Almost from the first year of launching Health Populi in 2007, I’ve written a “TrendCast” for the coming year of health care. Over many years, there weren’t so many blogs devoted to health care which featured such prognostications, and so readers could divine signal from noise and move forward into new years with manageable lists of What To Expect Next Year in Healthcare.
Here’s one from ten years ago that brings a sense of déjà vu: most of the findings are consistent with what we know for sure about 2026 and it’s useful to look back with today’s eyes to understand why so many aspects of U.S. healthcare have been slow to change. 
Today I have a full inbox and file on my hard drive of 2026 forecasts, at least three dozen of them, and my intent was to review the best of them and share with you my Top 10 Tea Leaf Reads among them. But I have a better idea, given the State of Our Health/Care World — and my own demands from clients and colleagues for how to consider so many uncertainties accompanying us into 2026.
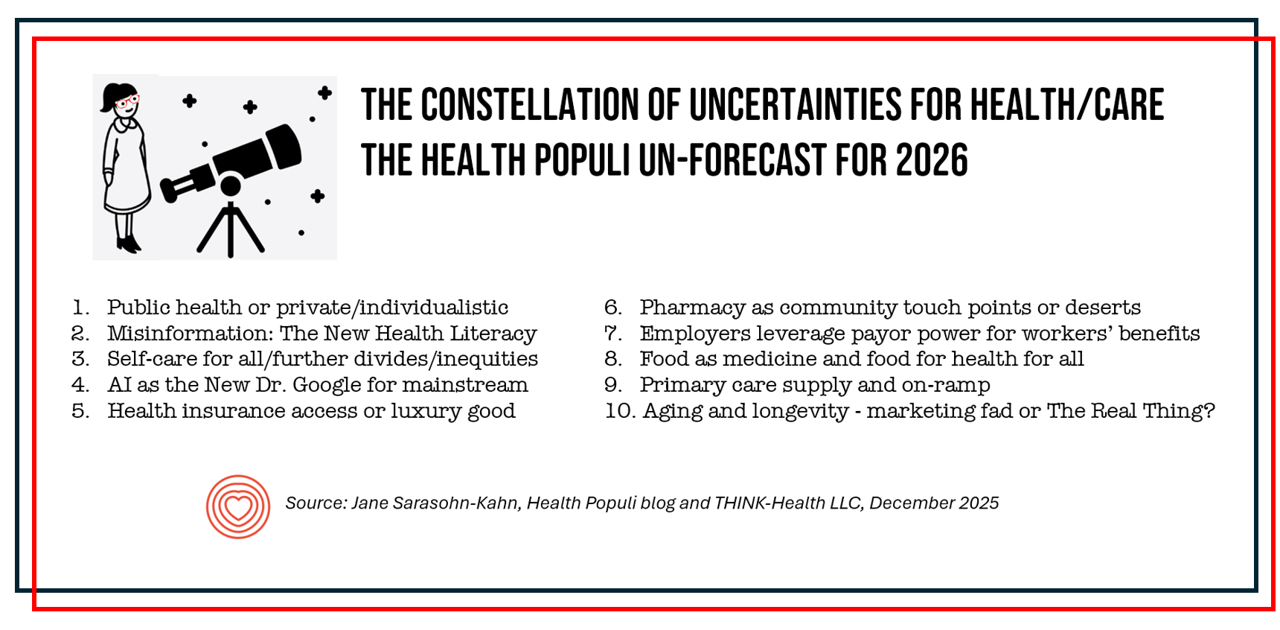
So welcome to my first UnForecast of Uncertainties: in scenario planning parlance, these are the known un-knowns. These apply to the entire ecosystem of health/care in the U.S.; some will be useful for the rest of the world but should be translated into local markets based on unique regimes for health system financing, delivery, regulation, and health citizen differences (whether demographic, fiscal, or social.
For context, I turn to Dr. Seuss’s protagonist in the classic strategic planner’s guide titled I Had Trouble In Getting to Solla Sollew.
