At this moment, the healthcare job I’d least like to have is that of a non-profit hospital Chief Financial Officer (CFO). Five news stories, published in the past 24 hours, tell the tale:
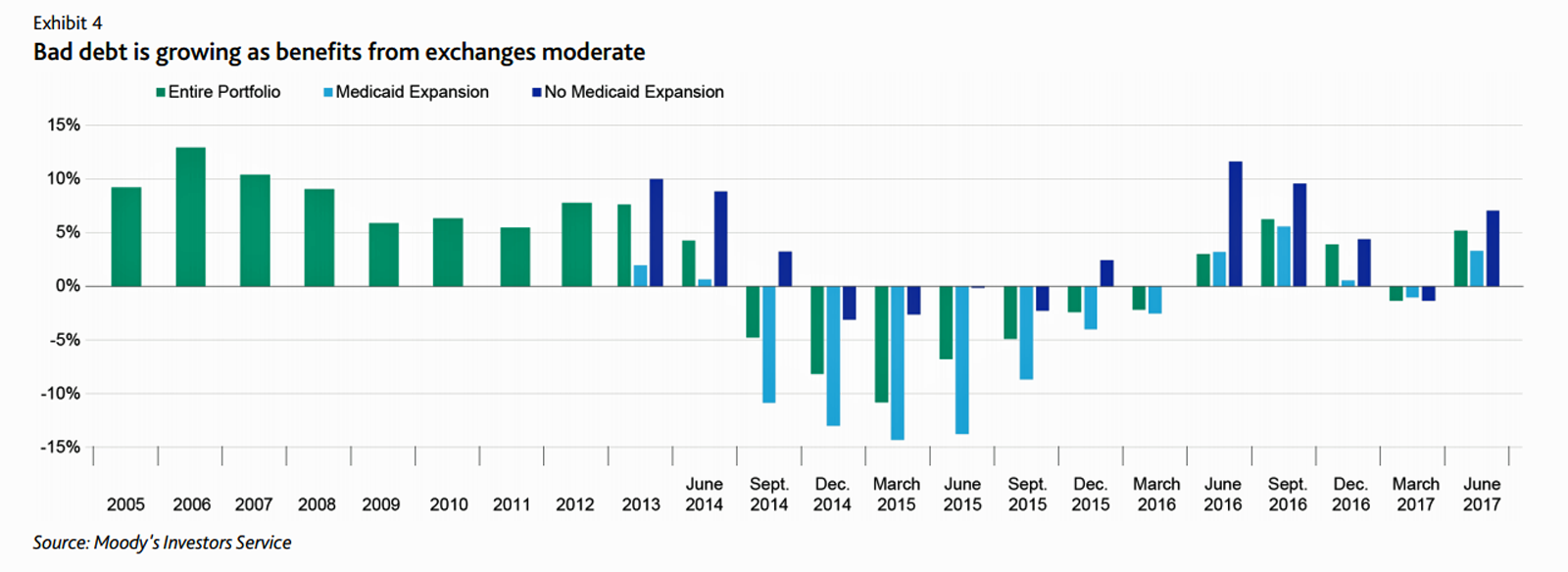
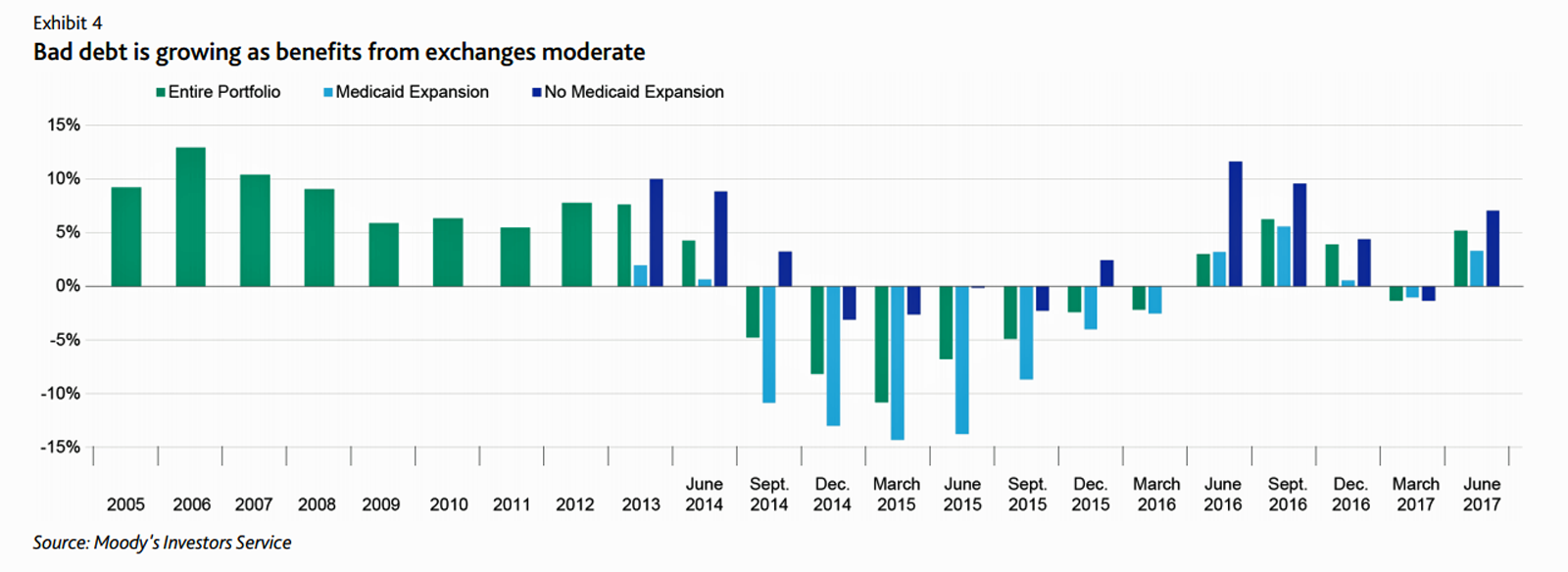
First, Moody’s forecast for non-profit hospitals and healthcare in 2018 is negative due to reimbursement and expense pressures. The investors report cited an expected contraction in cash flow, lower reimbursement rates, and rising expense pressures in the midst of rising bad debt.
 Second, three-quarters of Federally Qualified Health Centers plan to lay off staff given lack of budget allocations resulting from Congressional inaction. Furthermore, if the $3.6 bn in funding is not immediately restored, researchers from Milken Institute School of Public Health from George Washington University calculated, jobs lost in 2018 could range from 76,000 to 161,000 across the U.S. This would then ripple to a state economic loss of $7.4 bn to $15.6 bn in gross state economic product. Because health centers are sited in every U.S. state, the negative economic impact would impact the entire nation’s Governors and state budgets.
