Can AI Make Healthcare Human Again? Dr. Topol Says “Yes”
“The Fourth Industrial Age,” Dr. Abraham Verghese writes, “has great potential to help, but also to harm, to exaggerate the profound gap that already exists between those who have much and those who have less each passing year.” Dr. Verghese asserts this in his forward to Deep Medicine, Dr. Eric Topol’s latest work which explores the promise of artificial intelligence (AI), Big Data, and robotics — three legs of the Fourth Industrial Age stool. [If you don’t know the work of Dr. Verghese, and since you’re reading the Health Populi blog, you must get to know Dr. V now. Your
Digital Transformation Is The New Mantra But Can’t Happen Without Access To Connectivity
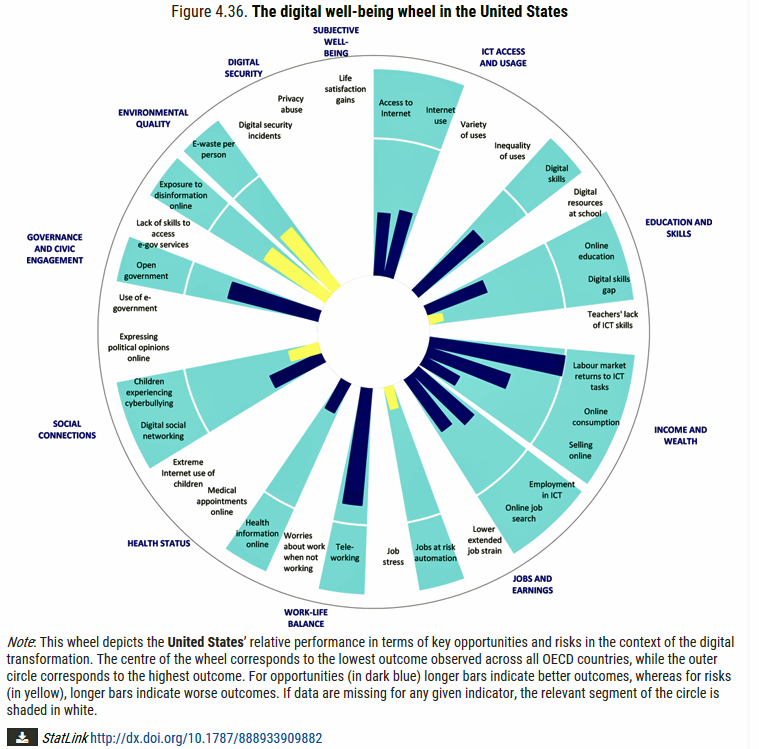
As more of our “things” get digitally connected, there’s an unanswered question about how our connected lives impact human life and health. A new report from the OECD asks and answers: How’s Life in the Digital Age? Opportunities and Risks of the Digital Transformation for People’s Well-being. This research is part of OECD’s ongoing series asking the Big Question, “How’s Life?” A prevailing current mantra in work and daily living is “digital transformation.” The OECD broadly defined the phrase in their 2017 paper on the topic as follows: Mobility, cloud computing, the Internet of things (IoT), artificial intelligence (AI) and big
Calling Out Health Equity on Martin Luther King Day 2019
On this weekend as we appreciate the legacy of Martin Luther King, Jr., I post a photo of him in my hometown of Detroit in 1963, giving a preliminary version of the “I Have a Dream” speech he would deliver two months later in Washington, DC. Wisdom from the speech: “But now more than ever before, America is forced to grapple with this problem, for the shape of the world today does not afford us the luxury of an anemic democracy. The price that this nation must pay for the continued oppression and exploitation of the Negro or any other
What #CES2019 5 Tech Trends to Watch Mean for Health/Care

As #CES2019 kicks off in Las Vegas with today’s first Media Day, the Consumer Technology Association presented its forecast on the 5 Technology Trends to Watch in 2019 — and they all play into health, wellness, and medical care. The five trends are: Artificial Intelligence on the Rise Envisioning the Smart Home of the Future Digital Health Tech Empowers Patients Esports and Sports Technology, and Smart Cities Promote Resilience. Here are how these five mega-trends can bolster our health and healthcare products and services over the next decade. AI is indeed on-the-rise in healthcare: as I have begun planning my agenda for
While National Health Care Spending Growth Slowed in 2017, One Stakeholder’s Financial Burden Grew: The Consumer’s

