“More than a year and a half into the COVID-19 outbreak, the recent spread of the highly transmissible delta variant in the United States has extended severe financial and health problems in the lives of many households across the country — disproportionately impacting people of color and people with low income,” reports Household Experiences in America During the Delta Variant Outbreak, a new analysis from the Robert Wood Johnson Foundation, NPR, and the Harvard Chan School of Public Health.
 As the HLTH conference convenes over 6,000 digital health innovators live, in person, in Boston in the wake of the delta variant, what should attendees keep in mind to help HLTH make health?
As the HLTH conference convenes over 6,000 digital health innovators live, in person, in Boston in the wake of the delta variant, what should attendees keep in mind to help HLTH make health?
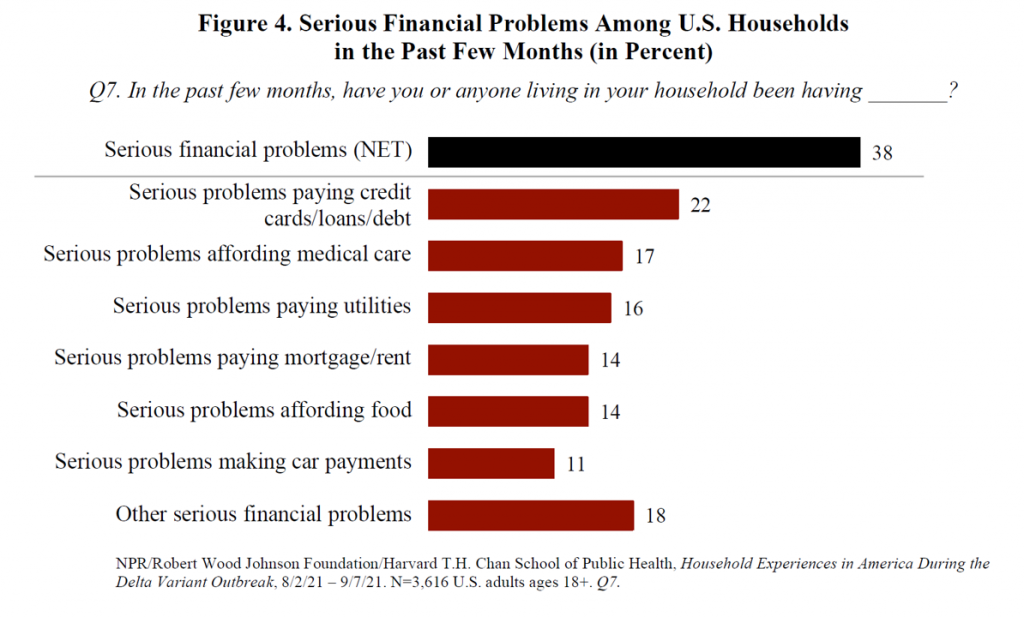
The top-line in the report, and the bottom-line for health citizens, was that 38% of U.S. households faced serious financial problems in 2020 in the delta variant phase of the pandemic.
This financial hit affected lower-income people earning under $50,000 a year harder than those with higher incomes, and especially impacted people who rented their homes and people of color.
The survey informing the report was conducted between August 2 and September 7, 2021, among 3,616 adults 18 and older (in English, Spanish, Mandarin, Cantonese, Korean, and Vietnamese based on consumers’ language preferences). The survey broke out race and ethnicity in terms of white, Hispanic/Latino, African American/Black, Asian, and Native American/American Indian/Alaska Native.
The major financial problems people faced in the past few months included making credit card and loan payments (among 1 in 5 people), affording medical care (for 17%), paying utilities, paying mortgage or rent, and affording food, shown in the first graph from the report (“Figure 4”).
Fifty percent of households without health insurance reported trouble affording medical care compared with 13% of people with health insurance.
One-half of U.S. households overall also said someone had experienced serious problems with depression, anxiety, stress, or sleeping in the past few months.
