Consumers’ Trust In Health And Personal Care Stores: The Growing Retail Health Ecosystem
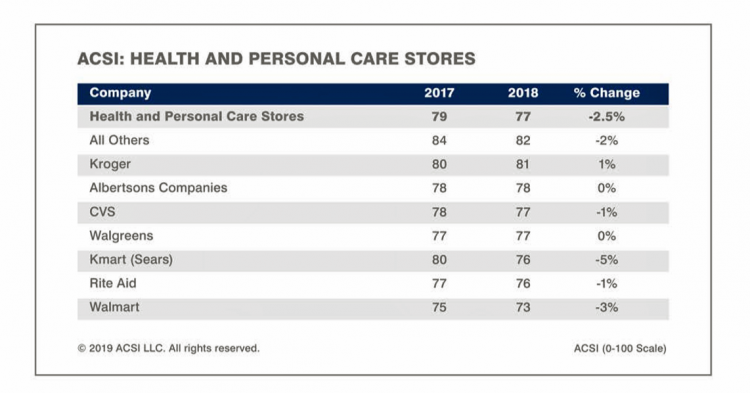
CVS + Aetna have merged to evolve a new business model for health and medical care. Walgreen’s continues to add new services beyond the core pharmacy business, and Walmart is expanding telehealth and healthier food aisles in the grocery. More grocery stores added dietitians to their operations in 2018, as well. As people take on more self-care for health care, they are looking to access products and services in retail bricks-and-mortar and ecommerce channels in the same places they buy food and other products. ACSI’s latest customer satisfaction benchmark study into retailers provides insights into the trusted channels for retail health
National Health Spending Will Reach Nearly 20% of U.S. GDP By 2027
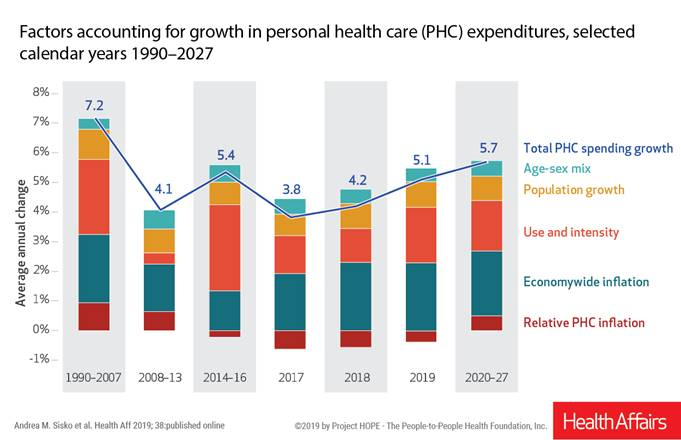
National health spending in the U.S. is expected to grow by 5.7% every year from 2020 to 2027, the actuaries at the Centers for Medicare and Medicaid Services forecast in their report, National Health Expenditure Projections, 2018-2927: Economic And Demographic Trends Drive Spending And Enrollment Growth, published yesterday by Health Affairs. For context, note that general price inflation in the U.S. was 1.6% for the 12 months ending January 2019 according to the U.S. Bureau of Labor Statistics. This growth rate for health care costs exceeds every period measured since the high of 7.2% recorded in 1990-2007. The bar chart illustrates the
“Telehealth is a digital distribution channel for health care” – catching up with Roy Schoenberg, President and CEO of American Well

Ten years ago, two brothers, physicians both, started up a telemedicine company called American Well. They launched their service first in Hawaii, where long distances and remote island living challenged the supply and demand sides of health care providers and patients alike. A decade later, I sat down for a “what’s new?” chat with Roy Schoenberg, American Well President and CEO. In full transparency, I enjoy and appreciate the opportunity to meet with Roy (or very occasionally Ido, the co-founding brother-other-half) every year at HIMSS and sometimes at CES. In our face-to-face brainstorm this week, we covered a wide range
Telehealth and Virtual Care Are Melting Into “Just” Health Care at HIMSS19

Just as we experienced “e-business” departments blurring into ecommerce and everyday business processes, so is “telehealth” morphing into, simply, health care delivery as one of many channels and platforms. Telehealth and virtual care are key education topics and exhibitor presences at HIMSS19. Several factors underpin the adoption of telehealth in 2019: Consumers’ demand for accessible, lower-cost health care services as people face greater financial responsibility for paying the medical bill (via high-deductible health plans and greater out-of-pocket costs for co-payments) Some consumers’ lacking or losing health insurance as ACA coverage eroded in the past two years, resulting in these patients
Health Is Social – The Social Determinants of Health at HIMSS19
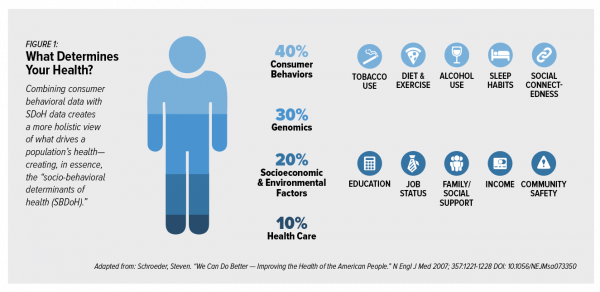
In the health care world, it is now commonly accepted that genes contribute less than half of the influence on peoples’ health status. Other issues play starring roles in overall well-being, including environmental factors, health care services, and social determinants of health (SDOH). These inputs include education, personal economics (like job security and financial stability), physical built environments (think: transportation access, safe and healthy housing), food and nutrition, and access to health care. At HIMSS17, I gave a talk in a big room about how technology can scale SDOH; we had standing room only, which is not a brag —
In U.S. Health Care, It’s Still the Prices, Stupid – But Transparency and Consumer Behavior Aren’t Working As Planned
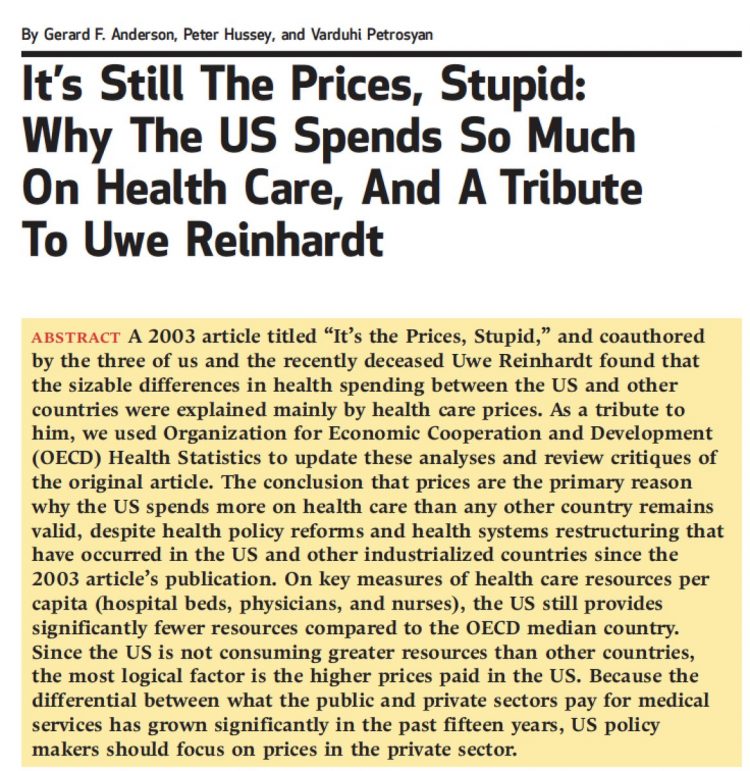
I’m glad to be getting back to health economic issues after spending the last couple of weeks firmly focused on consumers, digital health technologies and CES 2019. There’s a lot for me to address concerning health care costs based on news and research published over the past couple of weeks. We’ll start with the centerpiece that will provide the overall context for this post: that’s the ongoing research of Gerard Anderson and colleagues under the title, It’s Still The Prices, Stupid: Why The US Spends So Much On Health Care, And A Tribute To Uwe Reinhardt. It is bittersweet to
Broadband As Social Determinant of Health – Microsoft’s Plan to Bolster Rural Access

