 It’s de rigueur for any organization marketing a product or service in health care to be “patient-centered” these days. “Patient engagement” and “health engagement” are phrases found on health conference agendas, whether pitching to attendees in pharma and life sciences, health IT, health insurance, or healthcare (to hospitals and physicians, alike).
It’s de rigueur for any organization marketing a product or service in health care to be “patient-centered” these days. “Patient engagement” and “health engagement” are phrases found on health conference agendas, whether pitching to attendees in pharma and life sciences, health IT, health insurance, or healthcare (to hospitals and physicians, alike).
One paradigm for patient-centricity that’s more mature than most is IMS Health’s Patient Journey construct, which the data-driven company has been talking about since 2012. While the concept focused mainly on pharmaceutical marketing and medication adherence, it’s useful for all industry segments looking to motivate behavior change in health care – a Holy Grail whether looking to sell health insurance, support smoking cessation, or lower BMIs in a targeted group of people tending toward pre-diabetes.
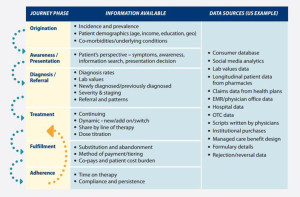
IMS Consulting Group has updated their original work in A new foundation for designing winning brand strategies – The Patient Journey re-envisioned. IMS says the Patient Journey describes “how patients experience a disease or condition from their first awareness of symptoms through all stages of presentation, diagnosis, referral and treatment, fulfillment, monitoring, adherence, and follow ups.” Think of this as the value-chain of patient and provider decisions along a person’s health continuum.
Common challenges faced by health marketers in building and using the Patient Journey are lack of a patient perspective (either due to ignoring it or basing it on physicians’ inaccurate or incomplete perceptions), missing patient affordability issues, and understanding “whys” behind peoples’ health decisions.
What would help to mitigate these problems is using real-world evidence to better understand peoples’ perspectives on their own Patient Journeys. The chart from IMS’s report shows different phases of the Journey, and the kind of information that’s available that can be used to enhance industry’s appreciation for that patient perspective. There’s a growing array of sources for real-world information – from consumer databases and social media analytics to prescription and fulfillment data, among other data.
“It is advisable to start building the Patient Journey with secondary data and use primary research to plug the gaps,” IMS recommends.
Health Populi’s Hot Points: IMS rightly points out that emotional drivers — for both patients and physicians — underpin Patient Journeys. Some of this can be scraped from social conversations between people in social networks. But there’s another source that’s also very useful and authentic: conversations between patients and providers. The relationship between patient and doctor still holds trust. Growing acceptance of Open Notes and other transparency projects that focus on shared decision making between people and their health providers can support better understanding of Patient Journeys for physicians at-financial-risk for delivering outcomes and quality care.
The fine print mentioned about “patient affordability” in building the Journey understanding is not trivial. I recently discussed this here in Health Populi, where consumers bundle financial health into overall health and well-being.
Using real-world data is indeed a key to getting real about the Patient Journey. On that road, organizations employing these new sources of data should make certain to be transparent, clear, and empathetic with patients to ensure the virtuous cycle of trust that can be built between health consumers and industry. Early uses of Big Data culled from third party data brokers in health haven’t always adopted this approach. For more on this important new reality of doing data-driven business in health, my paper, Here’s Looking at You, published by California HealthCare Foundation, speaks to the positive and darker uses of consumer-generated data.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...