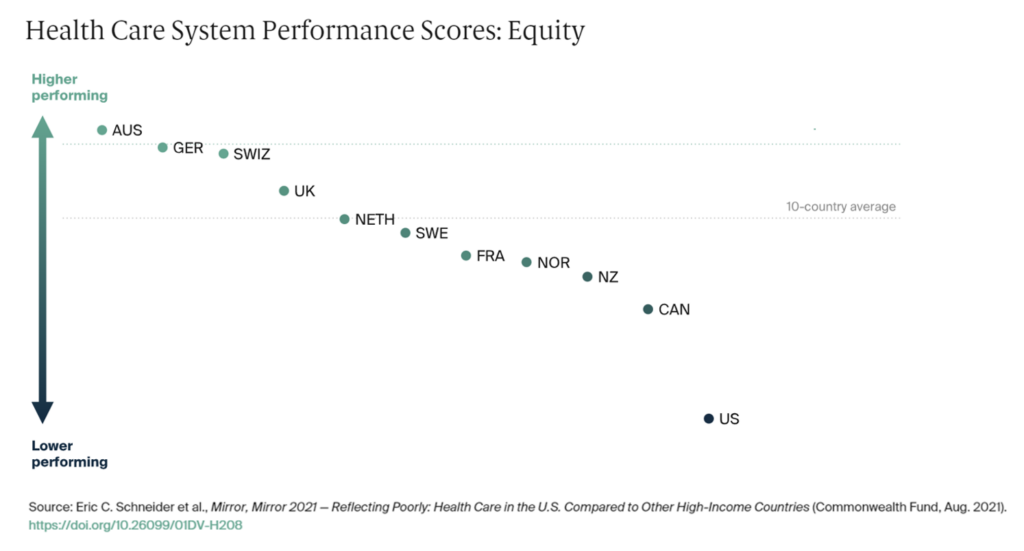
The U.S. spends more on health care than any other nation in the world. Yet Americans’ health outcomes rank relatively low compared with other wealthy peer nations on Planet Earth, manifesting a low return-on-investment for this huge financial spend.
Nowhere is this more evident than in America’s place in equity compared with nine countries, shown in the graph on health care system performance from The Commonwealth Fund’s perennial study, Mirror, Mirror – the latest version of which was subtitled, “reflecting poorly” on health care in the U.S.
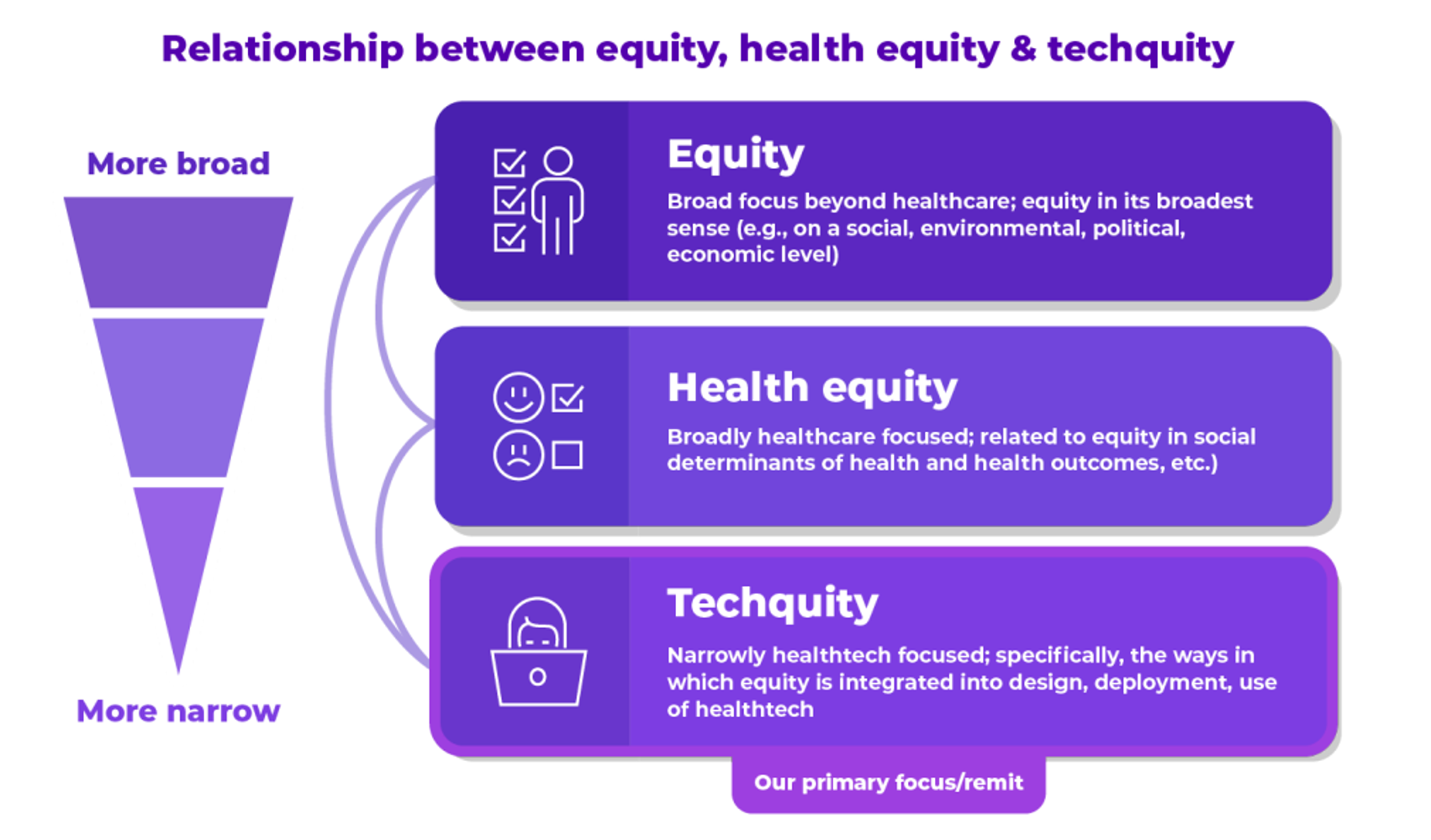
Equity is an over-arching concept that the health care ecosystem has begun to embrace as a key metric for what looks good (or not) in U.S. health care.
This week at the VIVE 2023 conference, the HLTH Foundation, collaborating with Ipsos, published a report on Techquity in 2023, analyzing survey data collected from 212 respondents from 200 health care organizations.