In the U.S., the highest levels of unemployment are in places that often have the lowest access to broadband connectivity. And, “without a proper broadband connection, these communities can’t start or run a modern business, access telemedicine, take an online class, digitally transform their farm, or research a school project online,” Microsoft President Brad Smith said yesterday as the company announced their continued commitment to expanding broadband in rural America. Microsoft is expanding a program the company launched last year to address the rural broadband gap in the U.S. The Airband Initiative is working from Northwest Georgia to South Africa to bolster
Healthcare and the F-Word: Health Politics Rank High on November 6, 2018

“Let’s get this thing f-ing done,” Martha McSally passionately asserted on May 4, 2017. Paul Ryan said, on the floor of the U.S. House of Representatives without cursing, “A lot of us have waited seven years to cast this vote.” McSally, who represents Tucson, Arizona, in the U.S. Congress, is running to replace retiring Senator Jeff Flake. McSally was one of the 217 Republicans in the House who voted to repeal the Affordable Care Act, subsequently celebrating a victory in the Rose Garden of the White House with jubilant peers. The final vote was 217-213. Here’s the final roll call
Loneliness, Public Policy and AI – Lessons From the UK For the US

There’s a shortage of medical providers in the United Kingdom, a nation where healthcare is guaranteed to all Britons via the most beloved institution in the nation: The National Health Service. The NHS celebrated its 70th anniversary in July this year. The NHS “supply shortage” is a result of financial cuts to both social care and public health. These have negatively impacted older people and care for people at home in Great Britain. This article in the BMJ published earlier this year called for increasing these investments to ensure further erosion of population and public health outcomes, and to prevent
The Single Market for Healthcare in Europe: Learnings for the U.S.

When I asked my longtime colleague and friend Robert Mittman, with whom I collaborated at Institute for the Future for a decade, how he managed international travel and jet lag, he said simply, “The time zone you’re in is the time zone you’re in.” This lesson has stayed with me since I received Robert’s advice over twenty years ago. Over the next two weeks, as I work alongside colleagues and clients in the EU and soon-to-Brexit UK, I am in time zones five and six hours later than my home-base of US Eastern Time. But the time zones I’m working
CVS + Aetna: Inflection Point in US Healthcare, Merger Approved Update

CVS Health’s acquisition of Aetna was approved this week by U.S. Federal regulators after months of scrutinizing the antitrust-size-market control implications of the deal. I wrote this post on the deal as an inflection point in American healthcare on 3rd December 2017 when CVS and Aetna announced their marriage intentions. This post updates my initial thoughts on the deal, given the morphing US healthcare market on both the traditional health services front and fast-evolving retail health environment. The nation’s largest retail pharmacy chain signed a deal to combine with one of the top three health insurance companies. The deal
The Importance of Broadband and Net Neutrality for Health, to the Last Person and the Last Mile

California’s Governor Jerry Brown signed into law a net neutrality bill this weekend. Gov. Brown’s proverbial swipe of the pen accomplished two things: he went back to the Obama-era approach to ensure that internet service providers treat all users of the internet equally; and, he prompted the Department of Justice, representing the Trump Administration’s Federal Communications Commission (FCC), to launch a lawsuit. California, home to start-ups, mature tech platform companies (like Apple, Facebook and Google), and countless digital health developers, is in a particularly strategic place to fight the FCC and, now, the Department of Justice. Nearly two dozen other states
Slow Food, Slow Medicine: What Italy Can Teach America About Health
Obesity, diabesity, food deserts and food swamps co-exist across America, factors that cost the U.S. economy over $327 billion a year just in the costs of diagnosed diabetes. In addition, America’s overweight and obesity epidemic results in lost worker productivity, mental health and sleep challenges, and lower quality of life for millions of Americans. Food — healthy, accessible, fairly-priced — is a key social determinant of individual health, wellness, and a public’s ability to pursue happiness. There’s a lot the U.S. can learn from the food culture, policy and economy of Italy when it comes to health. This week, I have the
Retail Tomorrow, Today: A Smart Grocery Cart and Digital Samples For Paleo-Eating Moms

In our Amazon-Primed world, the future of retail is not ten years from now; it’s “tomorrow.” So GMDC, the association of retailers and brands who supply them, has formed a program called Retail Tomorrow to turbocharge the supply side with consumers who are already demanding convenience, immediate (or “soon”) gratification, and health where she/he “is.” That’s personalization, and that’s where retail health can and is making a difference in Everyday Peoples’ lives. In our DIY culture, we’re pumping our own petrol, making our own airline and hospitality reservations (from Expedia to Airbnb), trading stocks online, and cooking at home enabled by
Self-Care is Healthcare for Everyday People

