Happy anniversary to me…well, to the Health Populi blog! It’s ten years this week since I launched this site, to share my (then) 20 years of experience advising health care stakeholders in the U.S. and Europe at the convergence of health, economics, technology, and people.
To celebrate the decade’s worth of 1,791 posts here on Health Populi (all written by me in my independent voice), I’ll offer ten health/care milestones that represent key themes covered from early September 2007 through to today…
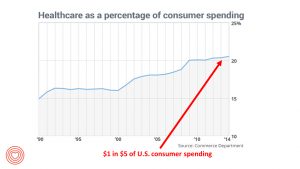 1. Healthcare is one-fifth of the national U.S. economy, and the top worrisome line item in the American family’s pocketbook. You can read more about this in Health Populi from day 1 in 2007 to late August 2017 with more evidence that health care costs are top-of-mind for U.S. health citizens. For the immediate future, patients will assume a greater share of health care spending given employers’ growing adoption of consumer-directed health plans — high-deductibles coupled with health savings accounts.
1. Healthcare is one-fifth of the national U.S. economy, and the top worrisome line item in the American family’s pocketbook. You can read more about this in Health Populi from day 1 in 2007 to late August 2017 with more evidence that health care costs are top-of-mind for U.S. health citizens. For the immediate future, patients will assume a greater share of health care spending given employers’ growing adoption of consumer-directed health plans — high-deductibles coupled with health savings accounts.
2. The Affordable Care Act worked to get health insurance to millions of uninsured Americans. But there is more work to do, and this week Congress re-convenes with some evidence of green shoots of bipartisan cooperation to fix, not repeal, the ACA. American workers highly value their health benefits, well-knowing how much it could cost them to fetch health plans on the individual market. As President Trump recently cut the Federal ACA budget for communicating health insurance marketplace options, the U.S. faces a situation where the nation’s President may be mindfully contributing to Americans’ reduced access to being health-insured by reducing access and on-ramps to consumers’ needed information. But State and local insurance navigators are working to fill this gap.
3. Sticker-shock is a mainstream reaction for American patients who fill branded prescription drugs. The course of a drug treatment to cure Hepatitis C reached $98,000 in 2014. The retail price of an EpiPen, $500 in 2016, driving angry patients in New York City to protest in front of Mylan’s offices. The latest entry into the pharma cost Hall of Fame is Kymriah, a new-new gene therapy treatment for treating young people with acute lymphoblastic leukemia, approved by the FDA last week. ALL is the most common form of cancer in young people. The list price will be $475,000 for a one-time treatment. Lowering the cost of prescription drugs is one health reform issue Americans across the political spectrum agree on.
for American patients who fill branded prescription drugs. The course of a drug treatment to cure Hepatitis C reached $98,000 in 2014. The retail price of an EpiPen, $500 in 2016, driving angry patients in New York City to protest in front of Mylan’s offices. The latest entry into the pharma cost Hall of Fame is Kymriah, a new-new gene therapy treatment for treating young people with acute lymphoblastic leukemia, approved by the FDA last week. ALL is the most common form of cancer in young people. The list price will be $475,000 for a one-time treatment. Lowering the cost of prescription drugs is one health reform issue Americans across the political spectrum agree on.
4. Most patients’ personal health information has moved from manila paper folders with hand-written notes to digitized, electronic health records. Most patients want to connect with their physicians using digital means, but privacy concerns remain. Trust must be earned to garner health engagement, as I recently discussed in light of Aetna’s breach of peoples’ HIV status in a mailed letter. Still, we know from research via the PatientsLikeMe community and other patient social networks that people managing serious diseases are willing to share personal health information when there is a value-exchange.
5. More personal health information is being generated through wearable technology. In the past decade, I’ve attended the annual CES (the acronym once fully called out as the Consumer Electronics Show). Beyond big-screen TVs and tricked-out cars, one of the fastest-growing areas at CES is digital health. While Fitbit wrist bands and Withings Wi-Fi scales represented the early generation of wearable tech for health (or mHealth), shiny new things are emerging via Apple Watch and heart-activity enhancements that are gathering data that’s getting stored in clouds (Amazon Web Services and Apple to Samsung and dozens of others). Data are mashed into algorithms that can then inform patients, consumers, caregivers, and clinicians to coach and inform decisions.
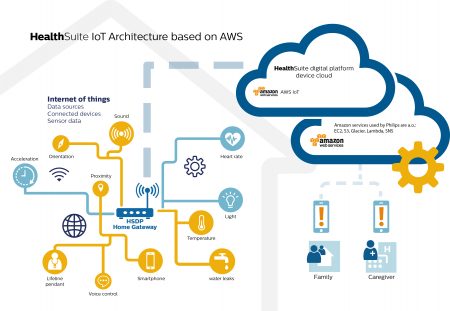 6. Beyond wearing tech, our homes and autos (the so-called “third space”) are getting filled with “things” in the growing Internet of Things environment. Light bulbs, washing machines, refrigerators and, of course, voice-powered digital assistants (THINK: Amazon Echo and Alexa) have begun to collect data on our daily habits, and health is already growing its IoT chops.
6. Beyond wearing tech, our homes and autos (the so-called “third space”) are getting filled with “things” in the growing Internet of Things environment. Light bulbs, washing machines, refrigerators and, of course, voice-powered digital assistants (THINK: Amazon Echo and Alexa) have begun to collect data on our daily habits, and health is already growing its IoT chops.
