Patients want their doctors to know what their personal costs for medicines are; 42% of patients also believe their doctor is aware of how much they spend on prescription drugs.
However, 61% of these people have not talked with doctors about drug prices. Nor do most doctors have access to this kind of information at the individual patient level.
One important tactic to addressing overall healthcare costs, and managing the prescription drug line item in those costs, is discussed in Doctors and Pharmacists: An Underused Resource to Manage Drug Costs for Older Adults, a report on a survey sponsored by AARP and the University of Michigan Medical School, and conducted by the University of Michigan’s Institute for Healthcare Policy & Innovation.
This research was part of U-M’s National Poll on Healthy Aging among 1,065 respondents ages 50-80 years of age. The term “doctor” used in the survey included health care providers broadly defined: physicians, specialists, physician assistants, and nurse practitioners.
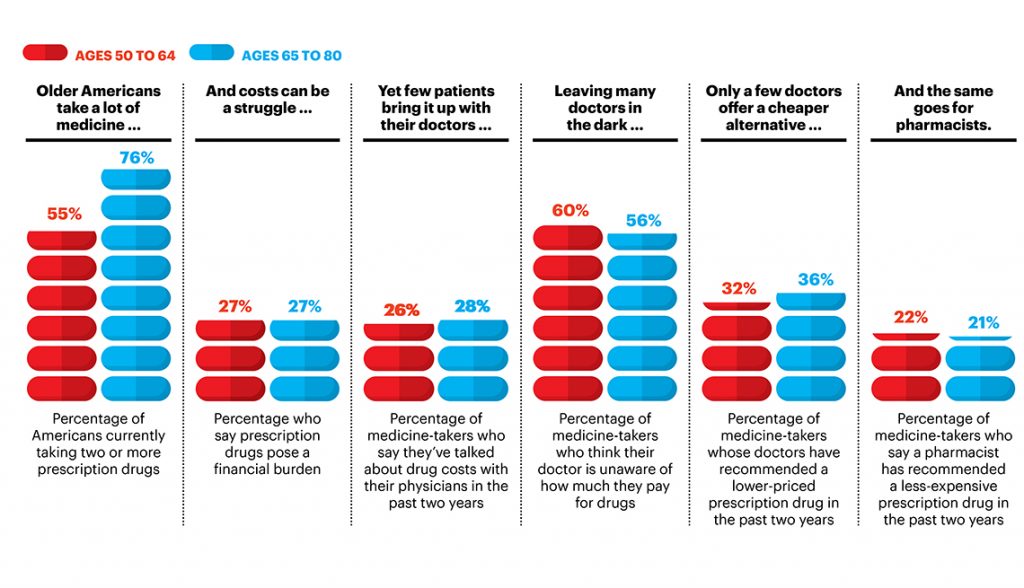
Among the survey’s key findings were that:
- 55% of people 50 to 64, and 76% of Americans 65 to 80, currently take two or more prescription drugs
- One-fourth of all adults over 50 say prescription drugs pose a financial burden, and only 49% of them talked to their doctor about costs (shown in the second graphic)
- Only one-fourth of patients 50 and over bring the topic of the high cost of prescription drugs up in conversation with their doctors
- Most older people think their doctor is unaware of how much they pay for medicines
- One-third of older Americans’ doctors have recommended a lower-priced drug in the past two years
- One-fifth of older Americans’ pharmacists have recommended less expensive drugs in the past two years.
The challenge of the prescription drug costs for older Americans increases as people age, with the reality that the older a patient gets, the more drugs they’re prescribed. Among Americans 50 and over,
- 19% face high complexity of prescription drug management, on at least 6 drugs prescribed by more than one doctor
- 47% of older Americans face moderate complexity, with 2 to 5 prescribed drugs and more than one doctor
- 34% of older people deal with low complexity, on one prescription and one prescriber.
Here’s a video put together by University of Michigan’s Institute for Healthcare Policy & Innovation discussing the survey findings.
[Herewith, I disclose my lifelong affection for U-M as my alma mater for all of my undergraduate and graduate education].
Health Populi’s Hot Points: The U-M researchers with AARP recognize that, “high out of pocket costs for prescription drugs can translate into missed doses and negative health outcomes.” Thus, the report recommends that patients should add the topic of the cost of medicines to their discussions with doctors, especially if people face a cost burden. Still, patients may feel time pressure during their visits with physicians, the researchers recognize.
The role of the pharmacist cannot be under-stated in the patient’s personal health ecosystem. Pharmacies are accessible, convenient, and freely available to people living in the U.S. Some pharmacies are open 24×7, and offer medication therapy management. My recent analysis of the state of retail pharmacy notes the growing role of pharmacies in health care, both those storefronts that are strictly pharmacy, and those co-located in grocery stores. Pharmacies, wherever sited, are morphing into primary care destinations for health support-hungry consumers.
 Regarding the cost of prescription drugs, most health consumers across the political spectrum believe in a Federal government role for dealing with the price of pharmaceutical products, noted in a recent Kaiser Family Foundation poll I discussed here in Health Populi.
Regarding the cost of prescription drugs, most health consumers across the political spectrum believe in a Federal government role for dealing with the price of pharmaceutical products, noted in a recent Kaiser Family Foundation poll I discussed here in Health Populi.
Self-rationing of prescription drugs due to cost is an American phenomenon compared with health citizens living in the rest of the world. The AARP and U-M researchers are right to point out the fact that high out of pocket costs for meds can result in missed doses and poor health outcomes; rationing does happen in the U.S., and it happens at home as patients, now health care consumers, make decisions to allocate family budgets between healthcare, housing, utility bills, and food.
I’ve made the case for physicians to morph into health economists. Clearly, patients are demanding more transparency for health care costs, and particularly for prescription drug costs, at the point-of-prescribing. Health information systems via the EHR should address this patient demand by building in patients’ personalized prescription drug benefit data before sticker shock, and abandoned prescription fulfillment, ensues at the drugstore. A growing supply of consumer-focused mobile apps have begun to fill this demand: I note more broadcast advertising dollars supporting the efforts of BlinkHealth and GoodRx, for example. They are surely filling a gap for consumers; but not the communications gap between doctors and patients for shared decision-making.




 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.