Delivering health care during the heights of the COVID-19 pandemic proved to both patients and their clinicians that virtual care was not only a viable channel for care, but very often a preferable “place” to collaborate for treatment.
Even before the coronavirus pandemic emerged in early 2020, telehealth and the hospital-to-home movement were beginning to become part of a portfolio of delivery modes across the continuum of care. Deloitte spells out the current and future prospects for the Hospital in the future “without” walls in a new report that spells out driving forces, future scenarios, and impacts on a business long defined by inpatient beds.
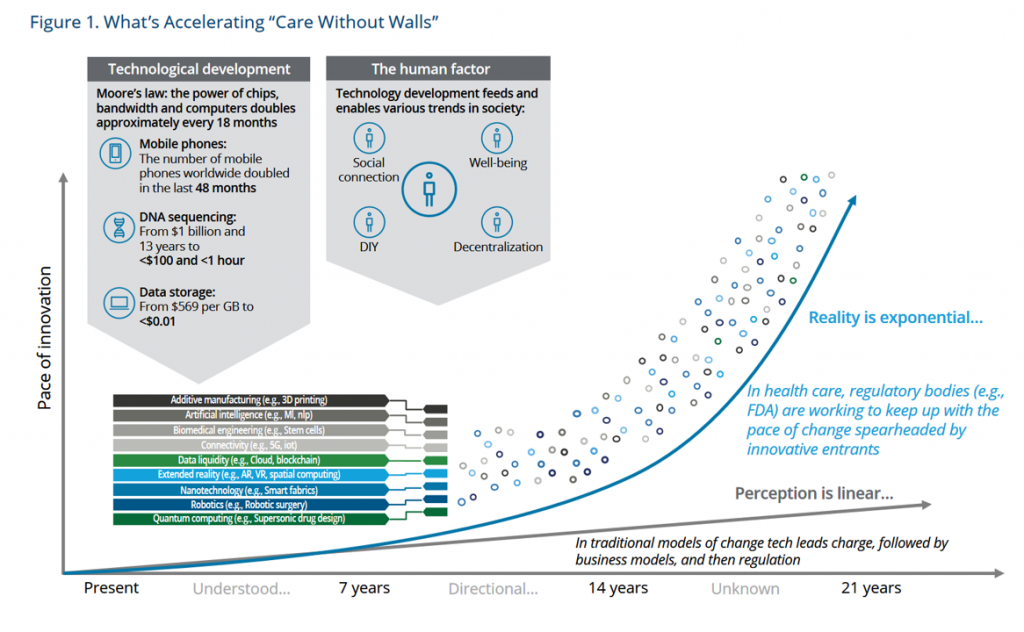
Several factors are accelerating “care without walls,” Deloitte notes, shown in the first graph.
These enablers include,
- Technology, such as the proliferation of mobile phones, DNA sequencing, and fast-declining data storage costs – all examples of Moore’s Law; and,
- Human factors, with technology enabling social connectivity, well-being, decentralization, and DIY (which I detail in my book, Health Citizenship).
Note the many technology components that underpin innovation, such as AI, connectivity (say, 5G), data liquidity (via cloud or blockchain), extended reality (ER, covering AR, VR, and spatial computing), and robotics, among other tech developments.
Taken together, these accelerators disrupt the traditional physical hospital’s role in at least six ways: via,
- Care delivery transformation, defined holistically including well-being across physical, mental, social, emotional, financial, and spiritual health
- Digital transformation, built on “radically interoperable” data on open, secure platforms
- Medical technology, with prolific sensors and devices that connect consumers, patients, and caregivers across the continuum from healthy to high-risk acute patients (that’s the Hospital@Home segment of people)
- Health equity, sustainability, and the environment (the ESG + H factors)
- The future of the workforce (attending to both clinician burnout and human capital sustainability and new roles that can extend providers’ expertise allowing folks to operate at the top of their licenses); and
- The future of regulation for medical, digital health, pharma, and other areas requiring risk-management.
Compared with care delivery in 2022 in much of the developed world, care is organized around the needs of providers, suppliers, plans, and payers…not consumers, patients and caregivers. Consumers are a growing force demanding health care on human, personalized terms akin to services received in other industry sectors in daily life.
