Globally Patients Seek Clear Communications to Build Trust with Healthcare, Especially in the AI Era

Globally, patients are growing consumer muscles leaning into trust that’s building on communications that connect with them, based on insightful research from Smart Communications. This consumer research was fielded by Toluna and Harris Interactive in February and March 2024. In The State of Customer Conversations, the report assesses input from global consumers from the APAC region (Australia, New Zealand, China, Hong Kong, Taiwan, Japan, and Singapore), German-speaking markets (Austria, Germany, Switzerland), the United Kingdom, and the U.S. The research revealed five key findings, shown in the first exhibit: Communications are increasingly important
On This July 4th 2024, Let’s Remember the Doctors Who Have Helped Patients Declare Their Independence – Wisdom from Michael Millenson

“’A reform,’ wrote a 19th-century British parliamentarian, ‘is a correction of abuses. A revolution is a transfer of power. As we celebrate the American Revolution, catalyzed by men who broke ranks with their peers to overthrow a power structure that seemed immutable, let’s also celebrate those physicians who broke with their peers and declared independence for American patients.” So begins an informative, timely essay on participatory medicine and patient engagement researched and beautifully written by Michael Millenson, whom I am blessed to call both dear friend and professional colleague. Michael’s essay on the
“Listen to Me:” Personalization in Health Care Starts With Taking Patients’ Voices Seriously – the 15th Beryl Institute-Ipsos PX Pulse Survey
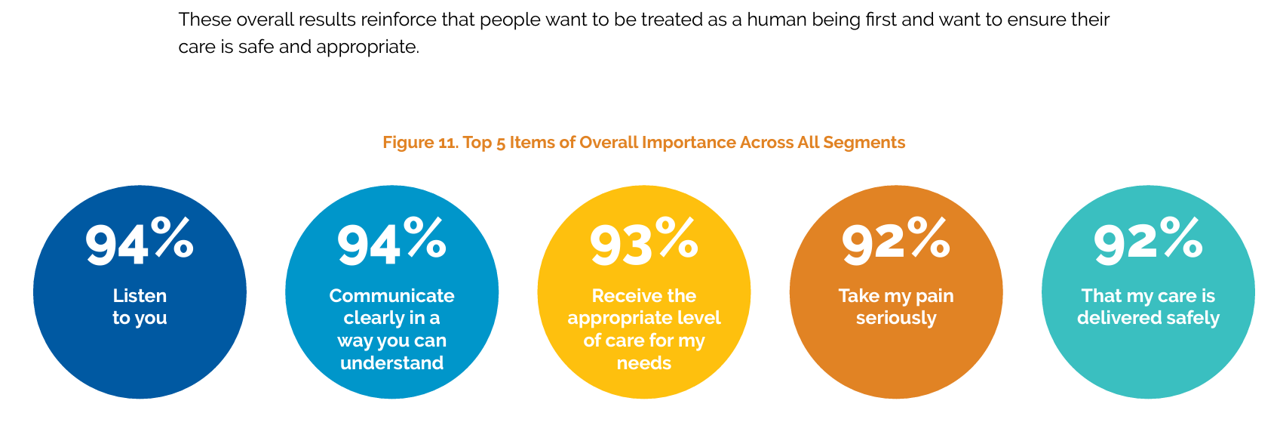