National health care spending growth slowed in 2017 to the post-recession rate of 3.9%, down from 4.8% in 2016. Per person, spending on health care grew 3.2% to $10,739 in 2017, and the share of GDP spent on medical care held steady at 17.9%. Healthcare spending in America is a $3.5 trillion micro-economy…roughly the size of the entire GDP of Germany, and about $1 trillion greater than the entire economy of France. These annual numbers come out of the annual report from the Centers for Medicare and Medicaid Services, published yesterday in Health Affairs. Underneath these macro-health economic numbers is
Broadband As Social Determinant of Health – Microsoft’s Plan to Bolster Rural Access

In the U.S., the highest levels of unemployment are in places that often have the lowest access to broadband connectivity. And, “without a proper broadband connection, these communities can’t start or run a modern business, access telemedicine, take an online class, digitally transform their farm, or research a school project online,” Microsoft President Brad Smith said yesterday as the company announced their continued commitment to expanding broadband in rural America. Microsoft is expanding a program the company launched last year to address the rural broadband gap in the U.S. The Airband Initiative is working from Northwest Georgia to South Africa to bolster
The Ultimate Health Outcome, Mortality, Is Rising in America

How long can people living in the U.S. expect to live? 78.6 years of age, if you were born in 2017. That’s a decline of 0.1 year from 2016. This decline especially impacted baby boys: their life expectancy fell to 76.1 years, while baby girls’ life expectancy stayed even at 81.1 years. That’s the latest data on Mortality in the United States, 2017, soberly brought to you by the Centers for Disease Control and Prevention, part of the U.S. Department of Health and Human Services. Underneath these stark numbers are the specific causes of death: in 2017, more Americans died
The Importance of Broadband and Net Neutrality for Health, to the Last Person and the Last Mile