I’ve used this Dr. Seuss deep cut for much of my career in conducting scenario planning projects, and it’s never failed to inspire teams engaging in futures work. The general theme is to confront obstacles and challenges in real-time and not avoid them…but also to recognize the nature of those obstacles can vary and may require good deal of patience and self-agency.
Our protagonist reminds us that “to be twice as careful and twice as smart,” we must “watch out for trouble in front and back sections by aiming” our “eyeballs in different directions.” 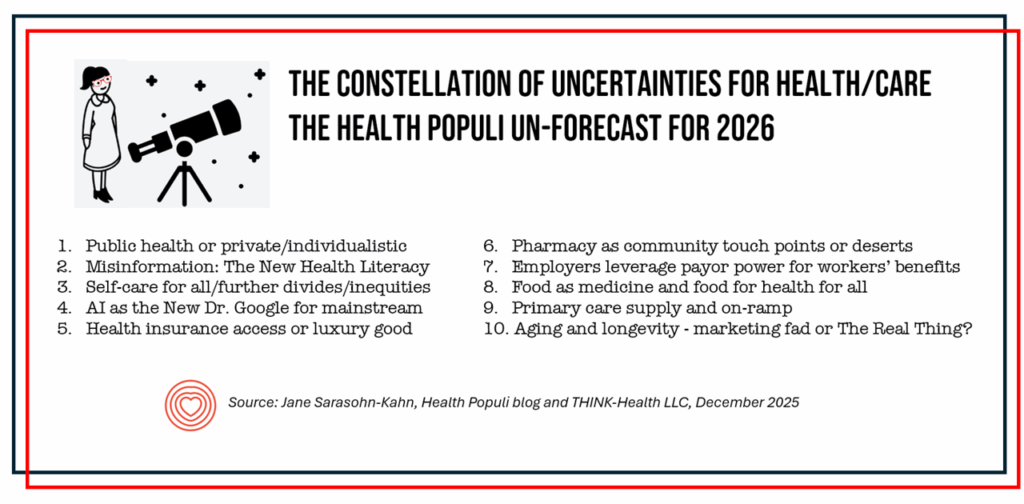
With these thoughts in mind, here are the “different directions” for your Uncertainties inventory, health/care planning v, 2026:
1. Public health or private/individualistic. For more on this uncertainty, check out my scenario planning exercise using it as a key future factor.
2. Misinformation and the New Health Literacy. Here, consider a new take on health literacy using authentically-voiced and -intended storytelling from colleagues at my alma mater, University of Michigan.
3. Self-care for all or self-care divides/inequities. Consider techquity issues (say, with respect to wearables and self-tracking accessibility) and what’s relevant to the individual in terms of both value and values.
4. AI as the New Dr. Google for mainstream consumers. My recent post on the topic may be helpful to you on DTC/AI for health care).
5. Health insurance access vs. health insurance as luxury good. We’re in the midst of not-knowing what may happen with ACA premium supports, today “knowing” they’ll be gone until they may not be based on Congress’s return to work in the new year. We know in this moment millions of Americans won’t be able to afford or be willing to pay the full retail cost burden of health insurance for individuals and families, based on the latest KFF consumer poll. I’ve been tracking self-rationing due to cost since my early health economics days; here’s a recent riff on the challenge.
6. Pharmacy as community touch points or pharmacy deserts. I’ve witnessed the power and equity-access of community/retail pharmacies for people lacking usual sources of primary care. With many storefronts closing (e.g., RiteAid) and hours reducing, stay tuned to the market status of this important source for self-care and family medical care. Another uncertain factor for consumer-facing pharmacy will be how the Trump Administration approach to Most-Favored-National medicines pricing, the launch of the TrumpRx platform, and the influence of Mark Cuban’s Cost Plus Drug organization could potentially lower patient-facing costs of prescribed medicines. Finally, what other Rx categories might pharmaceutical companies add to their direct-to-patient platforms (e.g., Lilly Direct, PfizerForAll, et al.)?
7. Employers leverage their payor power for workers’ benefits (and medical costs). Read this latest update from The Conference Board for a current primer.