Patients’ experience with health care in the U.S. dropped to its lowest point over the past year, explained in the 15th release of The Beryl Institute – Ipsos PX Pulse survey. The study into U.S. adult consumers’ perspectives defined “patient experience” (PX) as, “The sum of all interactions, shaped by an organization’s culture, that influence patient perceptions across the continuum of care.” The survey was fielded by Ipsos among 1,018 U.S. adults in March 2024. Health care providers (and other industry stakeholders that go B2B or B2B2C (or P) are all thinking
How to Get Better Care to More People? Address Burnout, Bridge Insights with AI, Embed Sustainability – the Philips Future Health Index 2024

Health care access is a challenge in rural and urban areas, cities and suburbs, and across more demographic groups than you might realize, as we see wait times grow for appointments, primary care shortages, and delays in screening plaguing health systems around the world. In the Future Health Index 2024, Philips’ latest annual report presents a profile of the state of health care focused on how to provide better care for more people. For the report, Philips surveyed a total of 2,800 healthcare leaders consisting of 200 respondents in 14 countries: Australia, Brazil, China,
The Thematic Roadmap for AHIP 2024: What the Health Insurance Conference Will Cover

Health insurance plans make mainstream media news every week, whether coverage deals with the cost of a plan, the cost of out-of-network care, prior authorizations, or cybersecurity and ransomware attacks, among other front-page issues. This week, AHIP (the acronym for the industry association of America’s Health Insurance Plans) is convening in Las Vegas for its largest annual 2024 meeting. We expect at least 2,400 attendees registered for the meeting, and they’ll not just be representing the health insurance industry itself; folks will attend #AHIP2024 from other industry segments including pharmaceuticals, technology, hospitals and health systems, and the investment and financial services
