: telehealth services increased across all delivery methods — video calls, text messaging and chat, phone calls, alike. The report notes that, “leading telehealth platforms like Teladoc and MDLive offer all three modalities, both direct-to-consumers and through their B2B arrangements with payers and providers.”
This speaks to the evolving role of hospitals in their local markets, and how patients-as-health-consumers will want to access health care “now” and after the pandemic. It’s an omnichannel landscape for care, from the home and phone to community hubs in pharmacies and grocery stores, to doctor’s offices, health systems, and urban “Pill Hill” academic medical centers.
What will enable this vision is a networked health care system where data can flow seamlessly between these different health care touchpoints. Note in the “Appeal of Telehealth Approaches” diagram above that most patients would look to a telehealth program that would allow them to share data form the medical devices in their home, and to share data in mobile health apps from the phone to the health system. That further enhances patient experience, and further enables the patient to self-manage care at home where it’s safe, hygienic, and risk-managed.
FYI, on 1st – 3rd September 2020, Parks Associates will be convening a Connected Health Summit, focused on consumer engagement and innovation.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...