Second, three-quarters of Federally Qualified Health Centers plan to lay off staff given lack of budget allocations resulting from Congressional inaction. Furthermore, if the $3.6 bn in funding is not immediately restored, researchers from Milken Institute School of Public Health from George Washington University calculated, jobs lost in 2018 could range from 76,000 to 161,000 across the U.S. This would then ripple to a state economic loss of $7.4 bn to $15.6 bn in gross state economic product. Because health centers are sited in every U.S. state, the negative economic impact would impact the entire nation’s Governors and state budgets.
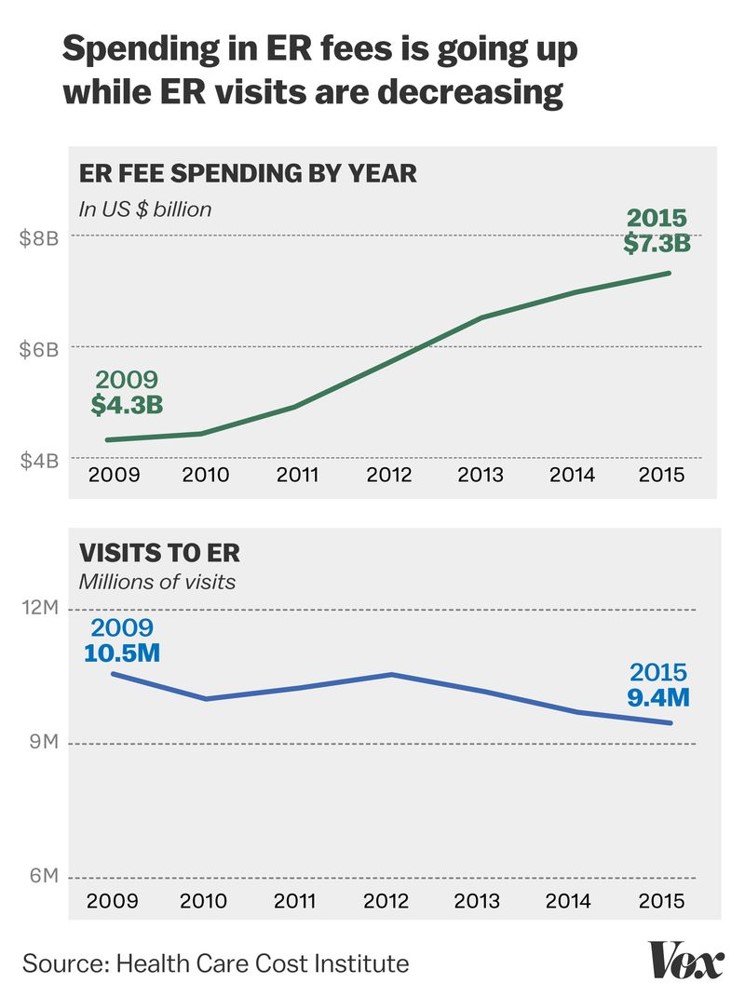 Third, emergency room spending nearly doubled between 2009 and 2015, although visit volume fell by over 1 million visits, Sarah Kliff reported in Vox today in a column titled, “Emergency rooms are monopolies. Patients pay the price.”
