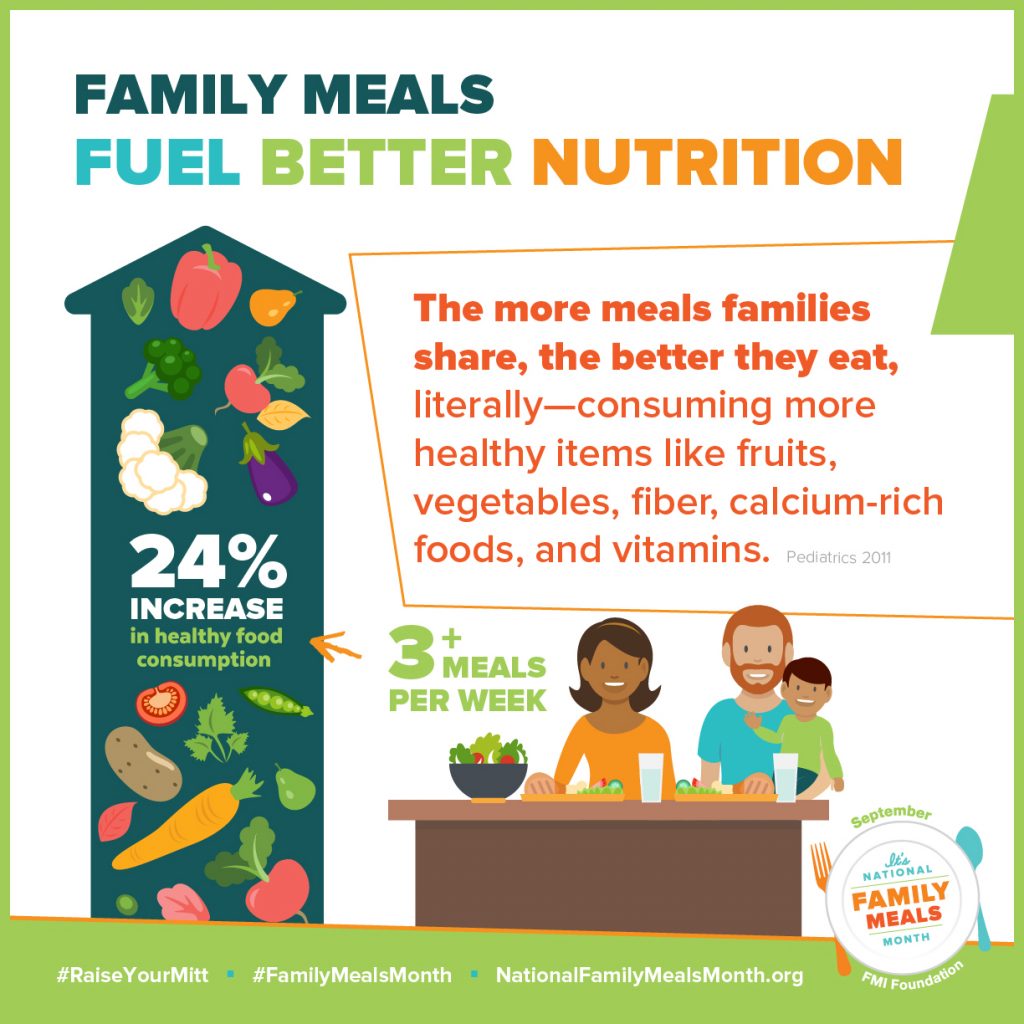
 When a family eats together, they eat more nutritiously, A family that shares 3 or more meals together each week has a 24% greater consumption of nutritious food.
When a family eats together, they eat more nutritiously, A family that shares 3 or more meals together each week has a 24% greater consumption of nutritious food.
Yet only one-half of families in the U.S. with kids under 18 eat dinner together every night of the week, a Gallup poll found.
It’s National Family Meals Month. Eating together as a family is a social determinant of health, and the Food Marketing Institute dedicates the month of September to promote the old school concept of the “family meal.”
Nutrition habits are built from early childhood. More kids are showing interest in food and nutrition, as evidenced by the growing inclusion of children on Food Network TV (in shows like Chopped, Jr., now in its 7th season), boosted by the stalwart efforts of Alice Waters and Jamie Oliver for healthy food in schools.
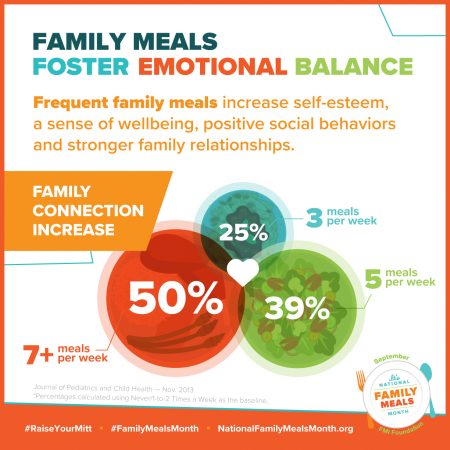
There’s also clinical evidence that more frequent family dining can help reduce obesity rates, eating disorders, and the incidence of diabetes.