8. Food as medicine and food for health for all…or not. Mainstream consumers, whether Walmart or Whole Foods shoppers, are all-in when it comes to food sourcing for health benefits — from energy boosting and sleep-promoting to managing chronic conditions. But with the erosion of SNAP benefits and growing demand for food pantry supplies, what might develop in 2026 to assuage this challenge for a key driver of health? And how might the growing DTP-consumer-driven adoption of GLP-1 medicines change demand for food, grocery store shopping, and other aspects of the consumer economy?
9. More health care professionals look for the Exit: where’s the primary care on-ramp?
10. Aging and longevity – marketing fad or The Real Thing? (On this score, I am finding a series written by Andy Miller, SVP Innovation & Product Development and AgeTech lead at AARP, super-insightful. In particular, his observation that “Longevity is a stack and not a vertical” presents a well-formed, actionable thesis).
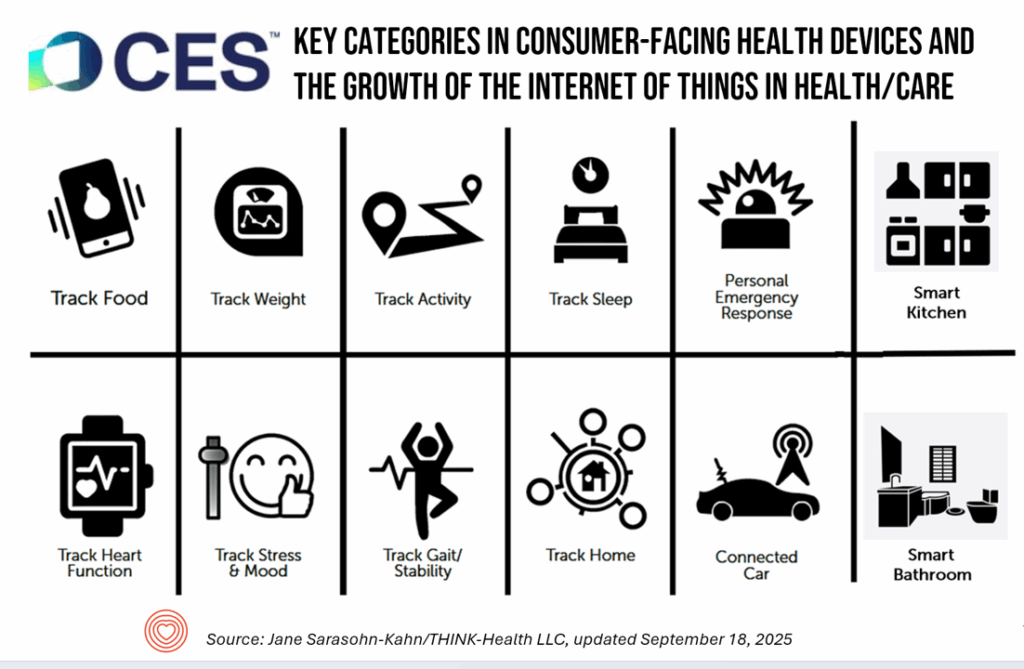
I’ll be sorting out the subtexts for each of these, and other, market factors right after popping our prosecco cork, bound for CES 2026 for a full week of meetings in Las Vegas. For now, these issues will be top-of-mind in my own workflows and discussions, refining along the journey as I explore the consumer’s growing role in their own health, the health of loved ones for whom they care, and their communities.
Everyone — may you be well, be at peace, be open to love, laughter & community…Jane S-K




 I'm once again pretty gobsmackingly happy to have been named a judge for
I'm once again pretty gobsmackingly happy to have been named a judge for  Stay tuned to Health Populi in early January as I'll be attending Media Days and meeting with innovators in digital health, longevity, and the home-for-health during
Stay tuned to Health Populi in early January as I'll be attending Media Days and meeting with innovators in digital health, longevity, and the home-for-health during  Jane collaborated on
Jane collaborated on