Third, emergency room spending nearly doubled between 2009 and 2015, although visit volume fell by over 1 million visits, Sarah Kliff reported in Vox today in a column titled, “Emergency rooms are monopolies. Patients pay the price.”
Fourth, the Commonwealth Fund’s Dr. David Blumenthal sees the erosion of the employer-sponsored health insurance market. “New data suggest that job-based health coverage provides far less protection to U.S. workers and their dependents than it once did,” which we’ve been observing here on Health Populi since our inception ten years ago. Dr. Blumenthal succinctly puts the situation as, “declining generosity.” The abridged version is that health care costs have increased much faster than workers’ wages. In recent years, though, health insurance premiums have grown more slowly, but employers have not shared cost savings with employees.
Fifth, the Children’s Health Insurance Program (CHIP) has yet to have its funding renewed by Congress, causing some states to alert CHIP families to the fiscal reality that they should begin research private health insurance options. While CHIP has had strong bipartisan support since it began in 1997 — jointly created by Democrat Edward Kennedy of Massachusetts and Republican Orrin Hatch of Utah — the 115th Congress today can’t agree how to pay for health for nine million American kids who have depended on it for a decade.
Finally, and sixth, to the patient-as-payor perspective: most consumers can’t find healthcare price information online, which makes it difficult for patients without health insurance or those in high deductibles to estimate what a health service will cost before receiving it. This research was published by a team from Duke’s Margolis Center for Health Policy in JAMA Internal Medicine.
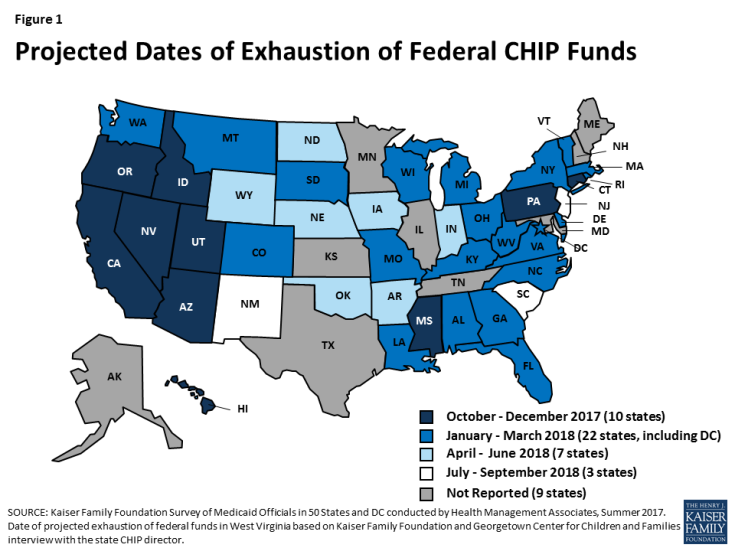 Health Populi’s Hot Points: Play out the logic, connect the dots, and do the simple math. Expect more Americans to visit hospital ERs due to lack of an on-ramp to primary care, for unpaid bills to increase at non-profit hospitals, and for their CFOs to face ever-growing bad-debt burdens.
Health Populi’s Hot Points: Play out the logic, connect the dots, and do the simple math. Expect more Americans to visit hospital ERs due to lack of an on-ramp to primary care, for unpaid bills to increase at non-profit hospitals, and for their CFOs to face ever-growing bad-debt burdens.
Moody’s, have your green eye shades and calculators at the ready. You may well be re-defining what a “negative outlook” for healthcare providers, hospitals and physicians, really looks like for 2019.




 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.