 Investing information technology dollars in telehealth and mobile platforms, patient engagement, and cybersecurity are major focuses for leading IT-savvy hospitals in America, according to the 2016 Most Wired survey of healthcare organizations, released in July 2016 sponsored by Hospitals and Health Networks and Health Forum, a division of the American Hospitals Association.
Investing information technology dollars in telehealth and mobile platforms, patient engagement, and cybersecurity are major focuses for leading IT-savvy hospitals in America, according to the 2016 Most Wired survey of healthcare organizations, released in July 2016 sponsored by Hospitals and Health Networks and Health Forum, a division of the American Hospitals Association.
This survey, in its 18th year, has become an important benchmark measuring the adoption of information technology tools and services among American hospitals and health systems. The complete list of Most Wired hospitals for 2016 can be found here.
The most popular telehealth services offered by the Most Wired hospitals are virtual consultations and office visits, among 61% of Most Wired vs. 43% of all hospitals; remote stroke care for 49% of Most Wired compared to 39% of all hospitals; and, telemental health (remote psych examination and psychotherapy) for 47% of Most Wired vs. 34% of all hospitals. The first chart details the telehealth service utilization for 2016 Most Wired compared with all hospitals.
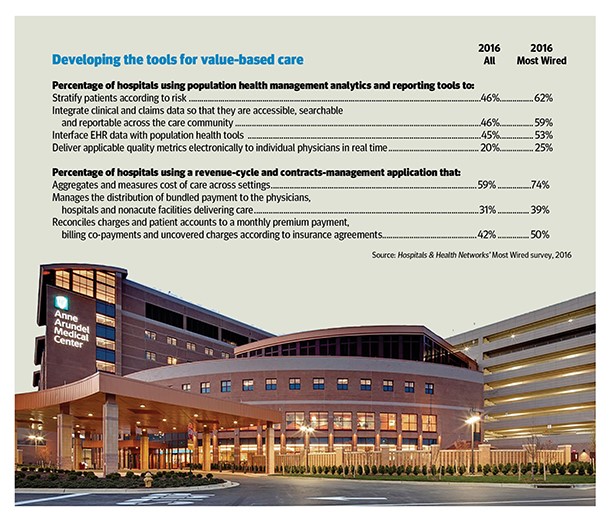 A growing population-health among health providers is driving adoption of IT tools for value-based care, according to the research. 62% of Most Wired hospitals are stratifying patients according to risk, 59% integrating clinical and claims data, and 53% interfacing EHR data with population health tools, shown in the second graphic.
A growing population-health among health providers is driving adoption of IT tools for value-based care, according to the research. 62% of Most Wired hospitals are stratifying patients according to risk, 59% integrating clinical and claims data, and 53% interfacing EHR data with population health tools, shown in the second graphic.
Revenue-cycle management is an important competency in a growing value-based payment era, with 74% of Most Wired aggregating and measuring cost of care across settings; 50% reconciling charges and patient accounts to a monthly premium payment and other charges based on insurance contracts; and, 39% managing distribution for bundled payments to providers in their system (doctors, hospitals, non-acute facilities). See the second chart for details comparing Most Wired and all U.S. hospitals.
Cybersecurity is top-of-mind for the vast majority of hospitals, both uber-Wired and overall: 93% of Most Wired hospitals are using mobile-device encryption, 89% adopting mobile-device management systems, 78% employing two-factor authentication, and 68%, digital signatures. This issue has hospital board-level oversight among 90% of the Most Wired. And, a majority of both Most Wired and all hospitals are engaging third-party security audits to risk-manage cybersecurity.
The AHA’s press release noted that, “In redefining the way that they provide care in their communities, Most Wired hospitals are using technology to build patient engagement with the individual’s lifestyle in mind, which includes electronic access to their care team” via patient portals, mobile e-visits, and social media for patient support groups.
The survey was conducted between January and March 2016 among 680 participants representing 2,146 hospitals – about one-third of all hospitals in the U.S.
Health Populi’s Hot Points: Hospitals are moving outside of their traditional four walls, providing care where and when patients need it, according to AHA’s CEO and President Rick Pollack. As such, health providers are investing more capital dollars in technology to manage virtual care between providers, and providers and their patients; geographically disparate teams (the “liquid labor force”); deeper implementation of electronic health records to derive more benefits from that significant investment; and, big data analytics, among other projects covering the survey’s four focus areas: infrastructure, business and administrative management, clinical quality and safety, and clinical integration across provider communities (hospital, ambulatory, physician, patients, and community).
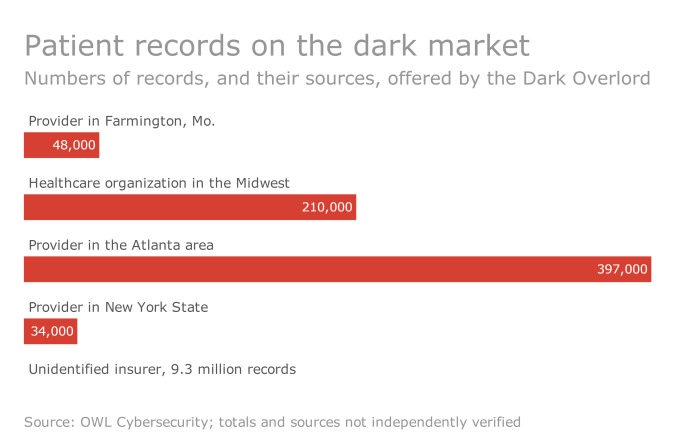 What’s keeping hospitals’ CxOs up at night is the valuable hacker’s market for personal health record data. This year’s Most Wired survey demonstrates the near-universal acceptance of this new reality, and subsequent investments that the vast majority of U.S. hospitals are making to secure patients’ personal health information. The pace of growth of the threat is growing; there’s coverage on the issue discussed this week here in Health Data Management, talking about The Dark Overlord offering ransoms for EHR data. See the bar chart for details of where the so-called Dark Overlord has cyber-struck health care organizations. The challenge is getting coverage well beyond health-tech trade publications: for example, US News & World report covered this threat in April 2016. PBS News Hour asked, “Has health care hacking become an epidemic?”
What’s keeping hospitals’ CxOs up at night is the valuable hacker’s market for personal health record data. This year’s Most Wired survey demonstrates the near-universal acceptance of this new reality, and subsequent investments that the vast majority of U.S. hospitals are making to secure patients’ personal health information. The pace of growth of the threat is growing; there’s coverage on the issue discussed this week here in Health Data Management, talking about The Dark Overlord offering ransoms for EHR data. See the bar chart for details of where the so-called Dark Overlord has cyber-struck health care organizations. The challenge is getting coverage well beyond health-tech trade publications: for example, US News & World report covered this threat in April 2016. PBS News Hour asked, “Has health care hacking become an epidemic?”
Ironically, it’s the very nature of the new-new technology – virtual care, telehealth, mobile platforms, digital health records – that provide the hacker their opportunity to breach security. Health information turns out to be a very valuable commodity: according to the Ponemon Institute, the average cost per stolen healthcare record is $355; the average global cost of a stolen record is $158.





 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...