Patients are the new healthcare payors, and as such, taking on the role of health consumers. In fact, health and wellness consumers have existed since a person purchased the first toothpaste, aspirin, heating pad, and moisturizing cream at retail. Or consulted with their neighborhood herbalista, homeopathic practitioner, therapeutic masseuse, or skin aesthetician. Today, the health and wellness consumer can DIY all of these things at home through a huge array of products available in pharmacies, supermarkets, Big Box stores, cosmetic superstores, convenience and dollar stores, and other retail channels – increasingly, online (THINK, of course, of Amazon — more on
The Digital Health Consumer According to Rock Health
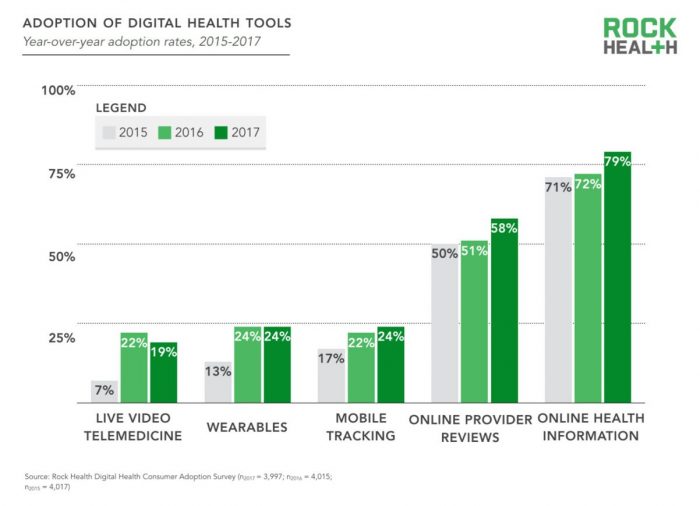
Looking for health information online is just part of being a normal, mainstream health consumer, according to the third Rock Health Digital Health Consumer Adoption Survey published this week. By 2017, 8 in 10 U.S. adults were online health information hunters. Six in 10 Americans looked for reviews of healthcare providers online, another new-normal consumer digital health activity. But only one in four people had used wearable technology for health, and one in five had participated in a live video telemedicine encounter. The Rock Health team observes that “the needle has not moved equally across every type of digital health solution.” Thus the
Disruption Is Healthcare’s New Normal
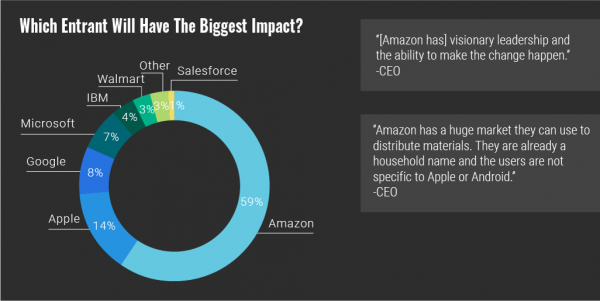
Googling the words “disruption” and “healthcare” today yielded 33.8 million responses, starting with “Riding the Disruption Wave in Healthcare” from Bain in Forbes, Accenture’s essay on “Big Bang Disruption in Healthcare,” and, “A Cry for Encouraging Disruption” in the New England Journal of Medicine Catalyst. This last article responded to the question, “Can we successfully deliver better quality care for patients at a lower cost?” asked by François de Brantes, Executive Director of the Health Care Incentives Improvement Institute. “Disruption” as a noun and an elephant in our room has been with us in healthcare since the September/October 2000 issue of
Value Comes to Healthcare: But Whose Value Is It?
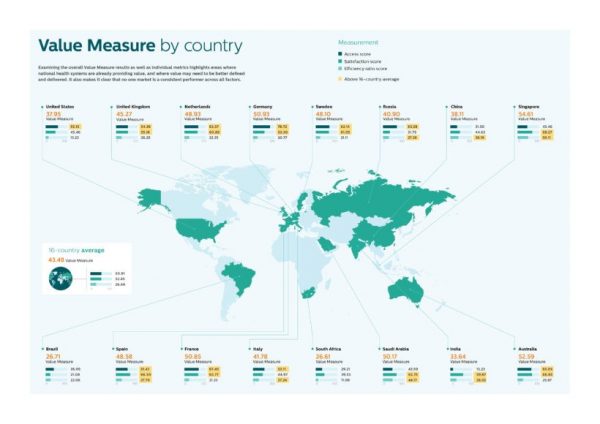
The Search for Value is the prevailing journey to a Holy Grail in healthcare these days. On that, most stakeholders working on the ground, globally. can agree. But whose value is it, anyway? Three reports published in the past few weeks give us some useful perspective on that question, woven together in today’s Health Populi blog. Let’s start with the Philips Future Health Index, which assesses value to 16 national health systems through three lenses: access, satisfaction, and efficiency. The results are shown in the map. “Value-based healthcare is contextual, geared towards providing the right care in the right place, at
Obese, Access-Challenged and Self-Rationing: America’s Health Vs Rest-of-World

The U.S. gets relatively low ROI for its relatively exorbitant spending on healthcare, noted once again in the latest Health at a Glance, the annual OECD report on member nations’ healthcare systems. The report includes U.S. country data asking, “How does the United States compare?” with its sister OECD countries. The answer is, “not well across most population health, access, and mortality measures.” For the Cliff’s Notes/Where’s Waldo top-line of the research, find the two long bars in this chart heading “south” of the OECD average, and one long blue bar going “north.” The northern climbing bar
Hospitals Work to Address Customer Experience Gap With Consumers, Kaufman Hall Finds

Hospital and healthcare providers are getting real about improving patient and health consumer experience, the latest Kaufman Hall research finds. The company’s 2018 State of Consumerism in Healthcare report is out, subtitled, “Activity in Search of Strategy.” Kaufman Hall has developed a Healthcare Consumerism Index for healthcare providers based on four pillars: access to care, consumer experience, pricing, and a strong foundation of consumer insights. Based on their assessment of providers on these components, Kaufman Hall found identified four tiers of performance: The top-performing group, Tier 1, includes only 8% of providers. These are the early adopters who allocate resources
Thinking About Kate and Anthony – Suicide and Depression Is US