Is There an Easy-Button for AI In Healthcare Team Well-Being? Exploring a New PC with Embedded AI

“The greatest opportunity offered by AI is not reducing errors or workloads, or even curing cancer: it is the opportunity to restore the precious and time-honored connection and trust,” Dr. Eric Topol wrote in his 2019 book, Deep Medicine: How Artificial Intelligence Can Make Healthcare Human Again. In the five years since Dr. Topol looked for AI to bolster the human-touch in health care, we’ve lived, worked, and muddled our way through the COVID-19 pandemic and witnessed the growing epidemic of burnout among clinicians, the front-line of medical care. I recalled Dr. Topol’s assertion on AI’s promise for humanizing health
How AI is Shaping the Patient and Clinician Experience – My Conversation with Microsoft
For change agents in health care, one of our True North paradigms is the Quintuple Aim. The five pillars of the Quint Aim grew from 3 goals of the Triple Aim: to improve patient experience, to drive better health outcomes, and to lower per patient costs. The Quadruple Aim added the goal of bolstering clinicians’ well-being (to address burnout, stress and depression), leading to the addition of health equity as the fifth objective. That happened in 2021, in the height of the COVID-19 pandemic which shined a bright light on health disparities, inequities, and risks in peoples’ social determinants of
From Evolution to Innovation, from Health Care to Health: How Health Plans With Collaborators Are Re-Defining the Industry
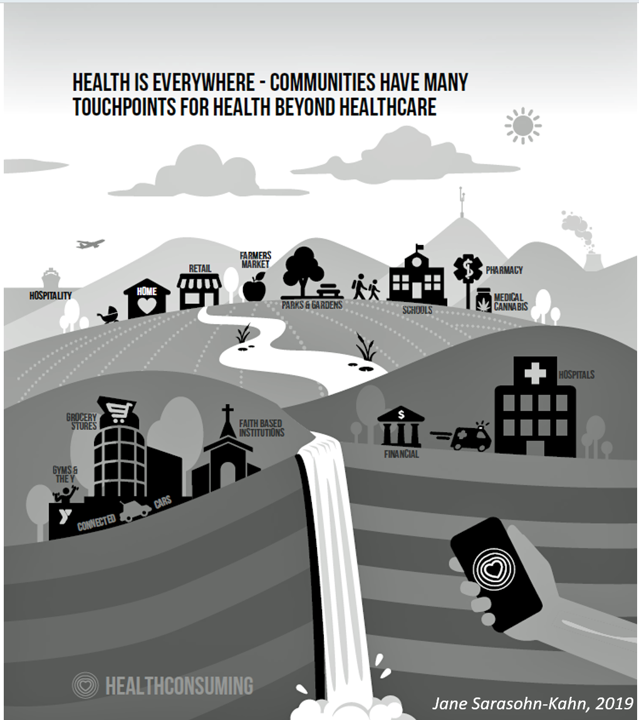
