Four in five U.S. physicians were using telehealth to care for patients at the end of 2021.
Among those doctors who were not providing telehealth by late 2021, just over one half never did so during the COVID-19 pandemic, according to the 2021 Telehealth Survey Report from the AMA.
This report provides insightful context for the upcoming annual ATA Conference for 2022, being held in-person in Boston kicking off May 1st. The meeting will be a strategically important, as the title of the conference asks: “What Now? Creating An Opportunity in a Time of Uncertainty.”
While most physicians entered 2022 using telehealth in caring for patients, one-half had decreased use primarily due to seeing more patients in-person mixed with virtual visits, and noting that either the patients or the clinicians themselves preferred to provide care in-person, the AMA found.
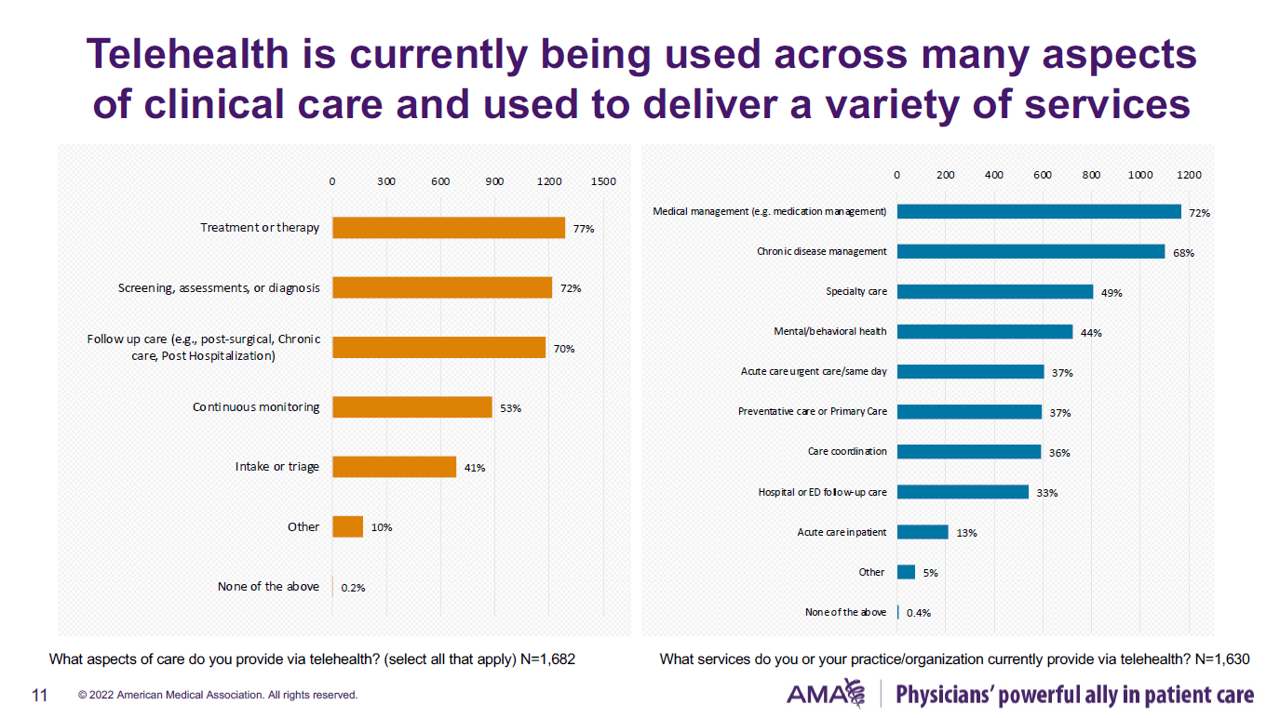
Doctors are deploying telehealth across a range of care workflows, shown in the bar chart.
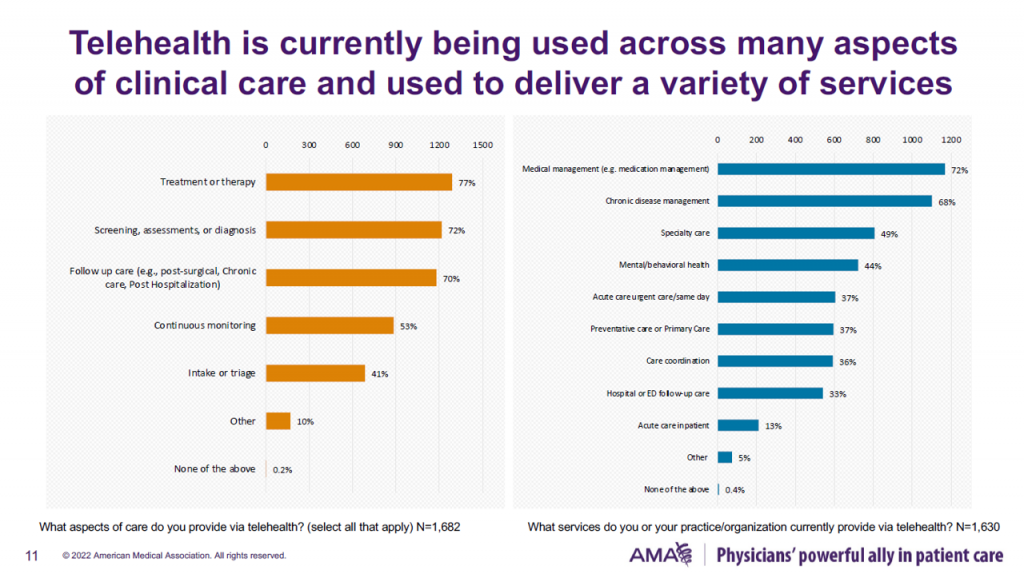
Most frequently, virtual care is being used for treatment or therapy, screening or diagnosis, and follow-up care, by at least 70% of clinicians. One-half of doctors uses telehealth for continuous monitoring of patients,
Overwhelming, medical and chronic disease management are the workflows for telehealth, followed by one-half of physicians using virtual care for specialty visits and 44% for mental and behavioral health.