For context in using this dataset, the folks responding to the study came from the HLTH and CHIME email lists; those on these lists may already be well aware of the concept of “techquity,” and certainly health equity. As a benchmarking survey conducted among a community of folks somewhat more clued-into the concepts being discussed, it offers us important insights into what this group of health industry leaders is thinking about — ahead of the mainstream, but directionally instructive for our understanding of the overall issues and where we are on the adoption curve of equity and its many layers — equity overall, health equity, and “techquity.”
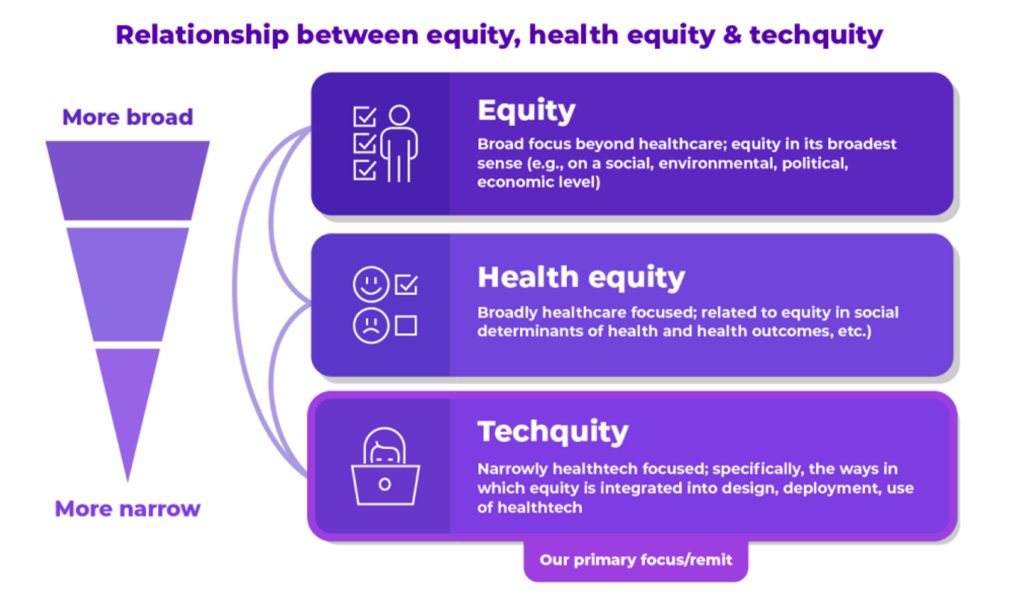
Start with the definition set forth in the report: that techquity is the “intentional design and deployment of technology both to advance health equity and to avoid depending existing systemic inequities and health disparities.”
