In the nation’s search for spending smarter on health care, the U.S. could save at least $13 billion a year through deploying medically-tailored meals for people enrolled in Medicare, Medicaid, and private insurance programs, according to the True Cost of Food, research published by the Tufts School of Nutrition Science and Policy collaborating with The Rockefeller Foundation.
It’s been one year since the White House convened the Conference on Hunger, Nutrition, and Health, kicking off the Biden Administration’s national strategy to improve health citizens’ access to healthy food as a matter of public health and economic security.
Over the past year, many stakeholders have come together to develop creative solutions to address food security for all — as a driver of health, productivity, and sustainability for the U.S. health care system.
Consider Chicago. The Windy City’s Mayor Brandon Johnson launched a study in September to explore options for launching and operating a municipally-owned grocery store to address the city’s food desert challenge.
“All Chicagoans deserve to live near convenient, affordable, healthy grocery options. We know access to grocery stores is already a challenge for many residents,” the Mayor explained. “The City of Chicago is reimagining the role government can play in our lives by exploring a public option for grocery stores via a municipally owned grocery store and market,” a city economic security advisor noted.
As the Tufts report explained, we can dig deeper into the concept of food security as a social determinant of health to see poor nutrition as a foundational determinant of health.
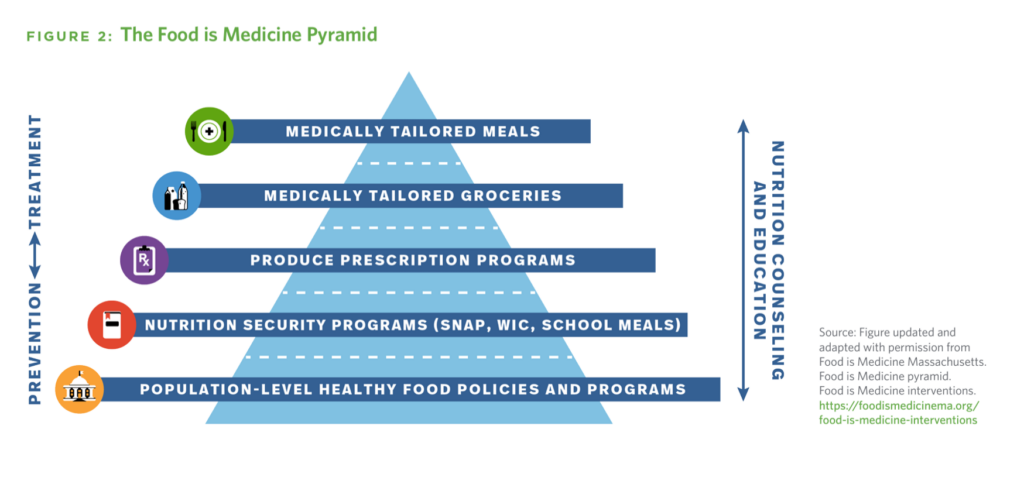
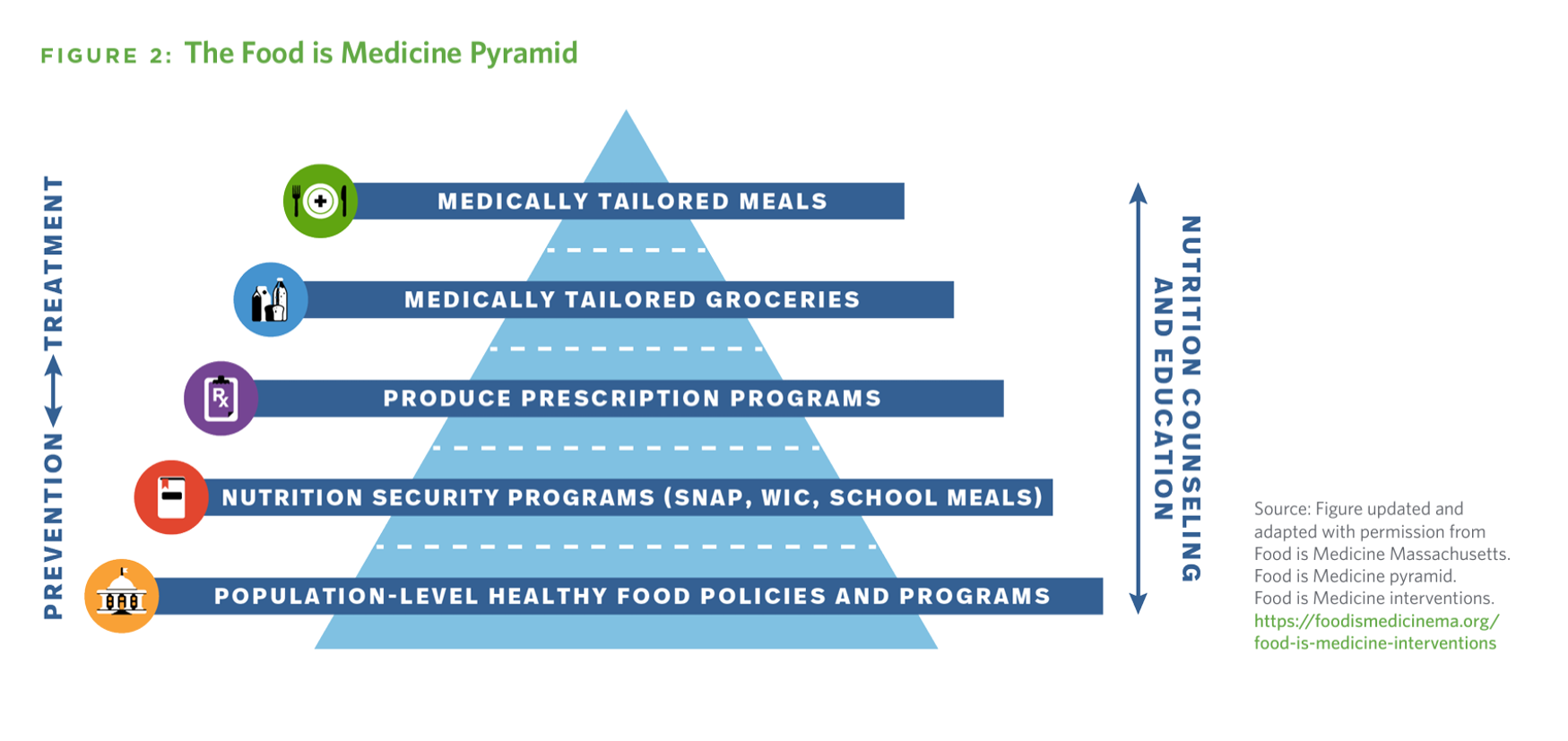
The Food Is Medicine (FIM) pyramid here illustrates the layers of that concept, the base of which is population-level healthy food policies and on top of the macro policies, specific nutrition security programs such as SNAP and WIC benefits that literally feed families and children at-risk for food deficits.
