 For the first time since 1993, expanding life expectancy in the United States has reversed, based on the latest report from the Centers for Disease Control, Mortality in the United States, 2015.
For the first time since 1993, expanding life expectancy in the United States has reversed, based on the latest report from the Centers for Disease Control, Mortality in the United States, 2015.
“The last time U.S. life expectancy at birth declined was in 1993, when it dropped from 75.6 to 75.4, according to World Bank data,” as quoted in the Washington Post.
Life expectancy at birth in 2015 was 78.8 years, a slight fall from 2014 at 78.9 years. The larger decline fell among men, from 76.5 to 76.3 years. For women, life expectancy at birth in 2015 was 81.2, falling from 81.3 in 2014.
The biggest percentage increase in age-adjusted death rates by race/ethnicity was among non-Hispanic white females (1.6%), followed by non-Hispanic black males (0.9%) and non-Hispanic white males (1.0%).
The chart shows death rates for the leading causes of death in 2015 by disease/condition. Note the expanding green bars in the chart, representing the increasing death rates between 2014 and 2015 for those conditions: heart disease, respiratory diseases, injuries, stroke, diabetes, kidney disease, suicide, and Alzheimer’s.
Health Populi’s Hot Points: The list of conditions which underlie Americans’ drop in life expectancy are largely attributable to lifestyle changes, like healthy food and nutrition choices, increasing physical activity, quitting smoking, and de-stressing. “Easy to say, hard to do,” the normal person living in America would and could say.
 Health policies aren’t just healthcare policies. They’re baked into other public policy areas, such as:
Health policies aren’t just healthcare policies. They’re baked into other public policy areas, such as:
- Transportation, such as supporting public transport availability and access versus promoting driving and highway construction
- Food systems, rewarding the growth of healthy crops and locations of grocery stores in food deserted communities, along with investing in more effective food safety regimes at the FDA
- Tax policies, for example levying soda and cigarette taxation that nudge consumers through behavioral economics to make and sustain more healthy choices
- Good job growth, where people can get employment that pays a fair wage affording families stable home lives and safe, clean housing
- Education, in particular early childhood education that protects kids from abuse and early life trauma which sustains through life and de-values human potential.
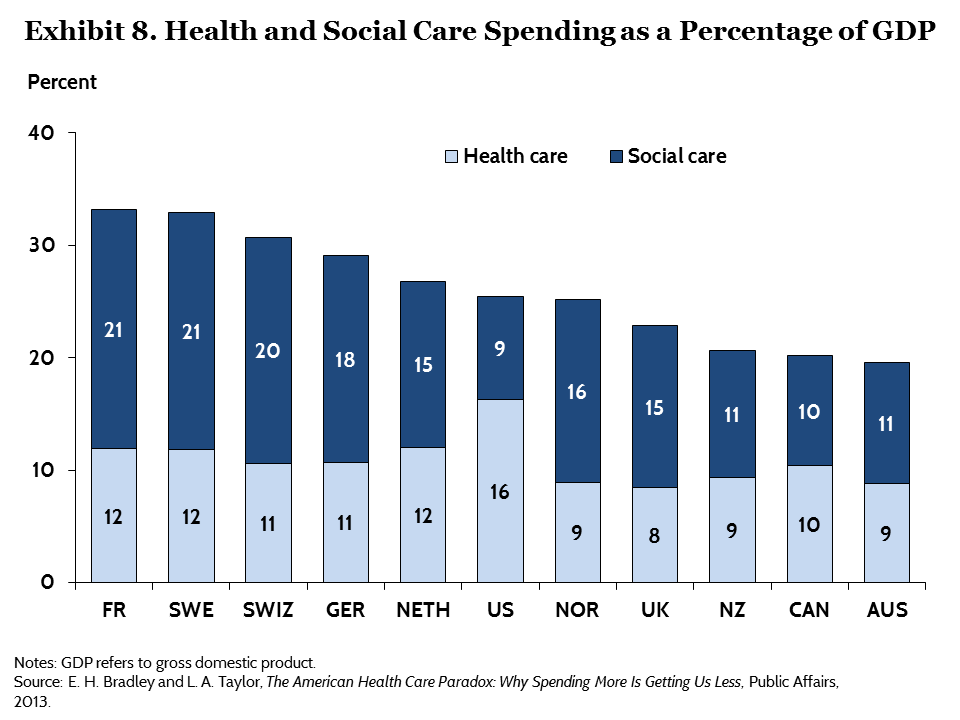
These social determinants of health (#SDOH) contribute much more to overall health and well-being — and life-extension — than genetics and access to health care services do. The U.S. allocates too little attention and money to social care investments than other wealthy countries whose citizens’ lives are longer, with quality, as the second chart illustrates (health versus social care spending as a proportion of the nations’ gross domestic product). These also boast stronger primary care backbones and healthcare access to their health citizens.
As we begin a new year and a new Presidential administration in 2017, let’s connect the dots together on what bolsters individual and public health. A case in point: New York City’s Mayor Bill DeBlasio writes this week about Healthier neighbourhoods through healthier parks in the December 10, 2016 issue of The Lancet, the British medical journal. DeBlasio is admirably following in his predecessor Mayor Bloomberg who knew and acted on the power of public health through social determinants for their health citizens.




 Thank you,
Thank you,  As a proud Big Ten alum, I'm thrilled to be invited to meet with the OSU HSMP Alumni Society to share perspectives on health care innovation.
As a proud Big Ten alum, I'm thrilled to be invited to meet with the OSU HSMP Alumni Society to share perspectives on health care innovation. I was invited to be a Judge for the upcoming CES 2025 Innovation Awards in the category of digital health and connected fitness. So grateful to be part of this annual effort to identify the best in consumer-facing health solutions for self-care, condition management, and family well-being. Thank you, CTA!
I was invited to be a Judge for the upcoming CES 2025 Innovation Awards in the category of digital health and connected fitness. So grateful to be part of this annual effort to identify the best in consumer-facing health solutions for self-care, condition management, and family well-being. Thank you, CTA!