Importantly and pragmatically, this definition includes both the technology deployed and the data practices implemented when using technologies.
The concept of techquity is built on four pillars in this research:
- Trust in the technology
- Access to the technology
- Initial use or adoption of the technology, and
- Sustained engagement with the technology.
The term “techquity” was new to one-half of the respondents. Once the term was explained in the survey interviews, the majority of people understood the concept.
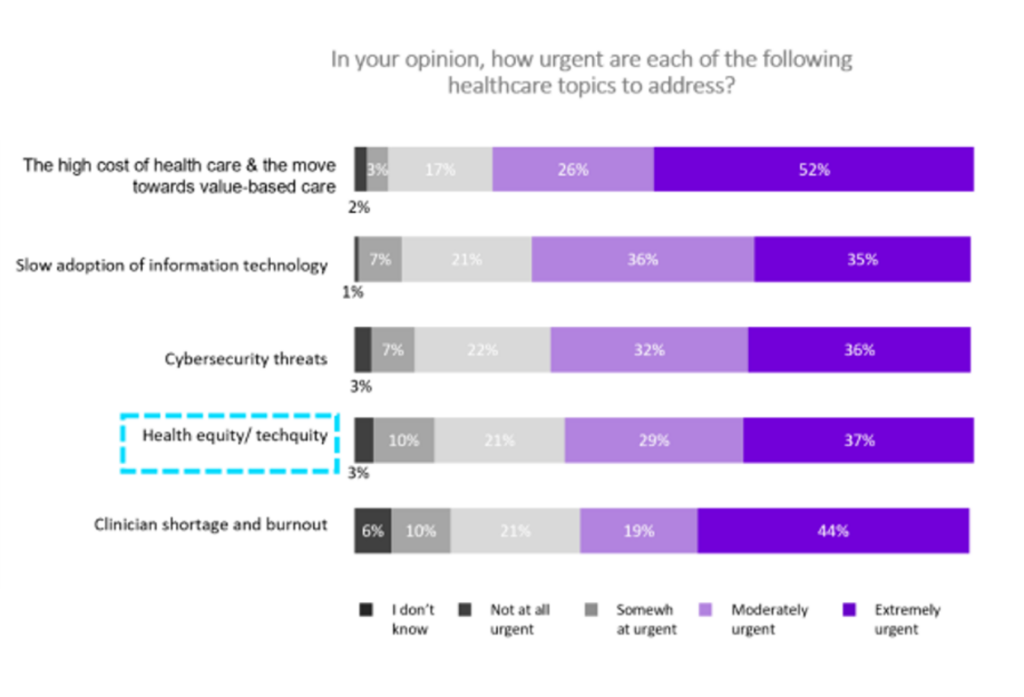
However, as the first bar chart illustrates, techquity fell below other priorities on leaders’ minds — namely the high cost of care and the move to value, 4 in 5 people calling as “urgent” (net moderately + extremely).
Second in priority for this audience was the slow adoption of information technology (among 71%), followed by cybersecurity threats which tied with health equity and techquity among about 2 in 3 respondents — still urgent, along with clinician shortage and burnout challenges which ranked a very close 5th place for urgency.
