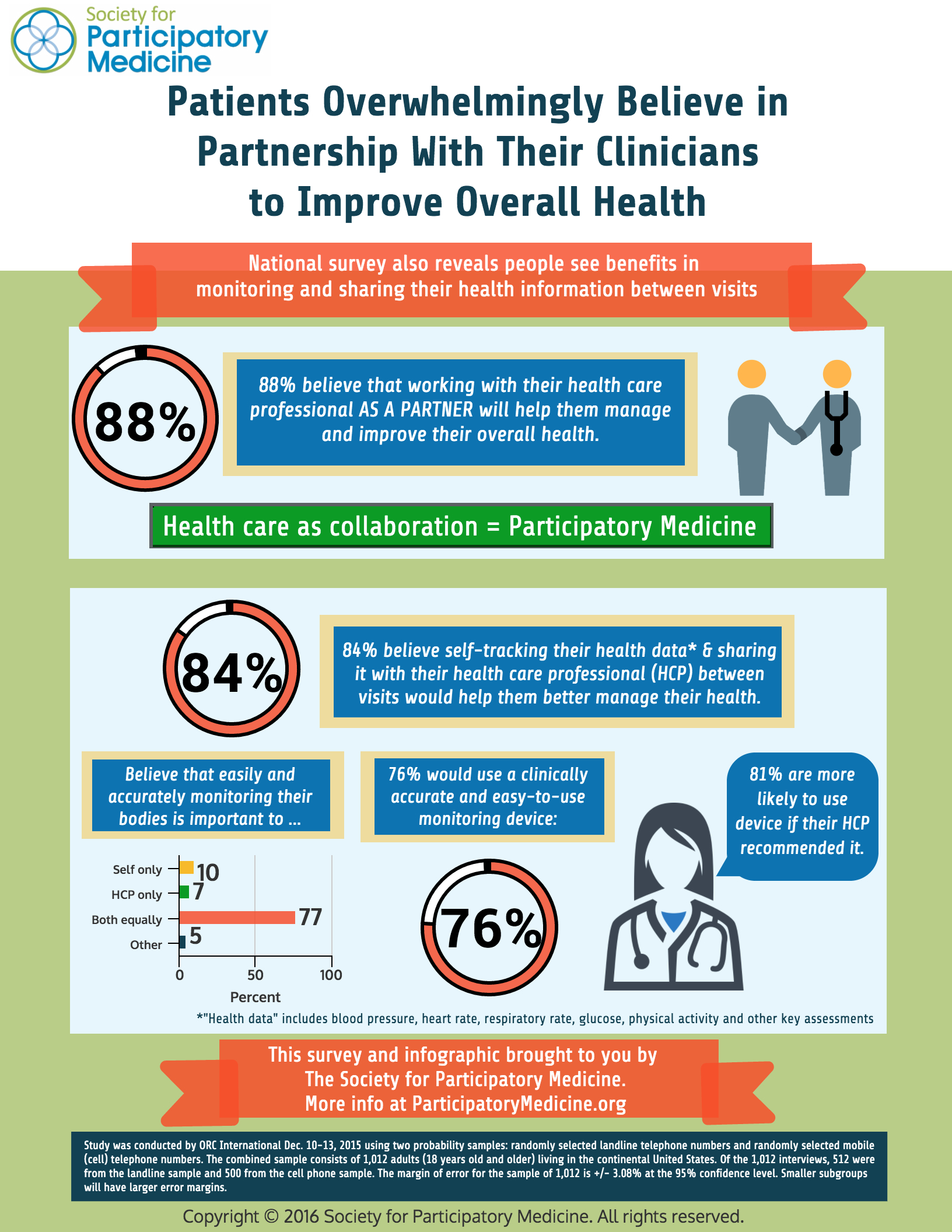
9 in 10 people in the U.S. believe working with their health clinician as a partner will help them better manage their overall health, according to a survey conducted for The Society for Participatory Medicine.
Consumers’ majority call-out for shared decision-making with health care professionals also extends to their self-tracking health data — for example, via activity trackers, digital glucometers for blood sugar, technologies for blood pressure, and food logging apps. 84% of people said that sharing their personal self-tracking health data with clinicians between visits would also help people manage health.
That clinician’s involvement is very important to health consumers for adopting and using a digital tracking device: 81% of people would be more likely to use the device if their health care professional recommended it.
Additional survey results are illustrated on the infographic, shown here.
“Increasingly, patients are actively monitoring their own health data to better self-manage their health and collaborate with their health care professionals,” Dr. Danny Sands, Co-Founder and Chair of the Society said in the organization’s press release on the study.
ORC International polled 2,012 U.S. adults, 18 and over, in December 2015.
Health Populi’s Hot Points: In the post-Recession economy, people have been more inspired by do-it-yourself personal work flows in daily life, from trading stocks and managing finances to arranging airline travel, hotel rooms, and just-in-time car services (read: Lyft and Uber).
So the health consumer’s healthcareDIY muscles are growing, too, enabled especially through the mass adoption of mobile platforms (particularly smartphones), and a growing supply-side of digital health tools.
 The most prevalent digital health tools available in 2016 is the electronic health record, now available in most physician offices. Some 74% of office-based physicians had a certified EHR system in 2014, according to the CDC update published in January 2016 on the adoption of EHRs.
The most prevalent digital health tools available in 2016 is the electronic health record, now available in most physician offices. Some 74% of office-based physicians had a certified EHR system in 2014, according to the CDC update published in January 2016 on the adoption of EHRs.
As the chart illustrates, just over one-third of physicians were electronically sharing patient health information with ambulatory providers and hospitals. Those physicians with EHRs were more like to share patient health information with external providers than physicians who did not have an EHR system. There is significant geographic variation in health data sharing by physicians, with the greatest likelihood nationally occurring in Oregon, Washington, North Dakota, and Massachusetts.
That’s as far as clinicians sharing EHR-stored patient data with other clinicians.
As for clinicians sharing with patients? Now that patients recognize the value of sharing their own patient-generated data with their personal physicians and other clinicians, we’re at the inflection curve of change as patient connect the dots between their personal DIY health/care strategies and their interactions with health care professionals.
A crucial linkage to moving this forward will be the development of digital health tools that seamlessly and enchantingly fit into both patients and health care providers’ work flows (personal for patients, professional/clinical for doctors and nurses). There’s no greater higher calling or need for user-centered design than in patient-centered health.
Note: I sit on the Board of Directors for the Society for Participatory Medicine. Follow the Society on Twitter @S4PM.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...