California’s Governor Jerry Brown signed into law a net neutrality bill this weekend. Gov. Brown’s proverbial swipe of the pen accomplished two things: he went back to the Obama-era approach to ensure that internet service providers treat all users of the internet equally; and, he prompted the Department of Justice, representing the Trump Administration’s Federal Communications Commission (FCC), to launch a lawsuit.
California, home to start-ups, mature tech platform companies (like Apple, Facebook and Google), and countless digital health developers, is in a particularly strategic place to fight the FCC and, now, the Department of Justice. Nearly two dozen other states are looking to write net neutrality laws following Governor Brown’s example.
“Net neutrality, at its core, is the basic notion that we each get to decide where we go on the internet, as opposed to having that decision made for us by internet service providers,” California State Senator Scott Wiener said about the rationale for the law which he drafted.
This blog, Health Populi, covers the intersection of health, people, technology, and economics. The issue of net neutrality and Everyday Peoples’ access to connectivity and broadband lies at the heart of this intersection. I’ve talked about the importance of connectivity as a social determinant of health here on this site in December 2017, as well as in July 2016 in the Huffington Post (appropriately published in the “Life/Wellness” section).
Resilient, consistent broadband connectivity is a social determinant of health because healthcare with providers and insurance plans, and self-care done in the DIY health sense, both depend on access to the internet: to providers’ portals for accessing our personal electronic health records; to sign up for health insurance, whether commercial plans via an employer or for, say, Medicare Part D prescription drug benefits; to search information on our health, wellness, and medical treatments via “Dr. Google,” WebMD, or any number of .gov, .edu, or .com healthcare information on-ramps; or, to order medical supplies and equipment on ecommerce sites like Amazon, CVS, Walgreens, Walmart, and other retail health outlets.
Health consumers and patients, without access to connectivity, can’t engage with modern healthcare in these ways.
”Broadband subscriptions are up, but too many households are still disconnected,” an essay published by Brookings was titled last week.
“Whether it’s consumers who are forced to pay higher prices at a local store than online, children who must travel to do web-based homework, or job seekers missing out on employment openings, Americans who lack a private broadband subscription shoulder substantial costs,” Tomer and Fishbane explained in their article.
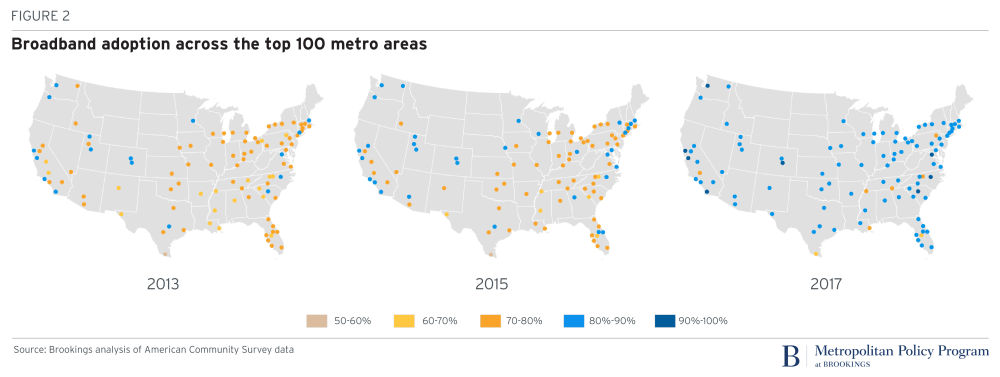
These three maps illustrate the inconsistent growth rates across metro areas in the U.S, leaving many people “in the digital dark,” the authors note. These gaps show that broadband access is “far” from matching other essential infrastructure services.
There is indeed improvement, Brookings’ analysis found, but millions of people still lack broadband access…separate from the issue of net neutrality.
Health Populi’s Hot Points: An update to the census-tract level broadband estimates will be published in December 2018, and this will give us updated pictures into neighborhood-specific connectivity. This is so important for health given that most of us in the field agree that our “ZIP code is more important than our genetic code.”
Just ask Americans: the most recent data from the Pew Research Center finds that one in 4 Americans said access to broadband was difficult.
That is, where we live directly shapes our socio-economic status, access to healthy food, education, transportation lines, jobs, and health care access — especially primary care.
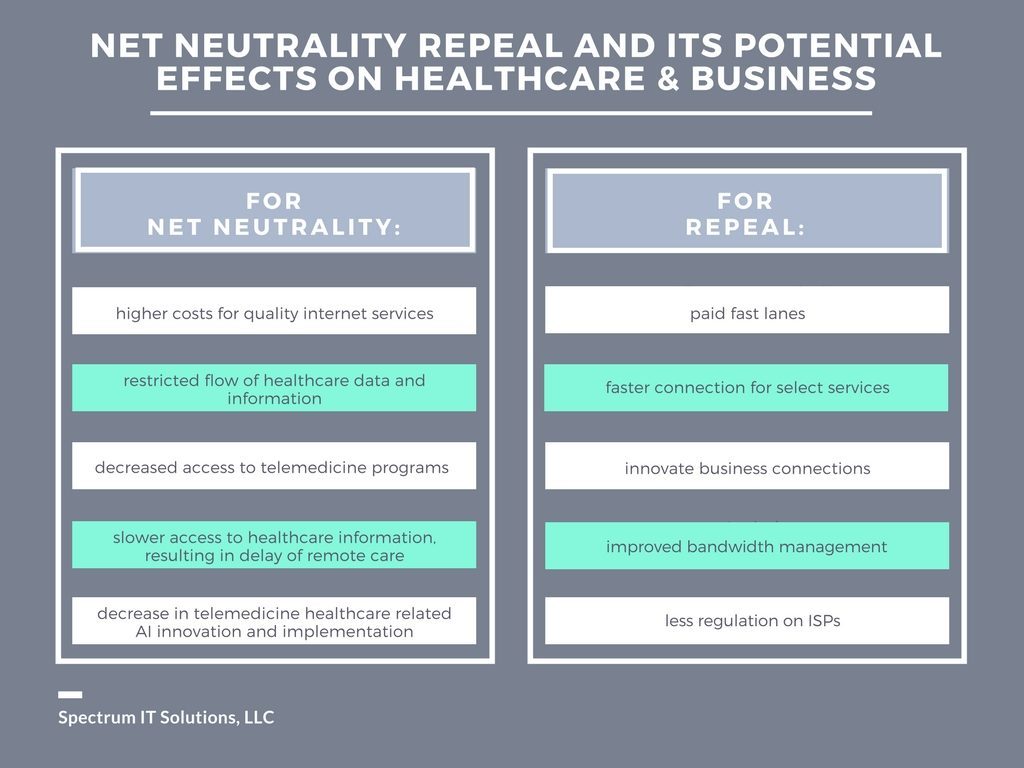
The second graphic, developed by Spectrum IT Solutions, identifies some areas where losing net neutrality could negatively impact healthcare — namely, higher costs for better internet services (which less-affluent patients could afford), restricted flow of healthcare data, and eroded access to telehealth, remote and virtual care programs. Together, these compromises could lead to increased healthcare costs, delayed diagnoses resulting in poorer outcomes and greater treatment costs, and delayed care — again, driving costs up through care delays and exacerbated medical conditions.
In parallel, U.S. patients would have lower quality healthcare at a higher cost, lower productivity, and less ability to contribute to the local and national economy as health citizens.
Broadband and its fair access rules for all health consumers through net neutrality are a bundled social determinant of health. Without them, the U.S. can neither address health disparities, health equity, public health, or bend that ever-increasing cost-curve through enabling access to lower-cost care and, especially, self-care.





 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...