Yesterday at 1 pm, we learned that the incidence of suicide is up in America in a report from the Centers for Disease Control (CDC), an agency in the U.S. Department of Health and Human Services. This morning, we awake to news that Anthony Bourdain, the witty and prolific travel and food expert, took his own life. Earlier this week, Kate Spade, fashion designer and creative force, took her own life. The loss of these two bright lights, gone from our lives to suicide within a few days of each other, gives me the sad compulsion to say something, again, about
Personalized Medicine: Consumer Concerns About Coverage, Affordability and Privacy
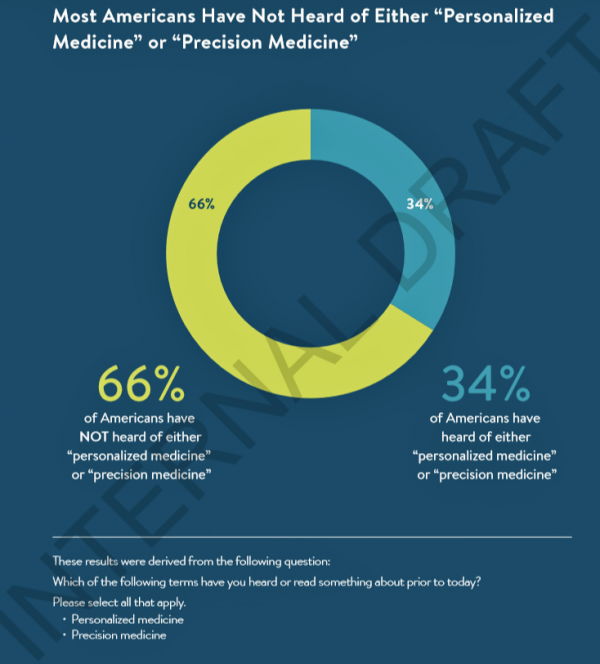
Two in 3 Americans haven’t heard the phrases “personalized medicine” or “precision medicine.” When the concept of therapies tailored to individual patients is explained, most people like the idea of diagnostic tools that can identify biological markers and marry to personal medical records data to help determine medical treatments that best fit them. This picture of U.S. consumers’ views on personalized medicine comes from a survey conducted for PMC, the Personalized Medicine Coalition, and GenomeWeb, published in May 2018. The poll results are published in Public Perspectives on Personalized Medicine, with the top-line finding that life science industry innovators must
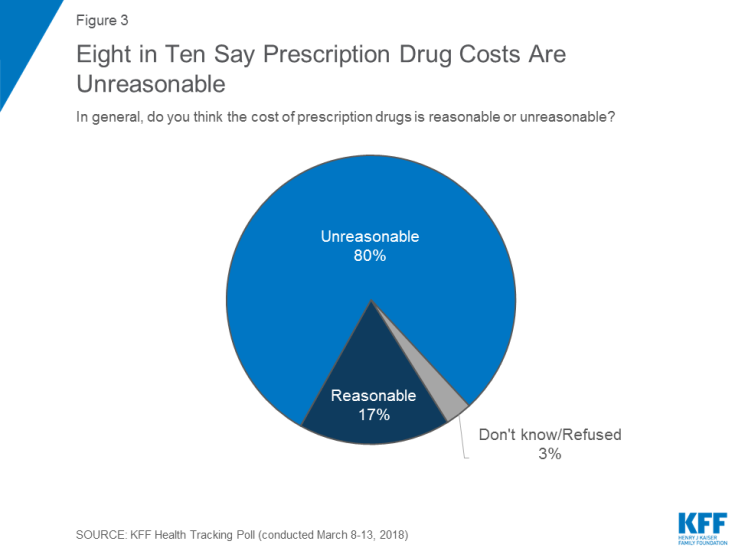
The Gap Between the Trump Administration’s Promise of Reducing Rx Costs for Consumers and What People Really Want
This is what happened to pharma stock prices on Friday after President Trump and Secretary of Health and Human Services Alex Azar outlined their new policies focusing on prescription drug prices. The graph is the Nasdaq U.S. Smart Pharmaceuticals Index (NQSSPH) from May 11, 2018, the date when POTUS and Secretary Azar made their announcement. What this upward driving curve indicates, from the start of stock trading in the morning until the ring of the closing bell, is that the pharma industry players, both manufacturers and PBMs, were quite delighted with what they heard. The blueprint for restructuring the prescription drug industry,
Guns, Jobs, or Health Care? In 2018, Voters Split as to Top Issue
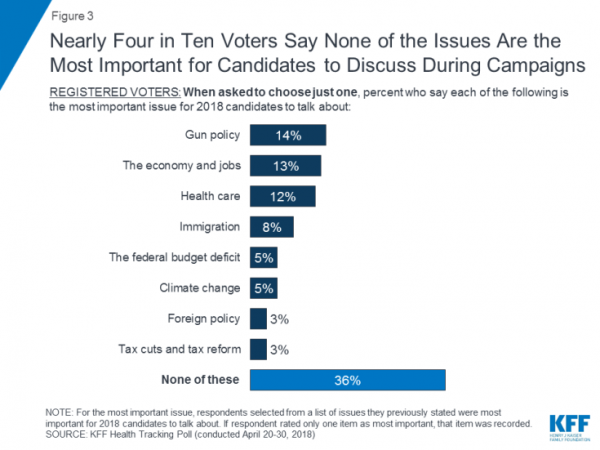
It’s a fairly even split between voting first on gun policy, jobs, or healthcare for the 2018 mid-term elections, ac cording to the May 2018 Kaiser Family Foundation Health Tracking Poll. Arguably, gun policy can cut in two ways: in light of the Stoneman Douglas High School shootings and wake-up call for #NeverAgain among both students and the public-at-large, vis-a-vis Second Amendment issue voters. And, as a growing public health issue, “guns” could also be adjacent to health. “If it isn’t a health problem, then why are all these people dying from it?” rhetorically asked Dr. Garen Wintemute, professor of emergency
Universal Health Care and Financial Inclusion – Two Sides of the Wellness Coin