 Health Populi’s Hot Points: This week during the HLTH conference, we’ll learn about exciting developments in new digital health products and services embedding AI, leveraging virtual care and telehealth, serving up new models of primary care, and a growing supply of mental health services that can scale beyond traditional face-to-face synchronous therapy encounters between patient and therapist.
Health Populi’s Hot Points: This week during the HLTH conference, we’ll learn about exciting developments in new digital health products and services embedding AI, leveraging virtual care and telehealth, serving up new models of primary care, and a growing supply of mental health services that can scale beyond traditional face-to-face synchronous therapy encounters between patient and therapist.
That’s the supply side of HLTH. But there are opportunities to learn from patients and advocacy groups at the meeting to inform the demand side of the health/care equation, and that’s crucial to understanding consumer experience, values and sense of value that enables people to get the care they need.
Particularly for those health citizens who have been long under-served by healthcare and digital health tools.
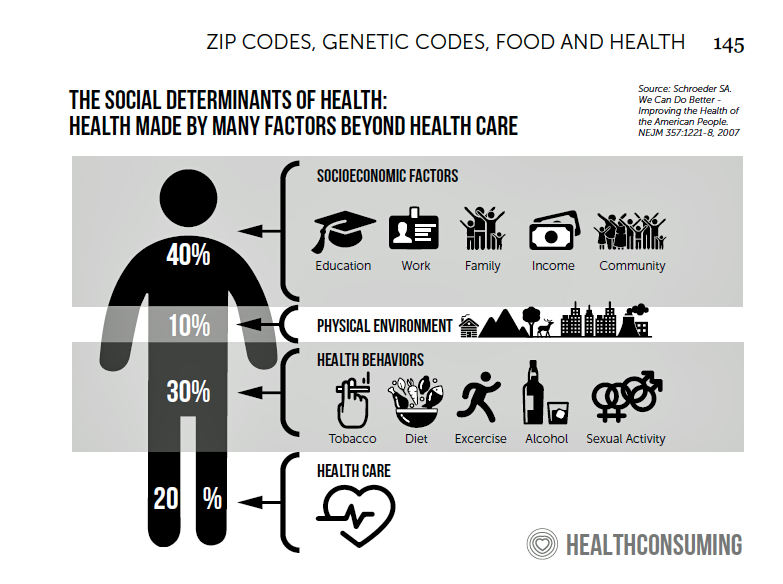
The fact is that the best-designed digital health innovations can’t, themselves, address the root causes of un-wellbeing and poor health outcomes which are influenced, from pre-birth through our early childhoods.
Those social determinants are intimately, inextricably linked to socioeconomics — household income, education, job and income security, safe and clean physical environments in the home and in our neighborhoods. And as the RWJF/NPR/Harvard Chan study shows, these social determinants risks travel in groups and double-down on those health risks for people who rent, people of color, those without access to healthy food, and folks who earn lower incomes.
 At the same time, the coronavirus pandemic accelerated the trend-already-in-place at the start of 2020 with our homes evolving into our health care spaces: ideally hygienic, safe, with nutritious food in the fridge, and connected online.
At the same time, the coronavirus pandemic accelerated the trend-already-in-place at the start of 2020 with our homes evolving into our health care spaces: ideally hygienic, safe, with nutritious food in the fridge, and connected online.
This month’s announcement launching the Advanced Care at Home Initiative bolsters this phenomenon. This alliance brings together the founding members Kaiser Permanente, Mayo Clinic, and Medically Home joined by new stakeholders including Adventist Health, ChristianaCare, Geisinger Health, Integris, Johns Hopkins Medicine, Michigan Medicine (University of Michigan), Novant Health, ProMedica, Sharp Rees-Stealy Medical Group, UNC Health, and UnityPoint Health.
One of the founding members Dr. Stephen Parodi of The Permanente Foundation noted, “Offering acute-level, hospital-quality care at home allows physicians and care teams to treat a whole person to meet their individualized care goals, while also helping address some of the social determinants of health….[and] supports a policy foundation for this more equitable future of health care.”
As we are amazed and exuberant about the digital future of health care this week at HLTH, let’s keep health — equitable, accessible, culturally compatible, high-value — in our hearts and minds.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...