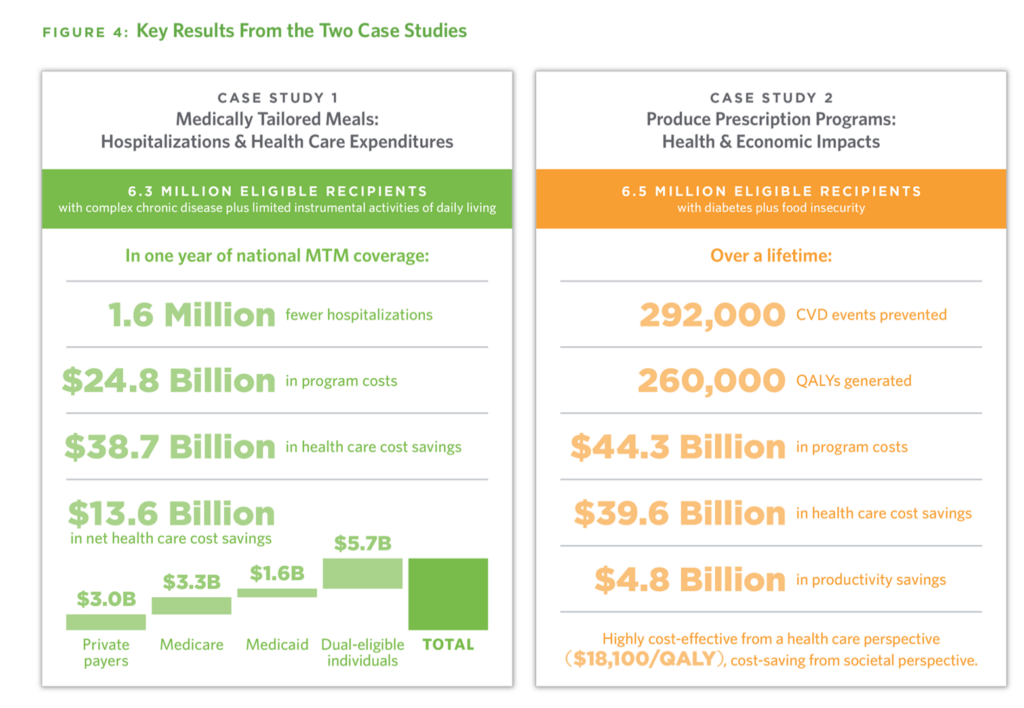
The health and economic benefits of medically-tailored meals and produce prescriptions (e.g., via “food farmacies”) are quantified here in the Tufts model, amounting to billions of dollars of savings and over a million hospital admissions averted in Year 1 of such a program.
These programs are particularly salient and impactful for patients dealing with cardiovascular diseases, diabetes, and cancer, Tufts called out in the report.
Inspired by the 2022 White House Conference, a consortium of five health care industry stakeholders came together to evolve, in their words, “a new way to think about food” with the hashtag, #NourishMy Health.
For this effort, Tufts Food Is Medicine Institute was joined by the American Cancer Society, the American Diabetes Association, the American Heart Association, and the National Association of Chain Drug Stores (NACDS).
NACDS published some major commitments and bold recommendations last year in sync with the White House Conference, especially focused on pharmacists’ and dietitians’ roles in bolstering communities’ health at home and closer-to-home — for conditions notably amenable to self-care and DIY which more consumers are embracing to manage diagnosed conditions as well as preventing their onset. [For more on that issue, see this post in Health Populi exploring CES 2023 technologies that bolstered patients’ self-care through consumer-facing technologies — which I’ll update at #CES2024].
Grocery stores, too, are part of the food-as-medicine movement in the retail health landscape. Note that in McKinsey & Company’s latest report on The state of grocery in North America 2023, the company asserts that, “grocery stores have become a destination for health and wellness — not just for food but also for nutrition and healthcare services.” [As a pretty good tea-leaf reader, I pointed this out in my 2019 book, HealthConsuming, devoting a section to “the grocery store as health destination”].
In that vein, another collaborator in the White House Conference was Kroger, the grocery chain, which has been growing its health/care portfolio beyond the food aisles through the Kroger Health operation and the store’s pharmacy business. One year later, following up its commitments announced at the Conference, Kroger held what it termed the Nourishing Change Summit to advance Food as Medicine.
“We have the unique opportunity to provide customers and patients with the resources they need to make healthier food choices and, ultimately, change their health outcomes,” Colleen Lindholz, president of Kroger Health, explained. “The future of healthcare isn’t volume-based, it’s value-based and personalized. Built on the foundation of Kroger Health’s industry-leading commitment to Food as Medicine, we are leading thoughtful discussions with a diverse set of leaders who use their broad expertise to create healthier communities.”
Several insights emerged from the Summit, including the learnings that,
- Collaborating across industry sectors can bolster healthier communities,
- Members of those communities — health citizens, all — play key roles in identifying local health needs and outcomes, and
- Each person’s health journey is unique, so solutions to “nourishing health” must be personalized to be effective and sustainable.