Two weeks in a row, The Economist, the news magazine headquartered in London, included two special reports stapled into the middle of the magazines. Universal health care was covered in a section on 28 April 2018, and coverage on financial inclusion was bundled into the 5th May edition. While The Economist’s editors may not have intended for these two reports to reinforce each other, my lens on health and healthcare immediately, and appreciatively, connected the dots between healthcare coverage and financial wellness. The Economist, not known for left-leaning political tendencies whatsoever, lays its bias down on the cover of the section here: universal healthcare
Pharma Spending Gone Bipolar: Generics At One End, Specialty Drugs on the Other
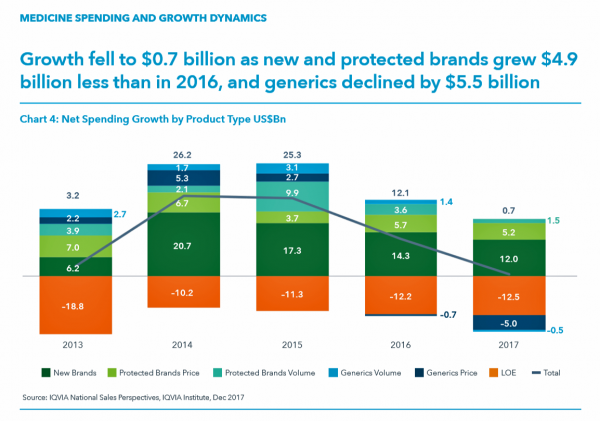
While the use of medicines continues to rise in the U.S., spending grew by only 0.6% in 2017 after accounting for discounts and rebates. In retail and mail-order channels, net spending fell by 2.1%. Prescription drug spending on branded products grew nearly $5 billion less than in 2016; generic drug spending fell by $5.5 billion, according to Medicine Use and Spending in the U.S., a report from the IQVIA Institute for Health Data Science. The report reviews medicines spending in 2017 looking forward to 2022. There were over 5.8 billion prescriptions dispensed in 2017, and generic drugs accounted 90% of
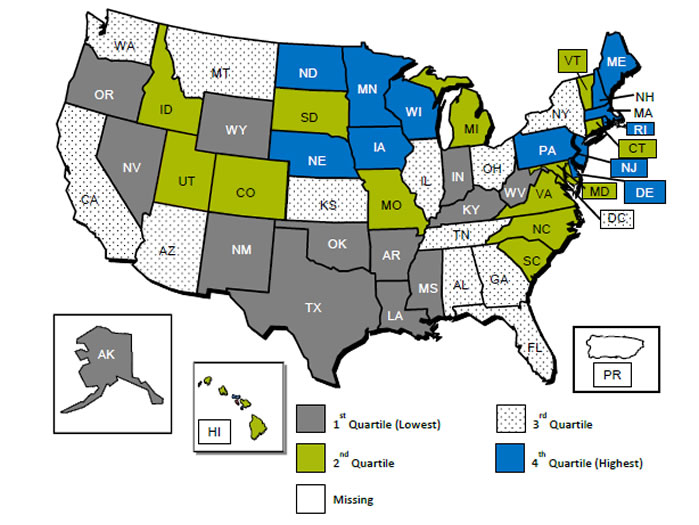
The Health of A Nation – Being Healthy In America Depends on Where You Live

In the US, when it comes to life and death, it’s good to live in Hawaii, Utah, Minnesota, North Dakota, and Iowa — the top five states with the greatest life expectancy and healthy life expectancy at birth in 2016. For health and longevity, sorry to see the lowest five ranked states are Washington DC which ranks last, along with Mississippi, Louisiana, South Carolina, and Alabama. This sober geography-is-health-destiny update was published this week in JAMA, The State of US Health, 1990-2016: Burden of Diseases, Injuries, and Risk Factors Among US States. The first chart illustrates states down the left
Sounds Like A John Denver Song: Virginia and Colorado Towns Rank High As Healthy Communities

If it’s true that “your ZIP code is more important than your genetic code,” you’d look for a job in 22046, buy a house there, and plant your roots. You’d find yourself in Falls Church, Virginia, named number one in the Healthiest Communities rankings of 500 U.S. towns. You can see a list of all of the communities here. The project is a collaboration between the Aetna Foundation and U.S. News & World Report, with help from the University of Missouri Center for Applied Research and Engagement Systems (CARES) and a team from the National Committee on Vital and Health
Building Trust and Truth in Patient Social Networks
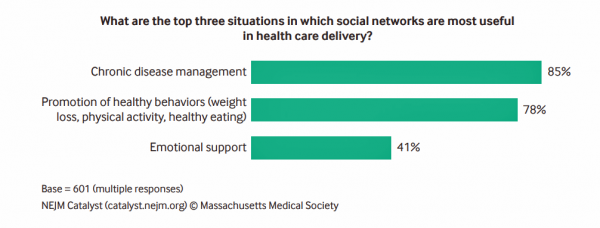
We are only just past the dawn of the second machine age, where digitization is enabling artificial intelligence. “Our new tools are destroying both trust and truth, creating a hunger for community and authenticity. We crave actual physical connection to neighbours, colleagues, and fellow townspeople, even if digitally facilitated.” Anne-Marie Slaughter wrote this in a column I read this morning in the Financial Times titled, “Our struggle with technology to protect trust and truth.” Trust and truth underpin health engagement, we learned in the first Edelman Health Engagement Barometer launched ten years ago. Those were the early days of the formation
How Albertsons Grocery Stores and Rite Aid Can Help Remake Healthcare

Albertsons, the grocery group with popular brands like Acme, Safeway, and Vons, announced a merger with Rite Aid, the retail pharmacy chain. The deal has been discussed as Albertsons’ move to succeed in light of growing competition from Amazon and Whole Foods, the proposed CVS/Aetna merger, and Walgreens’ possible purchase of AmerisourceBergen (finalizing its acquisition of over 1,900 Rite Aid stores). If played out well, the combination could become an important player in the evolving U.S. health/care ecosystem that brings a self-care front-door closer to consumers, patients and caregivers. “The new company is expected to serve more than 40 million
Getting Real About Social Determinants of Health
New research points out that real people live real lives, and our assumptions about social determinants of health (SDOH) may need to be better informed by those real lives. I read three reports in the past week sobering up my bullish #SDOH ethos dealing with food deserts, transportation, and health service access — three key social determinants of health. To remind you about the social determinants, here’s a graphic from Kaiser Family Foundation that summarizes the key pillars of SDOH. Assumption 1: Food deserts in and of themselves diminish peoples’ healthy nutrition lifestyles. Low-income households who are exposed to the same food-buying
Most Americans Say Healthcare is #1 Policy Issue Entering 2018