As a constant observer and advisor across the health/care ecosystem, for me the concept of a “health plan” in the U.S. is getting fuzzier by the day. Furthermore, health plan members now see themselves as medical bill payers, seeking value and consumer-level services for their health insurance premium investment. Weaving these ideas together is my mission in preparing a session to deliver at the upcoming AHIP 2024 conference in June, I’m thinking a lot about the evolving nature of health insurance, plans, and the organizations that provide them. To help me define first principles, I turned to the American father
Physicians Feeling Burnout and Depression Continues in 2024 — The Annual View From Medscape
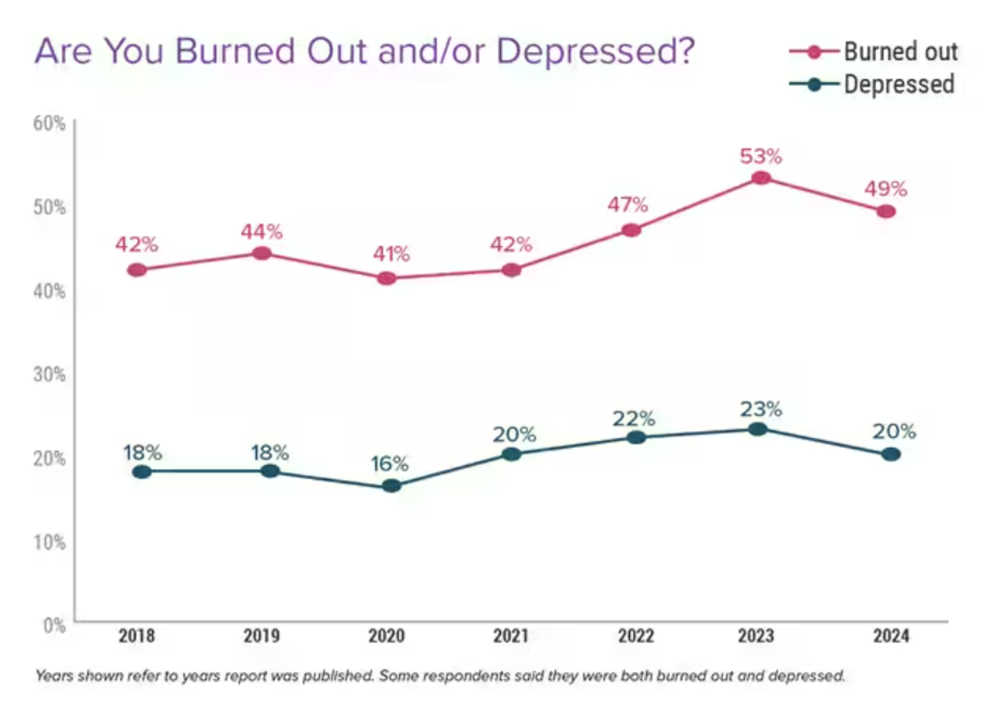
One-half of U.S. physicians report feeling burned out, and 3 in 5 of those doctors say they have felt burned out for over two years, according to the Physician Burnout & Depression Report for 2024 from Medscape. While the study’s press release asserts there may be “progress” given the percent of doctors citing burnout fell by 4 percentage points from 53% of doctors in 2022 to 49% in 2023, it is obvious the U.S. physicians need greater support and less taboo concerning their mental health which impacts both their professional and personal lives.
Ethics for AI in Health – A View From The World Health Organization
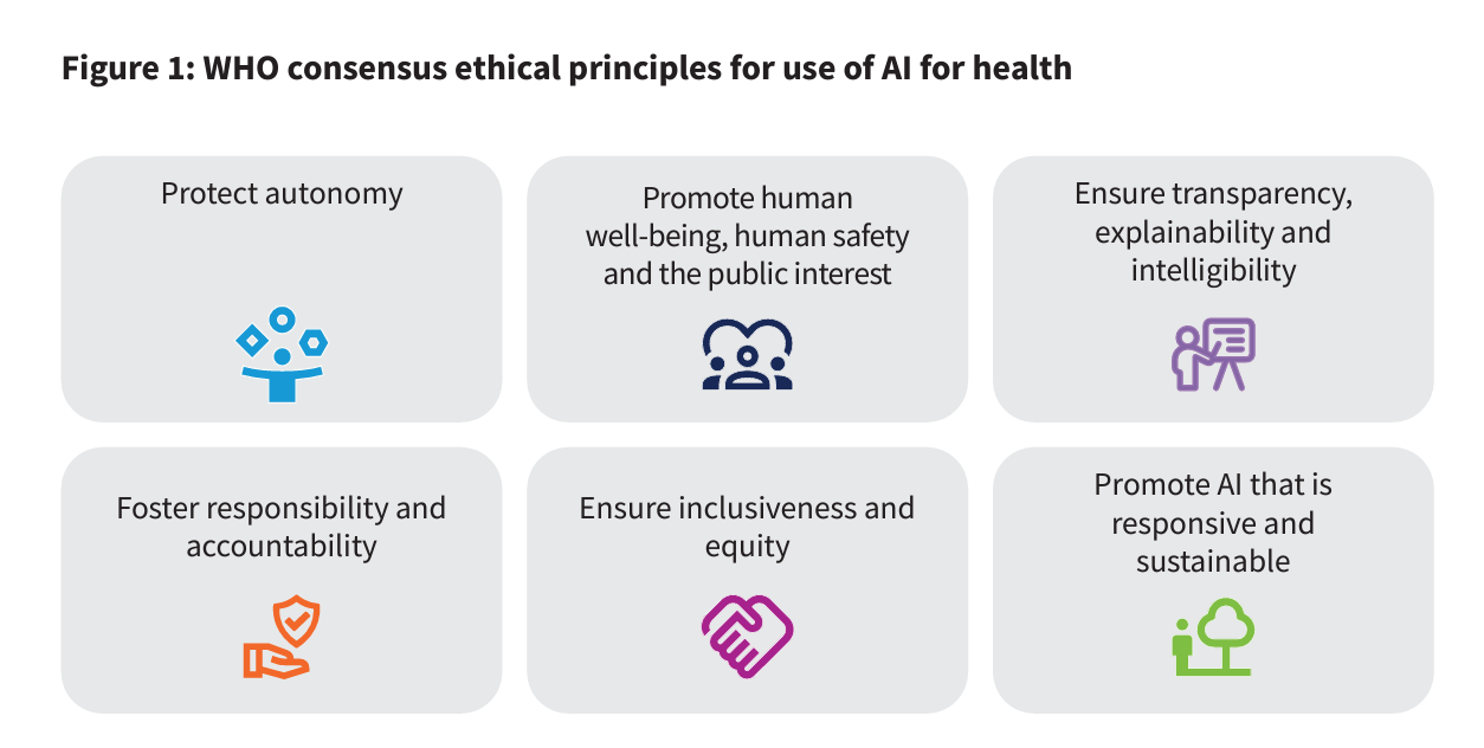
For health care, AI can benefit diagnosis and clinical care, address paperwork and bureaucratic duplication and waste, accelerate scientific research, and personalize health care direct-to-patients and -caregivers. On the downside, risks of AI in health care can involve incomplete or false diagnoses, inaccuracies and errors in cleaning up paperwork, exacerbate differential access to scientific knowledge, and exacerbate health disparities, explained in the World Health Organization’s (WHO) report, Ethics and governance of artificial intelligence for health. WHO has released guidance on the use of large multi-modal models (LMMs) in health care which detail 40+ recommendations for
