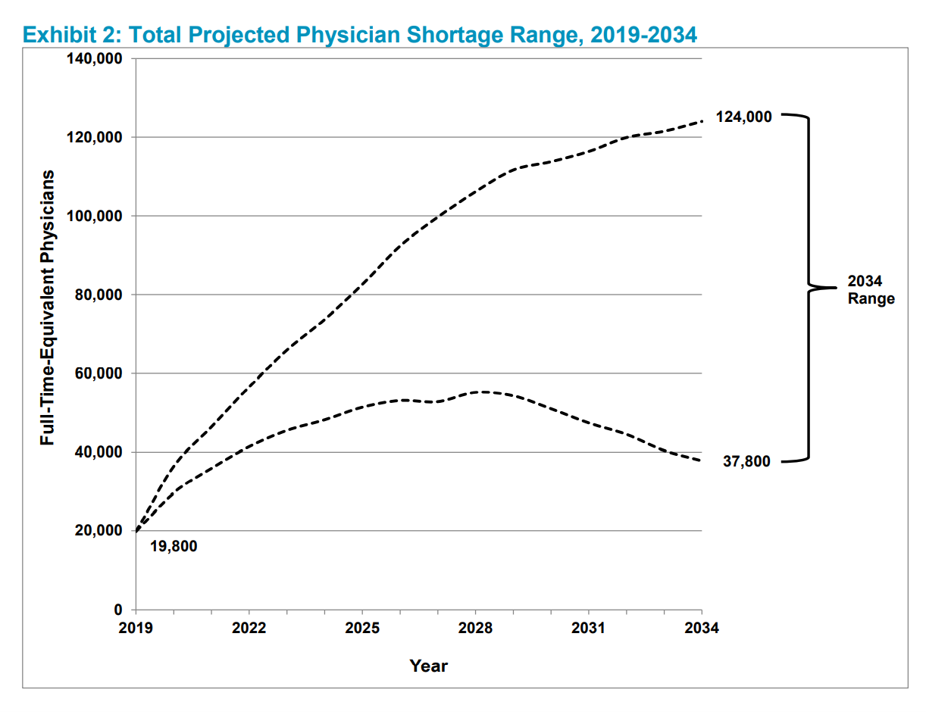
The U.S. will be short as many as 124,000 physicians in 2034, according to The Complexities of Physician Supply and Demand Projections From 2019 to 2034 from the Association of American Medical Colleges (AAMC).
 Published 11th June 2021, the report was prepared by IHS Markit Ltd. and updates AAMC’s six previous annual reports on physician workforce projections.
Published 11th June 2021, the report was prepared by IHS Markit Ltd. and updates AAMC’s six previous annual reports on physician workforce projections.
In this year’s projections, AAMC considers the long-term implications of the COVID-19 pandemic on physician supply, new to this report. Another timely feature in the 2021 study is the Health Care Utilization Equity Scenario which provides a baseline looking at inequities in access to care.
What’s underneath the sobering forecast is a combination of aging patients and aging doctors.
“Demographics continue to be the primary driver of increasing (physician) demand from 2019 to 2034,” AAMC asserts.
On the patient-health citizen side of the demand curve is this stunning chasm: in the U.S.,
- The population under 18 years of age is expected to grow by 5.6% to 2034
- The population age 65 years and older is forecasted to increase by 42.4%.
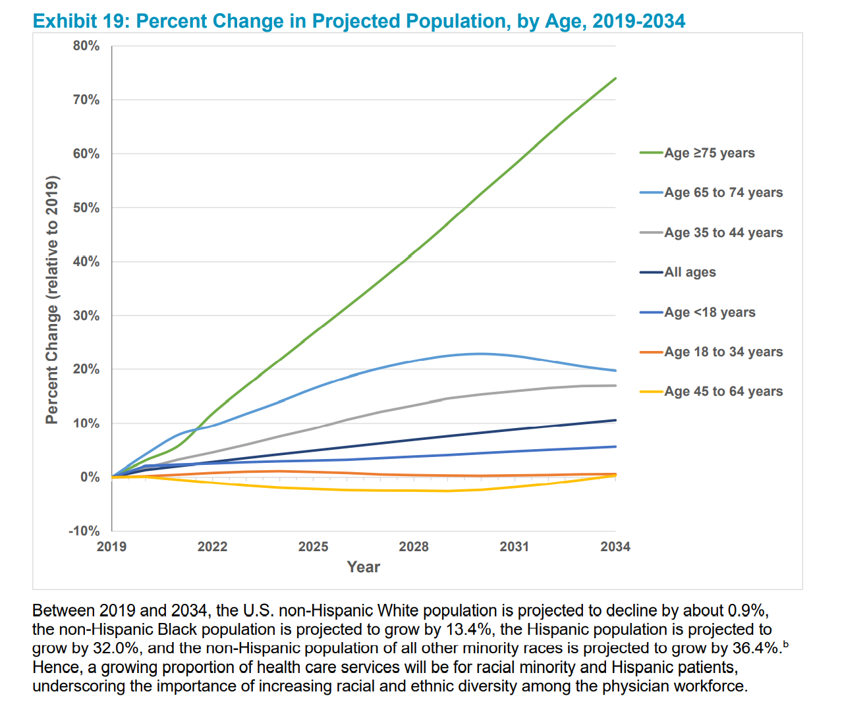 And then within that 65-and-over cohort are the older-aging folks 75 years of age and over — a group projected to grow in size by 74.0% to 2034.