California’s Governor Jerry Brown signed into law a net neutrality bill this weekend. Gov. Brown’s proverbial swipe of the pen accomplished two things: he went back to the Obama-era approach to ensure that internet service providers treat all users of the internet equally; and, he prompted the Department of Justice, representing the Trump Administration’s Federal Communications Commission (FCC), to launch a lawsuit. California, home to start-ups, mature tech platform companies (like Apple, Facebook and Google), and countless digital health developers, is in a particularly strategic place to fight the FCC and, now, the Department of Justice. Nearly two dozen other states
The Social Determinants of Food for Health, Farms, and the Economy
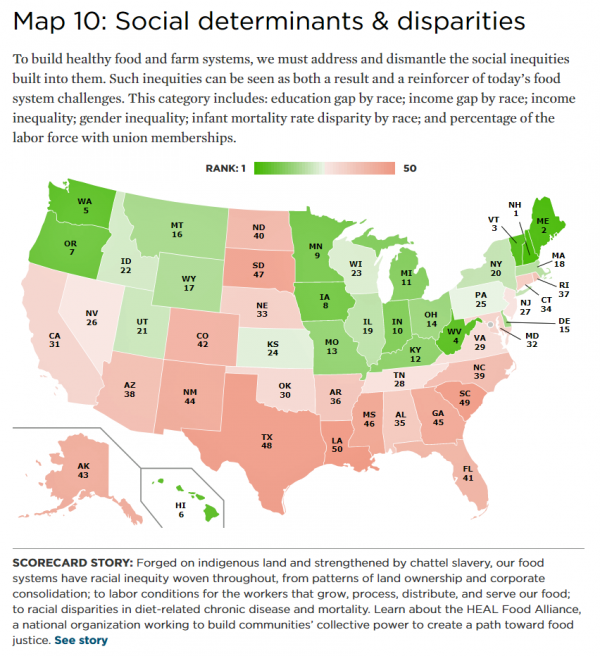
America’s agricultural roots go deep, from the native Patuxet tribe that shared maize with Mayflower settling Pilgrims in southern New England, to biodynamic and organic winemakers in Sonoma County, California, operating today. In 2016, 21.4 million full- and part-time jobs were related to agriculture and food sectors, about 11% of total U.S. employment. Farming is an integral part of a nation’s food system, so the Union of Concerned Scientists developed the 50-State Food System Scorecard to gauge the state of farming and food in the U.S. on several dimensions: diet and health outcomes, farming as an industry and economic engine,
Consumers Consider Cost When They Think About Medical Innovation
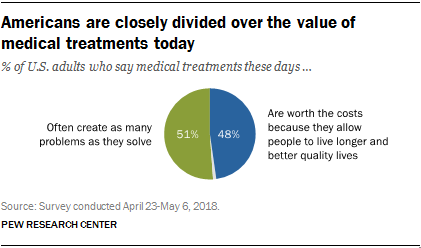
While the vast majority of Americans say that science has made life easier for most people, and especially for health care, people are split in questioning the financial cost and value of medical treatments, the Pew Research Center has found. The first chart illustrates the percent of Americans identifying various aspects of medical treatments as “big problems.” If you add in people who see these as “small problems,” 9 in 10 Americans say that all of these line items are “problems.” In the sample, two-thirds of respondents had seen a health care provider for an illness or medical condition in
Value Comes to Healthcare: But Whose Value Is It?
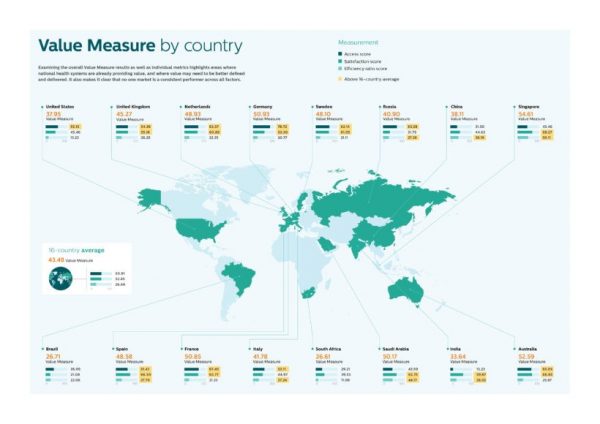
The Search for Value is the prevailing journey to a Holy Grail in healthcare these days. On that, most stakeholders working on the ground, globally. can agree. But whose value is it, anyway? Three reports published in the past few weeks give us some useful perspective on that question, woven together in today’s Health Populi blog. Let’s start with the Philips Future Health Index, which assesses value to 16 national health systems through three lenses: access, satisfaction, and efficiency. The results are shown in the map. “Value-based healthcare is contextual, geared towards providing the right care in the right place, at
Diabetes and Independence Day: An Inflection Point for Rising Blood Sugar
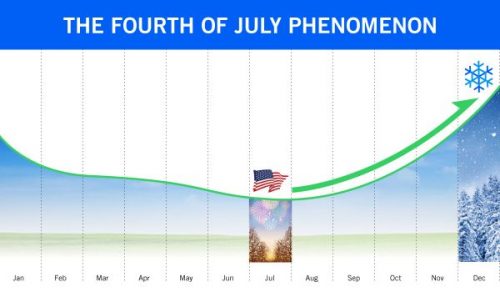
In the USA, July 4th celebrates the adoption of the Declaration of Independence on that day in 1776. For people with diabetes, July 4th is also an inflection point when blood glucose spikes and kicks off a rise in blood sugar levels through autumn to New Year’s Eve. The team at Livongo observed this by mining 20 million blood glucose measures among its community of people with diabetes. This research debuted in the inaugural Insights Report, Diabetes Across America: Seasons, Regions & More. I appreciated the opportunity to discuss these findings with Dr. Jennifer Schneider, Chief Medical Officer at Livongo. I
Obese, Access-Challenged and Self-Rationing: America’s Health Vs Rest-of-World

The U.S. gets relatively low ROI for its relatively exorbitant spending on healthcare, noted once again in the latest Health at a Glance, the annual OECD report on member nations’ healthcare systems. The report includes U.S. country data asking, “How does the United States compare?” with its sister OECD countries. The answer is, “not well across most population health, access, and mortality measures.” For the Cliff’s Notes/Where’s Waldo top-line of the research, find the two long bars in this chart heading “south” of the OECD average, and one long blue bar going “north.” The northern climbing bar
It Could Take Five Generations for a Low-Income US Family to Reach Average Income in America

Social mobility in America has a lot of friction: children of wealthier people tend to grow into affluence, and children of low-income parents tend to struggle to move up the income and education ladder, according to A Broken Social Elevator: How to Promote Social Mobility, a new report from the OECD. The Organization for Economic Cooperation and Development studied member nations’ economies, demographics, income and opportunities to gauge each country’s social mobility. Social mobility, the OECD explains, is multi-faceted. It can refer to inter-generational mobility between parents, children, and grandchildren. Alternatively, social mobility can look at intra-generational mobility, over the course
Pope Francis is a Public Health Advocate