7. Virtual health and telehealth have passed a tipping point for adoption. This very minute as I write this post, telehealth technology is helping thousands of people in Texas hurt by Hurricane Harvey get needed healthcare and medical attention sooner rather than later.
8. Health is social. Health is contagious. So are negative health behaviors. The research of Christakis and Fowler published in their book, Connected, demonstrates that people can kick-off a virtuous cycle of health for themselves that influences not only their immediate social network of friends and family, but positively influences their networks further out in the social web. This is at the root of public health: we are our brothers’ and sisters’ keepers, and this is the evidence for why social determinants of health are so powerful in communities. Loneliness is also a social determinant of health, as I wrote here about new research into our purpose and our wellness.
9. Health disparities continue to mar American health care. People of color and lower-income people have worse health outcomes, and for many conditions and procedures, less access to the latest evidence-based standards of care. This year marked 50 years since the 1967 Detroit riots, and 70 years since the Nuremburg Code emerged. Health care in the U.S. must confront these health inequities and bring greater “health symmetry” to all health citizens in the nation. Aside from issues of justice, a healthy citizenry is a productive one that generates tax revenue for a nation.
 10. Patients are morphing into health care consumers, seeking transparency, management tools, information, and support from both health industry players and from each other, in peer-to-peer networking. Amazon has “primed” health care consumers, and will be taking its place among the new entrants helping to improve peoples’ health care experiences. Consumers’ most recent excellent experience in retail defines their current benchmark for expectations in all sectors — including health care.
10. Patients are morphing into health care consumers, seeking transparency, management tools, information, and support from both health industry players and from each other, in peer-to-peer networking. Amazon has “primed” health care consumers, and will be taking its place among the new entrants helping to improve peoples’ health care experiences. Consumers’ most recent excellent experience in retail defines their current benchmark for expectations in all sectors — including health care.
I must thank two colleagues who first inspired me to launch the Health Populi blog: Matthew Holt and Bob Laszewski. Matthew, who founded The Health Care Blog in 2003, was my first close colleague to blog about health care. He provided early counsel to me on two issues: finding my authentic voice (which he certainly has), and warning against allowing the blog to be a major time-suck in daily life. Bob, a Washington, DC-based health policy expert, set an example of authenticity, passion, and fact-based reporting in his blog, Health Care Policy and Marketplace Review, founded in 2006.
 Health Populi’s Hot Points: The ten milestones listed here drive home several things “I know that I know,” learnings I’ve derived from my many years of working with clients across the health and healthcare landscape — traditional healthcare organizations and suppliers (hospitals, physicians, health plans, medical device, and pharmaceutical companies) to newer entrants including consumer goods, food, electronics, and financial services, among them.
Health Populi’s Hot Points: The ten milestones listed here drive home several things “I know that I know,” learnings I’ve derived from my many years of working with clients across the health and healthcare landscape — traditional healthcare organizations and suppliers (hospitals, physicians, health plans, medical device, and pharmaceutical companies) to newer entrants including consumer goods, food, electronics, and financial services, among them.
Healthcare is morphing toward health/care in a landscape where healthcare providers and traditional stakeholders (plans, suppliers, pharma) must inter-operate with new entrants — from Amazon to ZocDoc. That’s a good thing, because heath care consumers want care served up how and where we want it — and provided in a value-based framework. In that context, let me tell you what I know I know:
Noncommunicable diseases – heart, diabetes, cancers, among them – will kill most of us in 2017. These conditions are largely amenable through self-care and lifestyle changes such as quitting smoking, eating nutritious foods in right-sized portions, taking more activity and exercise, and moderately drinking alcohol.
To ensure healthy health citizens, spending money and labor on the social determinants of health are more important, dollar for dollar, than specialized tertiary healthcare services. See this article just published in the aftermath of Hurricane Harvey, on why investing in prevention, broadly writ, is crucial for a healthy nation. [It’s written by one of my favorite public health policy folks, Dr. Sandro Gallea.]
(Good) food is medicine. Starting people in life with nutrition, pre-natally and ongoing, is a huge health boost and a key social determinant of health for a lifetime. [My friends at SquareRoots, with whom I collaborated on a maternal and child health panel at CES 2016, are working on this.]
Mental health is core to overall health and well-being, just like heart health, gut health, bone health, and oral health. Bundling mental health into primary care would help improve America’s behavioral health crisis….coupled with greater resource allocation toward social care away from more expensive specialty healthcare spending.
The world’s developed countries that have invested in strong primary care backbones (supply of physicians, nurses, and other primary care provider types) have patients with better health outcomes. The U.S. spends relatively less per capita on primary care than these other countries, and our health outcomes fall well below those in Denmark, France, and even the UK — which spends far less per person on healthcare than the U.S. does.
As I look toward the next ten years of my work, trend-weaving and writing, I expect our houses (whether single family, apartment, or Tiny) will evolve into our true medical homes, where we take on greater self-care enhanced through Internet of Things, artificial intelligence, and enhanced health literacy. What will underpin this is greater attention to designing care processes, “things,” and experiences that speak to peoples’ own health literacy, values and preferences. “Personalized medicine,” in terms of genomics, has gained a lot of attention and resources. A greater focus and resourcing toward “personalized health” that accounts for our individual values and belief systems, socioeconomic status and preferences, will bolster health outcomes for all health citizens in the U.S.





 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...