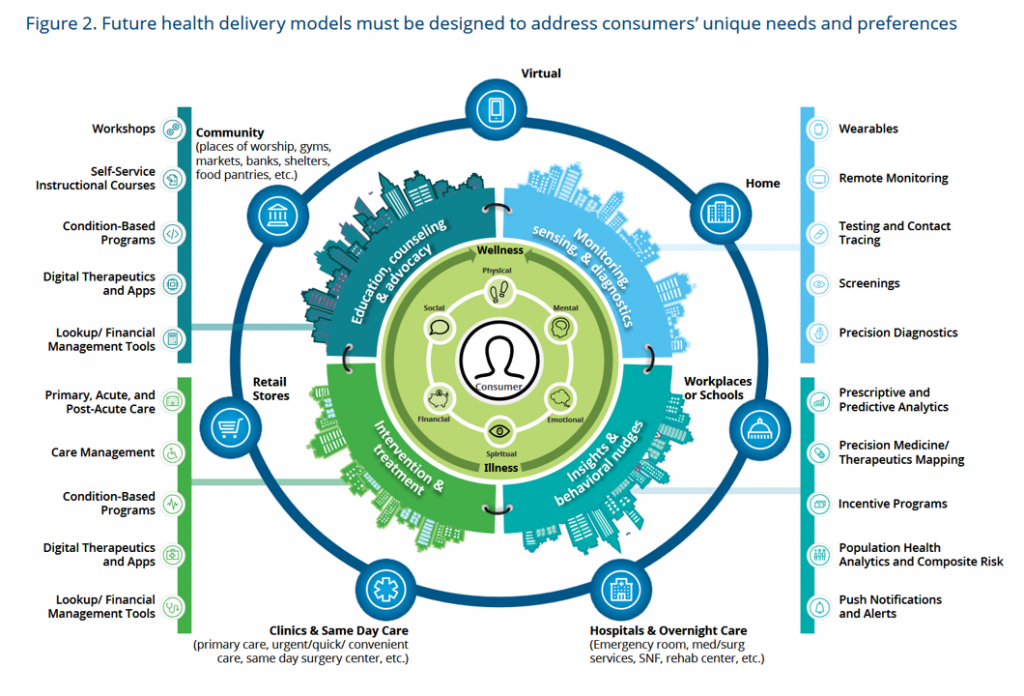
Health Populi’s Hot Points: The third image, titled “Figure 2” from the Deloitte report, details numerous care delivery models, enablers, and workflows that should be designed based on consumers’ needs and preferences.
That person is at the center of the diagram, surrounded by her personal definitions of health across the dimensions of physical, mental, emotional, spiritual, financial, and social.
Based on a person’s preferences — one’s sense of values and “value” in terms of ROI for time, money, effort expended — care should be designed and delivered in various sites deploying various workflows and tools that suit the patient-consumer’s condition and personal preferences.
The Deloitte report provides two scenarios of patient journeys based on individual’s demands, for congestive heart failure and diabetes. In both of these cases, there are digital health tools and apps that can be enchantingly designed for consumers to use in daily life-flows that enable DIY self-care to improve outcomes and enhance quality of life.
And these life-flows happen at home and on-the-go, in partnership with health care providers who play a greater role in health coaching and nudging via text message or phone call to help people stay on-track and engaged in collaborating for health-making.
There are many assumptions under this model, and Deloitte understands this won’t or can’t happen overnight. Regulation lags behind the promise of “exponential” innovation, along with risks of determinants of health such as lack of connectivity and health literacy, as well as bias in AI and unconscious behaviors on the part of clinicians and researchers, among others.
Furthermore, as we have seen with innovations in “e-health” and “m-health,” many regions that have had the least-developed physical infrastructure have leapfrogged ahead of “established” healthcare system with tremendous sunk costs in buildings and big-iron technologies. Incentives, regulations, and reimbursement regimes have led to entrenched interests that today could slow down innovations for hospitals without walls and more care delivered in the community, at work, and at home.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...