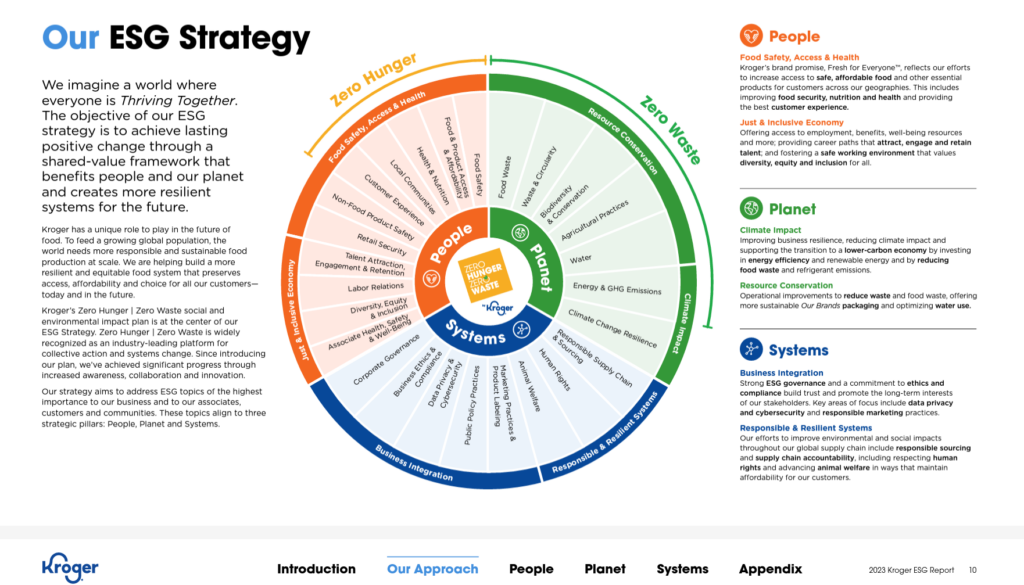
I’ve reviewed Kroger’s latest ESG corporate responsibility report, pulling the graphic above from it. If you read the fine print, you’ll see health, well-being, and equity baked into many aspects of the company’s approach to environmental, societal, and governance commitments. These address food safety, access and health; food access and affordability; health and nutrition; and prescription drug awareness, among other ESG objectives.
This is a fast-evolving space and part of my ongoing research and work with health/care ecosystem stakeholders across a diverse group of sectors — per Kroger’s advice for cross-sector collaboration.
For a good primer into Food-Is-Medicine, I recommend this paper from the BMJ’s “Food For Thought 2020” series on FIM actions to integrate food and nutrition into healthcare. In particular, check out a sidebar in Box 1 on examples of integration of FIM interventions in the U.S. — focusing on the states of Massachusetts and California using FIM programs with high-risk populations. This is one work- and policy-flow that helps to address health disparities and inequities while improving public and individual health, and empowering local communities and economic productivity.

Health Populi’s Hot Points: Looking at the future of food, the Backs\ash forecasting team from TBWA explored many driving forces shaping prospects for food and nutrition.
In the Food Rx discussion, the team points out the blurring lines between food and pharma, observing that consumer expectations are rising, seeking specific health and wellness benefits from what they consume. There’s a higher bar for so-called “health food,” along with expectations for personalization — begging the question, “What if….grocery stores offered personalized nutrition counseling? Allowing shoppers to get special recommendations and curated shopping lists made just for them?”
Of course with the promise of Food Rx comes a paradox — for example, that which this quote highlights. “There is an epidemic of people using drugs to continue eating badly,” from TBWA’s Des Jones.
While this is not a new concept, the team’s report realizes, “with the rapid rise of drugs like Ozempic, the conversation is taking a serious turn.”
And that prompts the question, “What if…food and pharma companies teamed up to make nutritious food more accessible?”
As Alicia Kennedy, Food & Culture Writer, asserts in the report’s introduction, “The future of food can be sustainable, delicious, beautiful, nutritious, and community-oriented….a source….of abundance, sharing, and good health.”
And Food as Medicine can be part of that vision. Here’s why….here’s the opportunity and the call-to-action…




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...