Concerns about health care are, by a large margin, the top domestic policy issue U.S. voters identified as they enter 2018. The proportion of Americans citing healthcare as the top public agenda priority grew by 50% since 2016, from 31% two years ago to 48%. Taxes rank #2 this year, garnering 31% of Americans’ concerned, followed by immigration, which has remained flat cited by about one-in-four Americans. The Associated Press (AP)-NORC Center for Public Affairs Research polled 1,444 U.S. adults 18 and over between November 30 and December 4, 2017 for this survey. While one-half of Americans would like the
Nurses Rate Highest for Ethics in American Professions Once Again in Gallup Poll
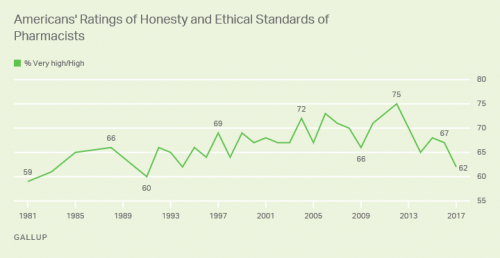
Nurses working in the U.S. are number one when it comes to ethics and honesty, the Gallup Poll found for the sixteenth year in a row. After nurses, military officers, grade school teachers, medical doctors and pharmacists rank second through fifth in ethical-line behind top-rated nursing. It’s important to note that consumers have ranked pharmacists and doctors in second and third place in this annual survey for many years. This year, both professions fall below the military and teachers. Nurses have been #1 in this study every year since Gallup launched the survey in 1999, except for 2001 when firefighters topped
Net Neutrality is Dead: What Happens to Connectivity as a Social Determinant of Health?

Today’s FCC’s repeal of the net neutrality rules for internet service providers will have an impact on healthcare — in particular, the channeling of telehealth services. “The Federal Communication Commission overturned a two-year-old set of rules passed during the Obama administration to protect consumers against bad behavior from their Internet service providers, overriding protests from consumer groups and Internet companies,” USA Today wrote just after the ruling. The concern from advocates to keep net neutrality is that the large ISPs — AT&T, Comcast, and Verizon, among them — could be so-called “bad actors” in favoring fast-lane communications for certain content versus
Movin’ Out(patient) – The Future of the Hospital is Virtual at UPMC