Nurses Continue to Rank Highest in Ethics and Honesty for Professions in the US — But Peoples’ Opinions for All Jobs, Including Nursing, Have Eroded in Gallup’s Latest Poll
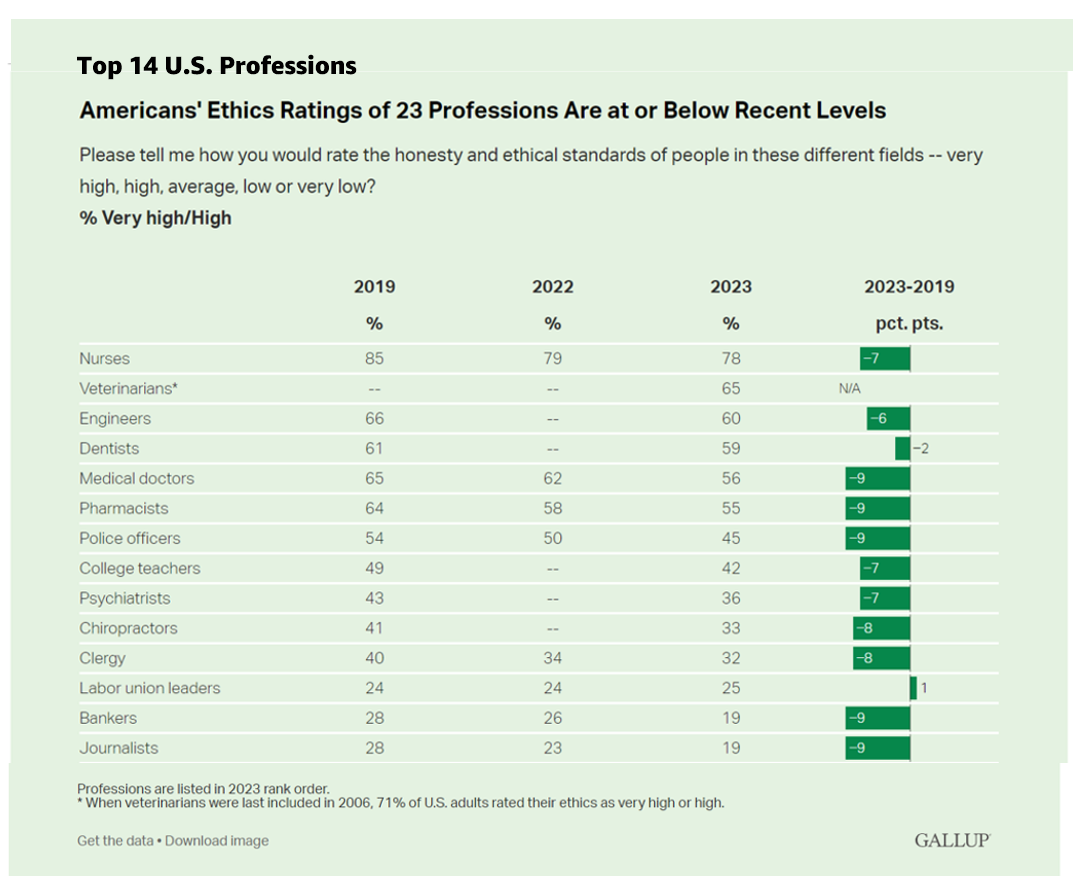
Ratings of honesty and ethics in professions have fallen down in the U.S., we find the Gallup Poll’s annual assessment of rankings for occupations that touch peoples’ lives in America. Each year for over a decade, nurses have ranked highest in this survey, representing the most-trusted profession working in America. However, even nurses’ ethic-equity has dropped in the hearts and minds of Americans over the past four years, falling 7 percentage points from a high of 85% of citizens ranking nurses at the greatest level of honesty and ethics to
Patients, Nurses and Doctors Blame Health Insurers for Increasing Costs and Barriers to Care
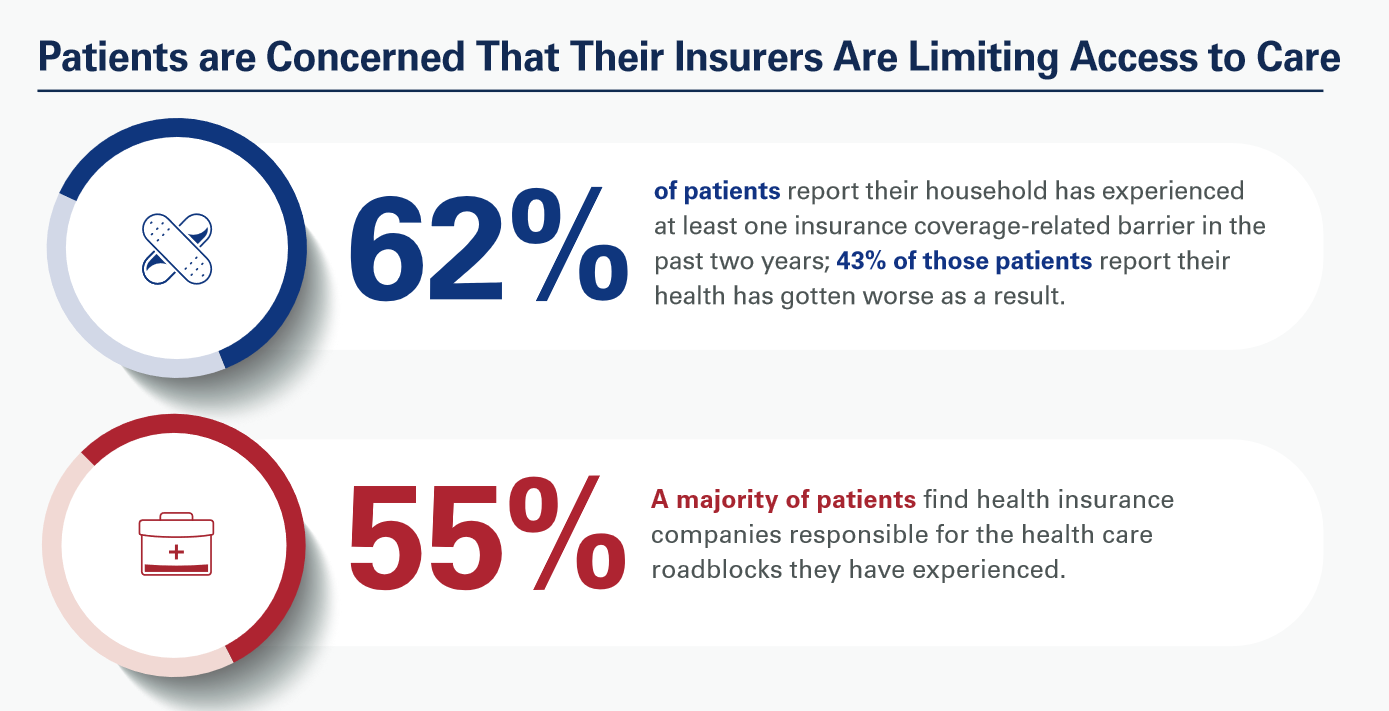
Most patients, nurses and doctors believe that health insurance plans reduce access to health care which contributes to clinician burnout and increases costs, based on three surveys conducted by Morning Consult for the American Hospital Association (AHA). Most patients have experienced at least one health insurance related barrier in the past two years, and 4 in 10 of those people said their health got worse as a result of that care-barrier. “These surveys bear out what we’ve heard for years — certain insurance companies’ policies and practices are reducing health care access and making




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...