Grocers and food manufacturers are sponsoring programs to support the family meal.
Grocery chains are using #FamilyMealsMonth to promote home cooking and sharing meals around the table. Some grocers’ health-related programs are offered by:
- Hy-Vee, Stay Healthy Together
- Meijer and Produce for Kids
- Kroger, with a tasty take on the Flavors of Mexico
- Wegmans, boosting the importance of home cooking.
and others. Just Google your favorite grocery chain and “Family Foods Month and 2017” and you’ll find all kinds of tactics to make family meal planning easier and financially palatable. The USDA also has an informative portal on family meals here.
For more real-time stories about this important program, follow #FamilyMealsMonth on Twitter.
Health Populi’s Hot Points: Doctors and the U.S. health system has begun to embrace the importance of nutrition as a factor in primary health that’s outside of the physician’s office. Note that primary care providers who could add a new staff member to their office teams would first choose a nutritionist or dietitian above any other worker-category, above mental health professional (#2 on the list), a clinical educator, or a social worker (via a PwC HRI survey).
A new article in JAMA published 7th September 2017 talks about Nutrition Counseling in Clinical Practice: How Clinicians Can Do Better. The article points out that despite evidence that small dietary changes can significantly impact patients’ health, doctors are ill equipped to discuss nutrition with them. Only 12% of office visits include counseling about diet, and only 20% of patients with heart disease or diabetes receive nutrition counseling.
The authors point out that nutrition counseling has long been a non-reimbursed service in commercial as well as government-sponsored health plans, in most cases. The reimbursement challenge couples with the nation’s food system environment: less nutritious foods are less expensive for consumer budgets, so patient adherence to nutrition advice can be compromised, especially for lower-income patients.
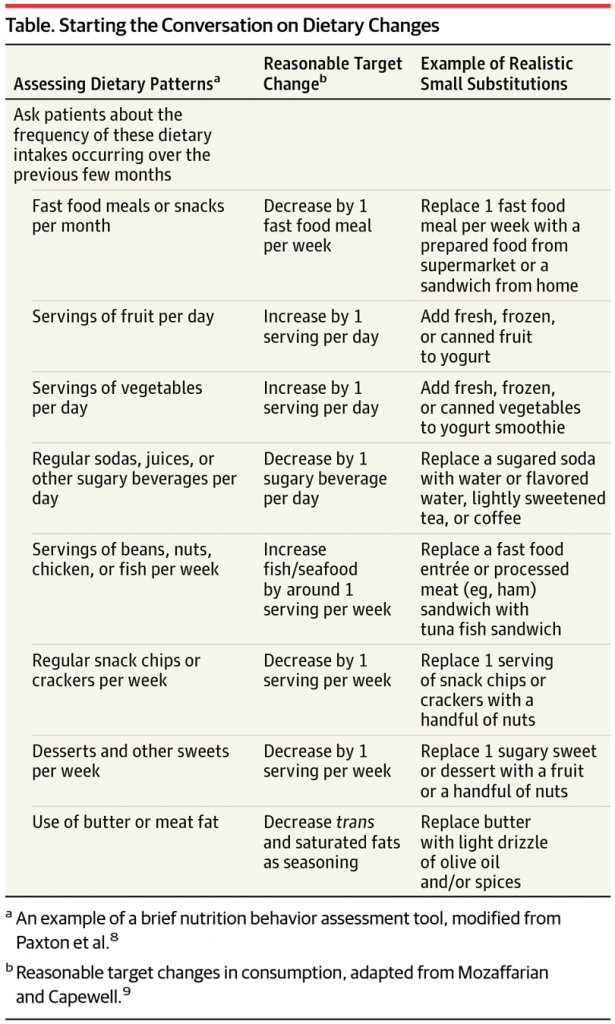 Value-based payment programs can align financial with clinical objectives, the article concludes. The authors, both physicians, recommend several steps to kick off the process in the clinical encounter:
Value-based payment programs can align financial with clinical objectives, the article concludes. The authors, both physicians, recommend several steps to kick off the process in the clinical encounter:
- Start the conversation with a few simple screening questions (see the table here)
- Structure the encounter with “5 As:” assess, advise, agree, assist, arrange, adapted from a useful smoking cessation counseling technique
- Focus on small steps, a la B.J. Fogg’s advice
- Use available resources
- Don’t do everything at once (again, THINK: small steps)
- Don’t do it all alone: collaborate, work together in the community (read #4 again).
And, of course, go back to the family meal recommendation and if the person lives alone, remember: health is social and we are connected in social networks for health.





 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...