In 2016, most consultations between patients and Kaiser-Permanente Health Plan were virtual — that is, between consumers and clinicians who were not in the same room when the exam or conversation took place. Virtual healthcare may be the new black for healthcare providers. Mercy Health System in St. Louis launched a virtual hospital in 2016, covered here in the Health Populi post, “Love, Mercy, and Virtual Healthcare.” Intermountain Healthcare announced plans to build a virtual hospital in 2018. And, earlier this month, UPMC’s CEO, Jeffrey Romoff, made healthcare headlines saying, “UPMC desires to be the Amazon of healthcare.” UPMC, aka University of Pittsburgh
U.S. Healthcare Spending & Outcomes in Five Charts: #EpicFail in the 2017 OECD Statistics
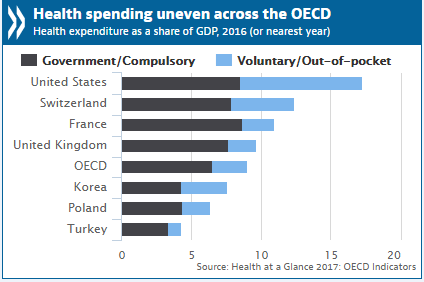
“Spend more. Get less.” If a retailer advertised using these four words, how many consumers would buy that product or service? This is the American reality of healthcare spending in 2016, told in the OECD report, Health at a Glance 2017. I present five charts from the study in this post, which together take the current snapshot health-economic lesson for the U.S. First, look at health expenditures as a share of gross domestic product: the U.S. is number one above Switzerland, France, and the UK, and about two times the OECD average. Note, too, the proportion of out-of-pocket and so-called
Rx Delivery to the Patient’s Door: Home Is Where the Health/Care Is
Talk about the last mile in healthcare. CVS Pharmacy will deliver prescription drugs to patients’ homes, the company announced this week. “Same-day prescription delivery gives customers the easy option of having the pharmacy they trust deliver right to their front door at no cost,” Helen Foulkes, President of CVS Pharmacy, said in the press release. Rx home delivery may not be “the” last mile to conquer all healthcare access challenges, but it’s nonetheless a signal that healthcare industry suppliers are focusing on helping patients streamline their health-consumer lives. In this case, it’s also CVS morphing towards Amazon’s Prime delivery model. Amazon
Most Consumers Would Trust a Health Info Site “Prescribed” by Their Doctor
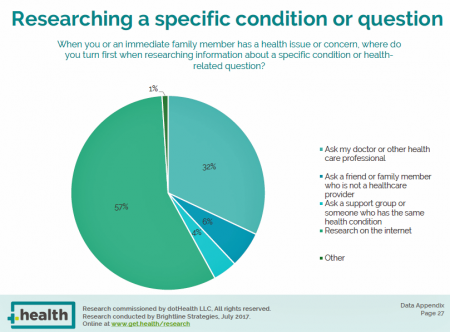
Most consumers access the Internet for health information before they ask their doctor for the same information. But virtually everyone who goes online for health information would trust a website recommended to them by their doctor, according to the dotHealth Consumer Health Online – 2017 Research Report. This survey was conducted on behalf of dotHealth, an internet registry company channeling “.health” domains to organizations in the broad health and healthcare landscape. [FYI, both Health Populi and JaneSarasohnKahn are also registered with .health domains, having availed ourselves of this service at launch]. Six in 10 consumers who have used the internet in the
What Patients Feel About Technology, Healthcare Costs and Social Determinants
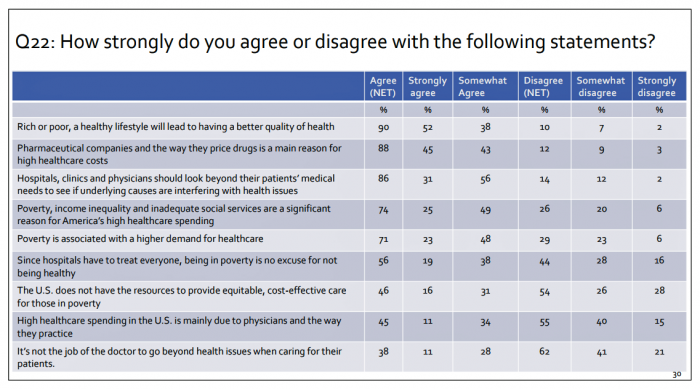
U.S. consumers feel positive about the roles of technology and social determinants in improving healthcare, but are concerned about costs, according to the 2017 Patient Survey Report conducted for The Physicians Foundation. The survey gauged patients’ perspectives across four issues: the physician-patient relationship, the cost of healthcare, social determinants of health, and lifestyle choices. Two key threads in the research explain how Americans feel about healthcare in the U.S. at this moment: the role of technology and the cost of health care. First, the vast majority of consumers view technology, broadly defined, as important for their health care. 85% of people
To Meet Health Consumers’ Digital Demands, Think Netflix and Verizon
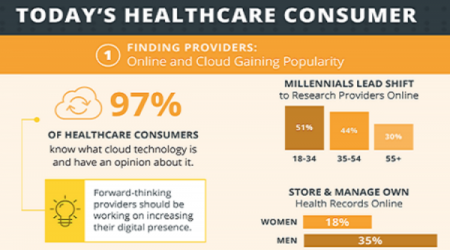
Health consumers have become savvy about the role of technology in their healthcare, according to a survey from Ambra, a company that is in the health cloud business. The survey paints a picture of health consumers hungry for digital health connections. The most popular activities patients do online for health were: To research symptoms and treatments To renew and/or fill prescriptions To view lab reports To make appointments To pay medical bills To correspond with the nurse or doctor To view imaging reports To get virtual care, and, To participate in patient communities. To meet patients where they want
Healthcare Quality and Access Disparities Persist in the U.S.
In 2015, poor and low-income people in America had worse health care than high-income households; care for nearly half of the middle-class was also worse than for wealthier families. Welcome to the 2016 National Healthcare Quality and Disparities Report from the Agency for Healthcare Research and Quality (AHRQ). The report assesses many measures quantifying peoples’ access to health care, such as uninsurance rates (which improved between 2010 and 2016), and quality of health care — including person-centered care, patient safety, healthy living, effective treatment, care coordination, and care affordability. While some disparities lessened between 2000 and 2015, disparities
Most Americans, Including Republicans, Want President Trump’s Administration to Make the ACA Work – Not Fail
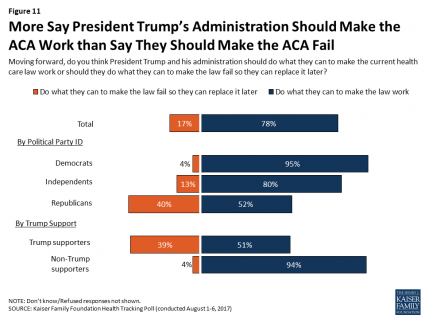
8 in 10 Americans want President Trump and his administration to do what they can to make the Affordable Care Act work, according to the latest August 2017 health tracking poll from Kaiser Family Foundation (KFF). By political party affiliation, this includes 95% of Democrats, 80% of Independents, and 52% of Republicans (that is, to emphasize the point, just over half, a majority, of Republicans). More Americans are also relieved and happy, versus disappointed and angry, that the ACA repeal did not occur (thus far), the second chart illustrates. To be sure, a majority of Republicans register anger and disappointment,
Is There Political Will for Healthcare Access in the US?
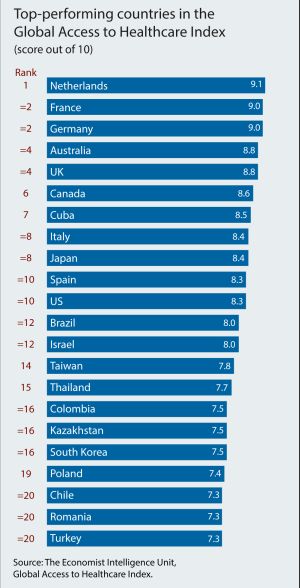
The Netherlands, France and Germany are the best places to be a patient, based on the Global Access to Healthcare Index, developed by the Economist Intelligence Unit (EIU). Throughout the world, nations wrestle with how to provide healthcare to health citizens, in the context of stretched government budgets and demand for innovative and accessible services. The Global Access to Healthcare Index gauges countries’ healthcare systems in light of peoples’ ability to access services, detailed in Global Access to Healthcare: Building Sustainable Health Systems. The United States comes up 10th in line (tied with Spain) in this analysis. Countries that score the
Healthcare Cost Concerns Trump All Others Across the Generations
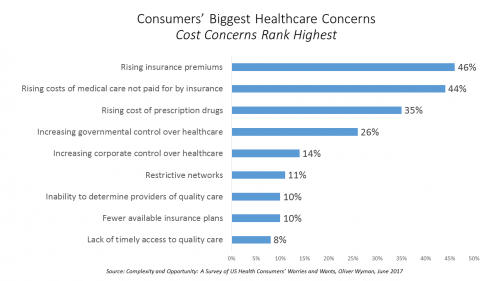
Patients, evolving into health consumers, seek a better healthcare experience. While most people are pretty satisfied with their medical care, cost and confusion reign. This is the topline finding of a study from Oliver Wyman appropriately titled, Complexity and Opportunity, a survey of U.S. health consumers’ worries and wants. Oliver Wyman collaborated on the research with the FORTUNE Knowledge Group. Consumers’ biggest healthcare concerns deal with costs: rising insurance premiums; greater out-of-pocket costs for care not covered by insurance; and, the growing costs of prescription drugs together rank as the top 3 healthcare concerns in this study. After costs, consumers cite government
Healthier Eating Is the Peoples’ Health Reform: the Gallup-Sharecare Well-Being Index