“The world today is mostly deaf,” the Pontiff observes in Pope Francis: A Man of His Word, Wim Wenders’ documentary on this religious leader who likes to quote Dostoevsky, joke about mothers-in-law, and advocate for the sick, the poor, the disenfranchised, and Planet Earth. He is, I realized while watching this film and hearing this man of words, a public health advocate. Throughout the film, we see clips of Pope Francis washing the feet of prisoners in Philadelphia, comforting dying children in a pediatric clinic in central Africa, and speaking out to the U.S. Congress about the dangers of climate
Re-Tweeting Sanofi’s Tweet: Inclusion Matters for Health, Wellness, and the Body Politic
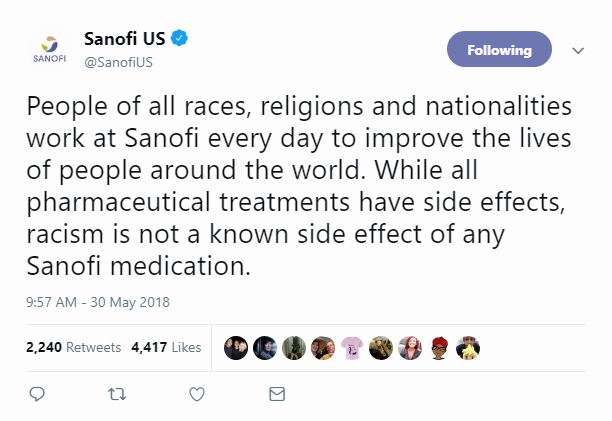
The communications team at Sanofi, the France-based global pharmaceutical company, quickly responded to a tweet by Roseanne Barr issued this morning about how her use of Ambien was related to her offensive tweet lobbed yesterday on Twitter about Valerie Jarrett, President Obama’s senior advisor. Barr’s comment on Twitter late last night was that, “I was ambien tweeting.” Ambien is Sanofi’s prescription drug used by patients to deal with insomnia and sleeplessness. Data provided to the FDA from patients who have used the product demonstrate a variety of side effects including but not limited to nausea, headache, slowed breathing, and amnesia
The Healthiest Communities Are Built on Education, Good Food, Mindfulness, and the Power of Love