Urgent care, the historically top use of telemedicine, is deployed by 37% of physicians in this study.
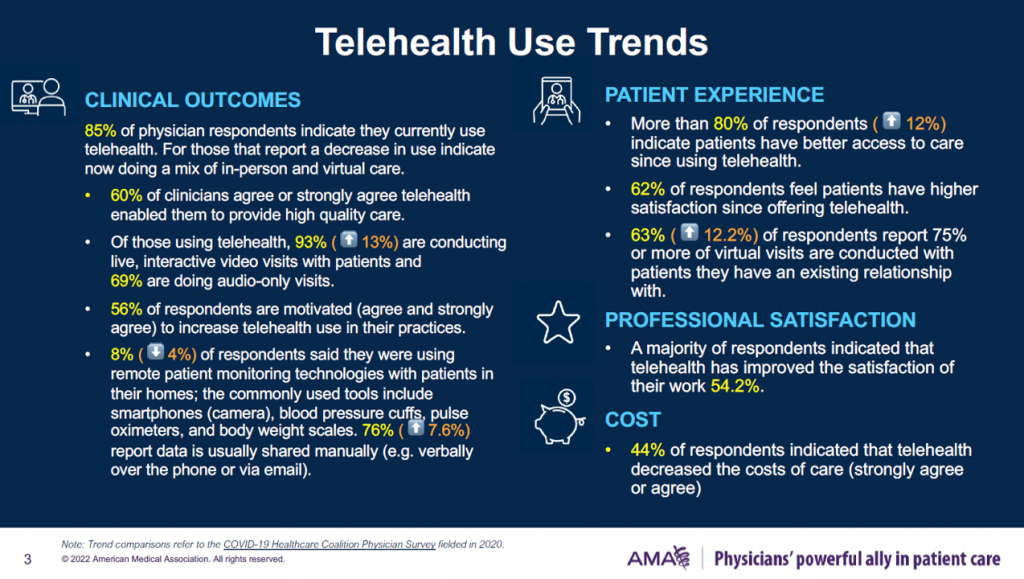
Given these data points, most physicians feel that telehealth allows doctors to provide more comprehensive care, agreed by about 60% of the clinicians. Most doctors also said that virtual care has improved patient satisfaction due to the platform’s access and convenience aspects.
Following patient satisfaction is physician satisfaction with telehealth, which has increased professional satisfaction among over 50% of doctors.
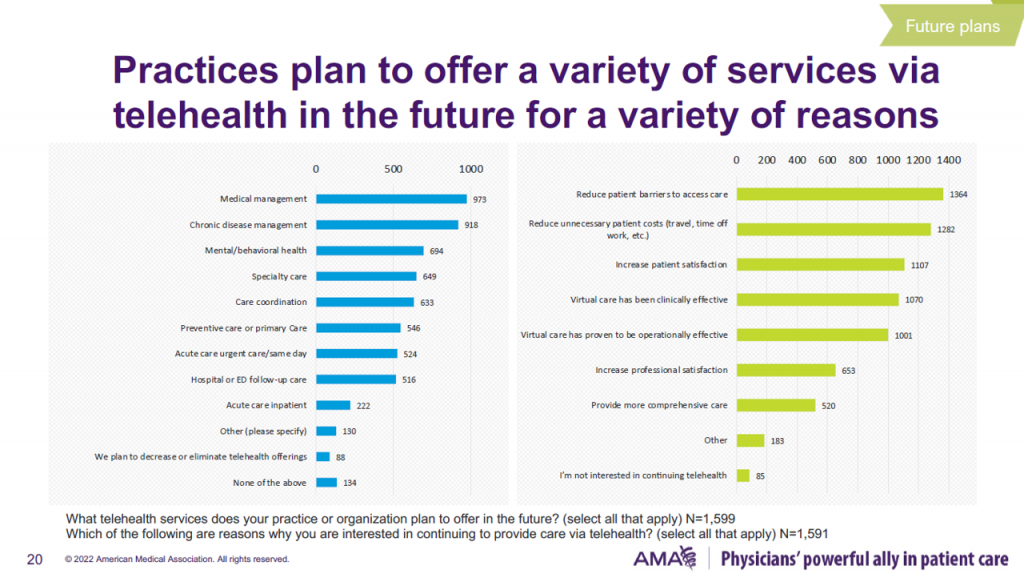
As such, most physicians and clinical organizations are interested in continuing to offer and expand telehealth to their patients. Reasons for doing so, among over 50% of doctors, include:
- Medical and chronic disease management
- Mental and behavioral health
- Specialty care
- Care coordination and continuity
- Preventive and primary care
- Acute, urgent, and same day care, and
- Hospital or emergency room follow-up.