The top healthiest eating communities tend to circle the perimeter of the map of the lower 48 U.S. states. In these towns, more than 72% of health citizens report healthy eating. These areas are located in California, Florida, and Massachusetts, among others. Areas with the lowest rates of healthy eating are concentrated generally south of the Mason-Dixon Line, in places like Arkansas, Kentucky, and Mississippi, and other states. In these places, fewer than 57% of people eat healthy. Eating healthy foods in moderation is a mighty contributor to personal and public health, discussed in the report, State of American Well-Being
Most Physicians Say Patients, Doctors and Hospitals Are All Losers Under Trump
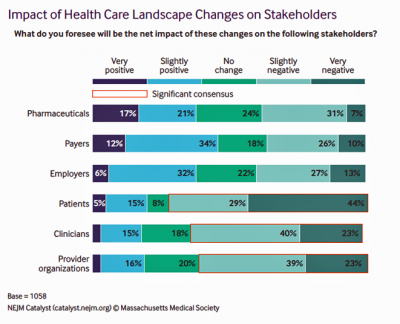
“Overall, Council members express pessimism about the health are landscape in the wake of the Trump administration’s proposed plans, citing no clear winners, only losers: patients, clinicians, and provider organizations.” This is the summary of the Leadership Survey report, Anticipating the Trump Administration’s Impact on Health Care, developed by the New England Journal of Medicine‘s NEJM Group. The first chart illustrates the “biggest healthcare losers” finding, detailed on the bottom three bars of patients, clinicians, and provider organizations. The stakeholders that will fare best under a President Trump healthcare agenda would be drug companies, payers, and employers. The biggest loser
Diet, Surgery and Pharmacy – The Pillars of Healthcare for 500 Years
Healthcare was based on three pillars in 16th century Florence, Italy: diet, surgery, and pharmacy. Five centuries later, not much has changed in Italy or the U.S. But how healthcare gets funded and delivered in the context of these pillars significantly varies between the two countries, and impacts each nation’s health. To put this in context, visiting the Biblioteca Medicea Laurenziana (the Medici’s Laurentian Library) today in Florence was a trip through medical-surgical history, starting in the second half of the 16th century. The design of this magnificent library’s foyer and reading room was initially conceived by Michelangelo. The reading room
States That Expanded Medicaid Improved Healthcare Access & Patient Outcomes
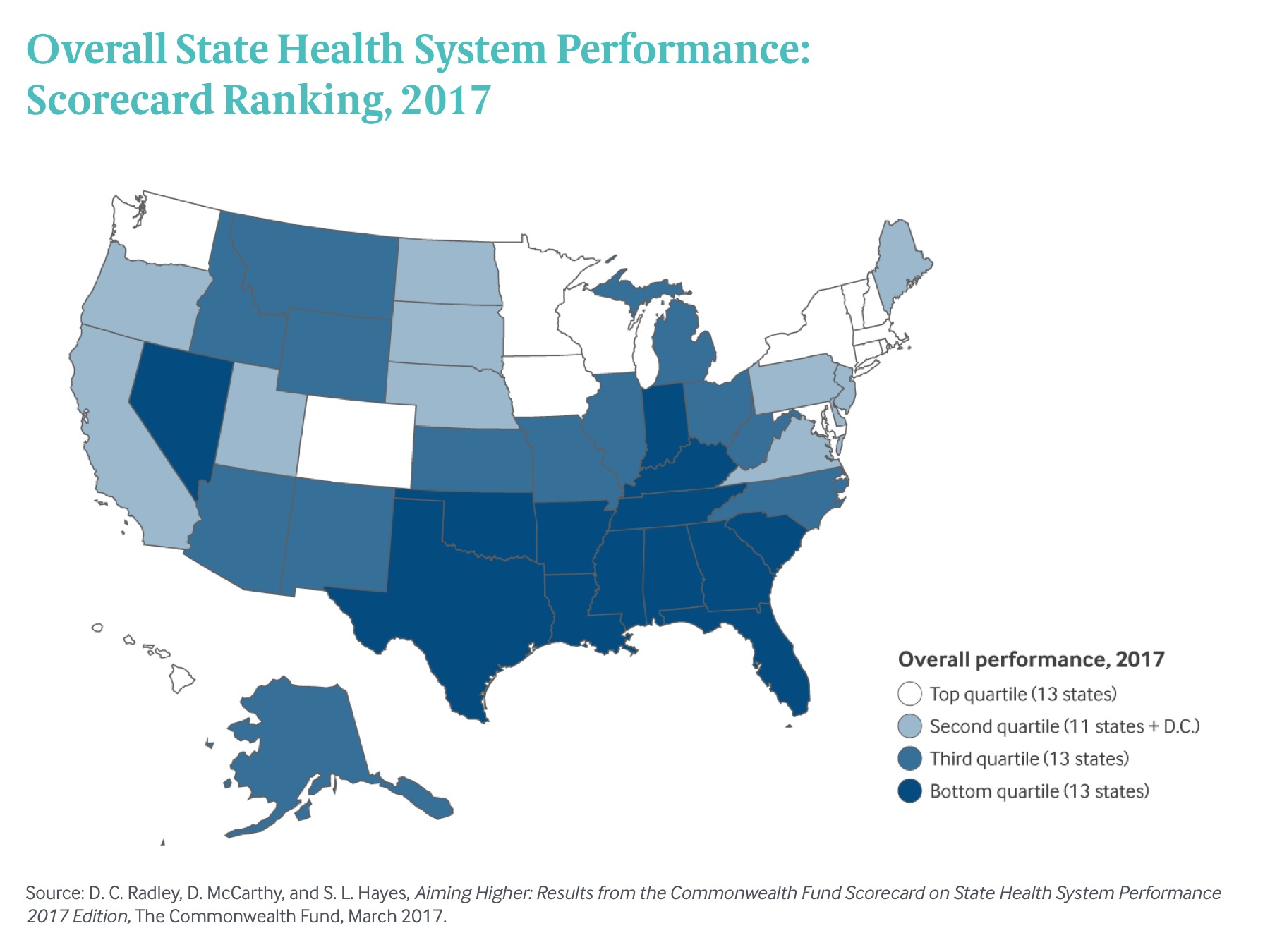
States that expanded Medicaid since the start of the Affordable Care Act made greater health system access improvements than those States that did not expand Medicaid, according to Aiming Higher: Results from the Commonwealth Fund Scorecard on State Health System Performance. There’s good news and bad news in this report: on the upside, nearly all states saw health improvements between 2013 and 2015, and in particular, for treatment quality and patient safety. Patient re-admissions to hospitals also fell in many states. But on the downside, premature deaths increased in nearly two-thirds of states, a reversal in the (improving) national mortality





 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.