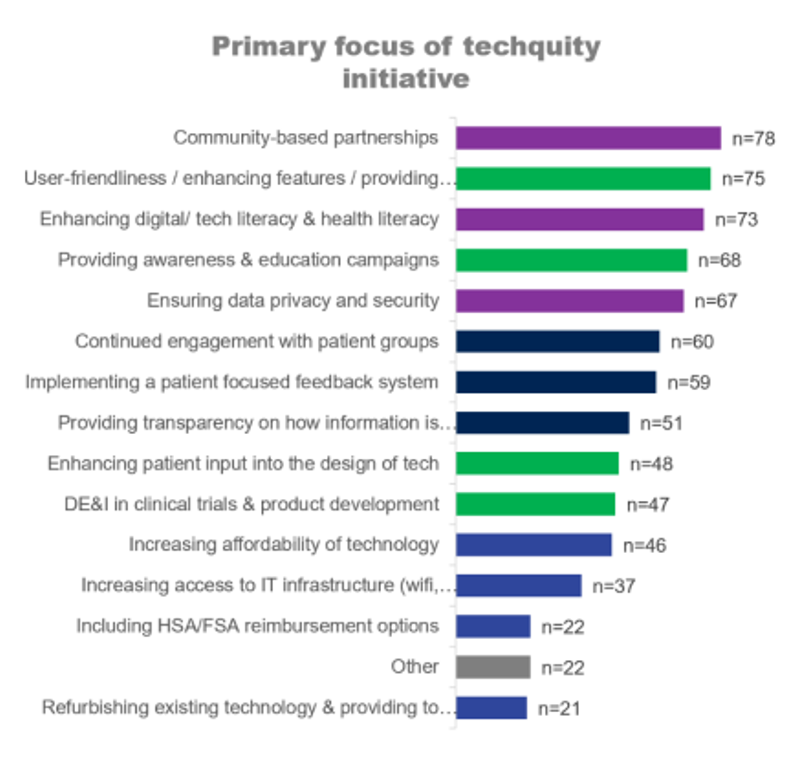
Among those folks who have embraced techquity in their organizations, they tend to support a specific group of people or a community – most notably, Medicare, Medicaid, rural geographies, and BIPOC communities.
Key focuses of the techquity “pioneers” initiatives have addressed community partnerships, the user-friendliness of health technology, addressing literacy, educating via awareness campaigns, and ensuring data privacy and security. You can see other initiatives listed in the bar chart here.
It is too early to assess the effectiveness of these initiatives. But we should be mindful in the current economic uncertain environment that investments in techquity may be constrained, an opinion held by over one-half of the survey respondents.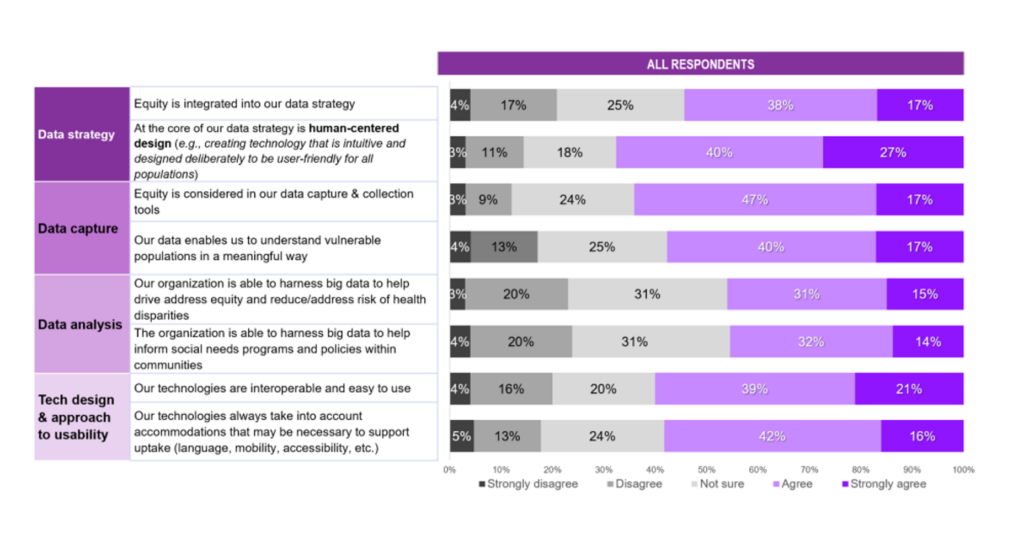
Health Populi’s Hot Points: Trust is the first pillar of techquity: trust is also the precursor for patients’ health engagement, we’ve learned from the earliest research into patient engagement and activation, from the first Edelman Health Engagement Barometer to the research of Judith Hibbard and most recently, the Edelman Trust Barometer.
Weaving together the data in the last chart from the Techquity report makes clear the value of equity-by-design.
As I introduced the report above, I noted that VIVE and Ipsos bundle both the technology and data practices into the techquity-concept. This was embraced by about one-half of respondents who agreed with the survey question that “equity is integrated into our data strategy.”
Human-centered design was also part of the thinking among two-thirds of respondents in this study.
We have a lot of work to do on this: as the study was conducted among more of the techquity/health equity cognoscenti, equity-by-design and its tactical calls-to-action must be baked into the plans of those charged with delivering on the promise of health equity — from data strategy and capture to analysis and usability design.
Thanks to the HLTH Foundation, #VIVE2023, and Team Ipsos for bringing these insights into the benchmarking research.




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...