But not so fast — there remain barriers to offering telehealth, with concerns about the roll-back of COVID-19 waivers, insurance coverage, and payment/reimbursement at the top of that list of obstacles to sustainable virtual care in practice.
Cross-state licensure barriers rank lower on the barrier list, with 54% of physicians anticipate being an ongoing challenge for continuing to offer telehealth.
Note that for this research, the AMA polled 2,232 physicians in November and December 2021 to gauge their perspectives on telehealth. (Due to the sample size, the Association advises us to see the data as “directional” and not methodologically statistically significant).
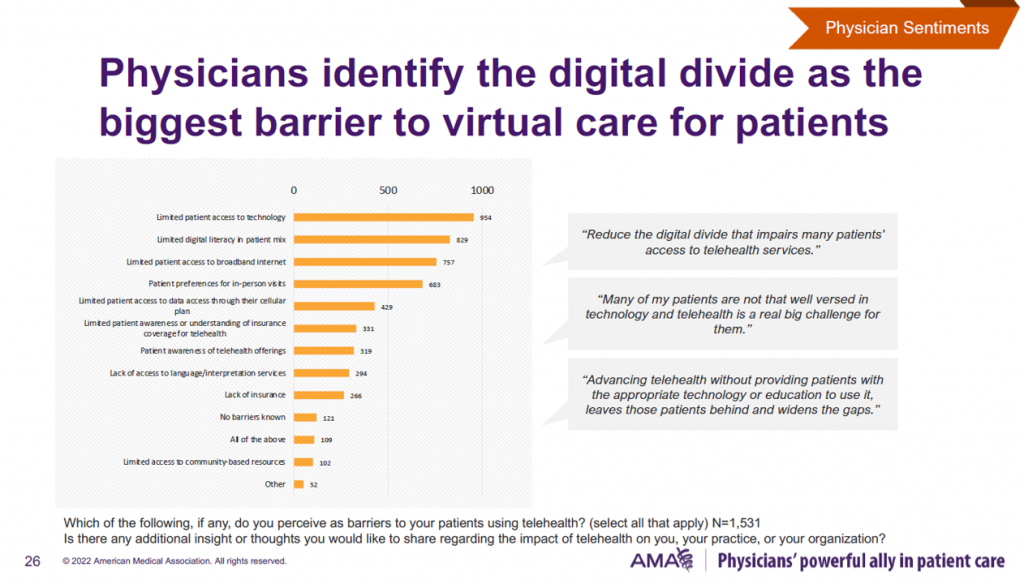
Health Populi’s Hot Points: Another barrier to physicians’ perceived ability to provide and expand services via telehealth are technology challenges for their patient population, and the digital divide confronting some of their patients.
The AMA explored the digital divide in some detail, calling it out as, “the biggest barrier to virtual care.”
The bar chart quantifies aspects of the challenge, led by three technology-related barriers: patients’ limited access to technology, limited digital literacy, and limited access to broadband.
As one clinician quoted in the AMA’s report described, “Advancing telehealth without providing patients with the appropriate technology or education to use it leaves those patients behind and widens the gaps.”
One of the side-effects of the COVID-19 pandemic was the digital transformation of people — using Zoom for work, going to school from home via Internet connection, attending prayer services to connect with faith communities, taking exercise classes at home in groups, virtually — via tele-exercise whether via the Y, Orangetheory, or a yoga instructor pivoting to online platforms, consumers’ mats stretched out on living room floors.
Those new life-flows were accessible and welcomed by people who had access to the Internet and connectivity via broadband/WiFi, and the hardware and data plans to digitally engage.
While doctors noted to the AMA their top virtual care platform of choice was Zoom, some patients could not meet-up due to barriers of lacking a smartphone, tablet, or computer device; the ability to pay for connectivity to the Internet; or the know-how to be able to access that well-intentioned “digital front door” to a virtual visit.
As the pandemic exacerbated many risks of social determinants of health like food security and the ability to earn a wage in hospitality or caregiving jobs, so, too, did the public health crisis shine a light on a newer determinant of health: connectivity as a basic human need.
Physicians realize that now, as sure as they may ask patients about their nutrition intake, job security, and ability to get to a doctor’s appointment for an office visit….
Many sessions during #ATA2022 will be addressing various aspects of this challenge: exploring the sustainability of telehealth, best practices, evidence-based case studies, and to be sure, health equity.
Follow the meeting on Twitter at #ATA2022. I know I’ll be paying close attention, keen to learn from the updates and insights.
Kudos and thanks to the AMA for conducting this important research.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...