And then within that 65-and-over cohort are the older-aging folks 75 years of age and over — a group projected to grow in size by 74.0% to 2034.
That means small growth expected for pediatrics and specialties that serve the young, and huge growth expectations for clinicians focused on providing care to older and older health citizens.
This Big Trend converges with another aging demographic: that of U.S. physicians themselves.
In 2017, HealthLeaders published an essay titled, “The U.S. physician workforce is getting old, fast.”
The article quoted a study from Merritt Hawkins, noting that 43% of physicians in the U.S. were 55 years old or older.
In addition to aging, the coronavirus pandemic has wreaked havoc on physicians’ anxiety, stress, and depression.
A Medscape survey found that one in four physicians was considering retiring earlier than planned, due to their experience of the pandemic.
Furthermore, nearly 1 in 5 U.S. clinicians was considering quitting their profession during the COVID-19 pandemic, according to a JAMA Network Open investigation published in April 2021. Another 30% of physicians was considering cutting work hours, further exacerbating the supply-side of physician FTEs.
A Physicians Foundation survey of doctors polled in August 2020 (in the midst of the pandemic) found that 8% of doctors had closed their practice as a result of COVID-19, and another 4% were considering shutting practices down in the next twelve months.
Notwithstanding the wild cards that COVID-19 might present to the forecast scenarios, AAMC believes that the essential drivers of physician supply and demand aren’t changing all that dramatically. Demand will outstrip supply, largely due to that patient demographic of more aging people living longer and fewer people being born to balance out the population pyramid.
 Health Populi’s Hot Points: How to mitigate the supply-and-demand gap between growing health citizen needs for care as we age, and a shortage of doctors?
Health Populi’s Hot Points: How to mitigate the supply-and-demand gap between growing health citizen needs for care as we age, and a shortage of doctors?
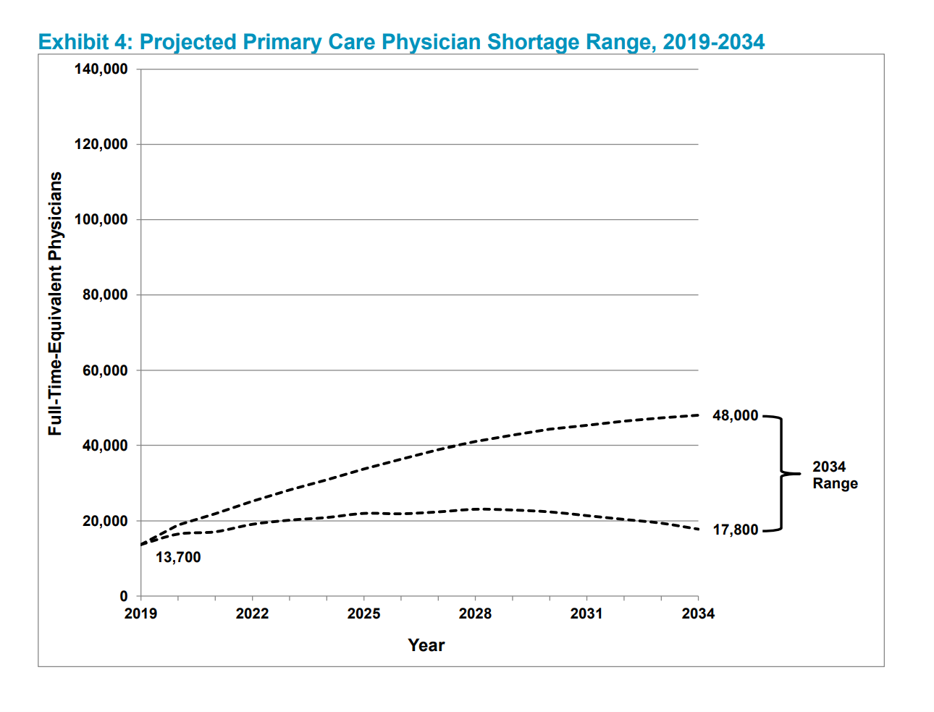
Consider a subset of physician shortage shown here in the third chart — that is the shortage expected for primary care doctors.
The AAMC report’s conclusion offers a portfolio of policy prescriptions to deal with the shortage as played out in the various scenarios.
The “Evolving Care Delivery System Scenario” looks at future health care workflows that use more managed care principles such as shifting more care from specialty physicians to PCPs, applying population health principles, and employing more so-called physician-extender professionals — nurse practitioners, physician assistants, and other licensed staff that are well-trained and can serve patients quite well for primary care, geriatrics, and other services in high demand. Nurses, too, can operate at the top of their license and provide a lot of primary care.
In my own “evolving care” scenario, we’d grow virtual care across the continuum of care, and move much of it to the person’s home. More older people want to age longer at home, and have already begun to engage with telehealth during the pandemic along with taking advantage of retail health channels. This is the sweet spot for, for example, Best Buy Health, and no doubt Amazon Care can expand across various siloes to bundle up care for aging at home.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...