Be the change you wish to see in the world, Gandhi has been attributed as saying. This sentiment was echoed by Lauren Singer as we brainstormed the social determinants of health and the factors that underpin healthy communities. Our Facebook Live session was convened by the Aetna Foundation, which sponsored research on the Healthiest Communities in 2018. In addition to Lauren, founder of Trash Is For Tossers, Dr. Garth Graham, President of the Aetna Foundation, Dr. Pedro Noguera, Distinguished Professor of Education at UCLA, and I joined the quartet, moderated with panache and sensitivity by Mark J. Ellwood, journalist. Each
The U.S. is a Nation in Pain – America’s Life Expectancy Fell Again in 2016
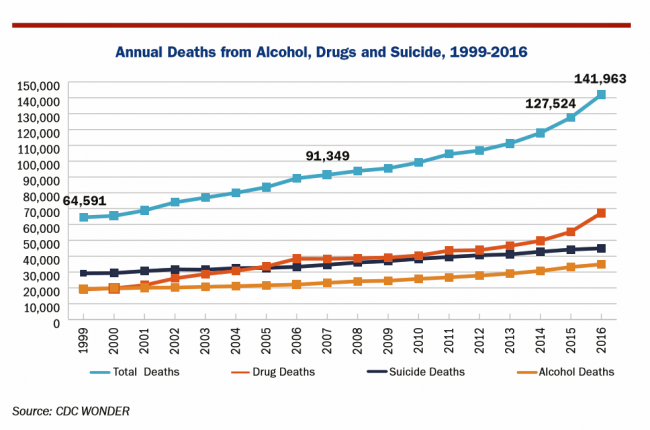
American saw the greatest number of deaths from suicide and alcohol- and drug-induced fatalities was recorded in 2016. That statistic of nearly 142,000 equates to deaths from stroke and exceed the number of deaths among Americans who died in all U.S. wars since 1950, according to Pain in the Nation Update from the Well Being Trust and Trust for America’s Health. The line graph soberly illustrates the growing tragic public health epidemic of mortality due to preventable causes, those deaths of despair as Anne Case and Sir Angus Deaton have observed in their research into this uniquely all-American phenomenon. While this
A Tale of Two America’s for Health
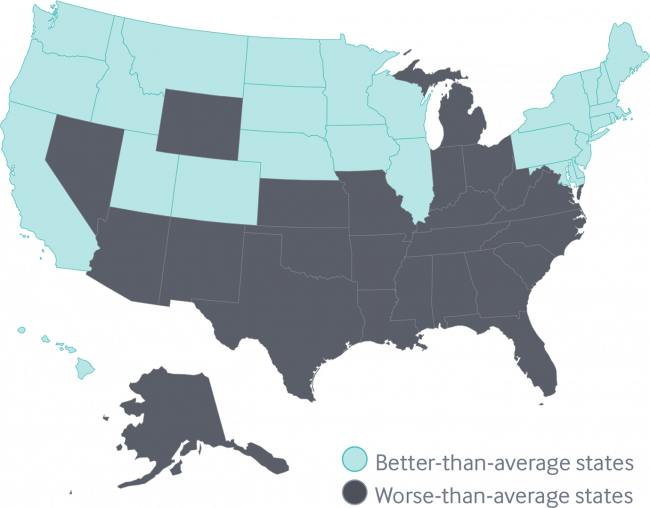
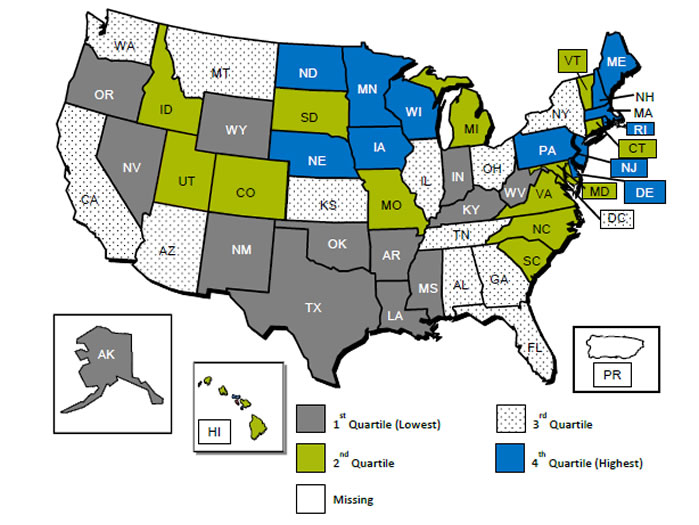
Disparities in Americans’ health vary among people living in each of the 50 states. These differences in health status generally fall into two regions: north and south, found in the Commonwealth Fund’s 2018 Scorecard on State Health System Performance. The map shows this stark geography-is-health-destiny reality: the worse-than-average states, the Fund found, run from Nevada southeast to Arizona, through New Mexico and Texas all the way to Atlantic Ocean and the Carolinas, then north west all the way up through the industrial Midwest states through Michigan to the north. Wyoming is the only non-contiguous state in the worse-performing U.S. state
Universal Health Care and Financial Inclusion – Two Sides of the Wellness Coin

Two weeks in a row, The Economist, the news magazine headquartered in London, included two special reports stapled into the middle of the magazines. Universal health care was covered in a section on 28 April 2018, and coverage on financial inclusion was bundled into the 5th May edition. While The Economist’s editors may not have intended for these two reports to reinforce each other, my lens on health and healthcare immediately, and appreciatively, connected the dots between healthcare coverage and financial wellness. The Economist, not known for left-leaning political tendencies whatsoever, lays its bias down on the cover of the section here: universal healthcare
Food as Medicine Update: Danone Goes B-Corp, Once Upon a Farm Garners Garner, and Livongo Buys Retrofit

As the nation battles an obesity epidemic that adds $$ costs to U.S. national health spending, there are many opportunities to address this impactful social determinant of health to reduce health spending per person and to drive public and individual health. In this post, I examine a few very current events in the food-as-medicine marketspace. Big Food as an industry gets a bad rap, as Big Tobacco and Big Oil have had. In the case of Big Food, the public health critique points to processed foods, those of high sugar content (especially when cleverly marketed to children), and sustainability. But
The Health of A Nation – Being Healthy In America Depends on Where You Live

In the US, when it comes to life and death, it’s good to live in Hawaii, Utah, Minnesota, North Dakota, and Iowa — the top five states with the greatest life expectancy and healthy life expectancy at birth in 2016. For health and longevity, sorry to see the lowest five ranked states are Washington DC which ranks last, along with Mississippi, Louisiana, South Carolina, and Alabama. This sober geography-is-health-destiny update was published this week in JAMA, The State of US Health, 1990-2016: Burden of Diseases, Injuries, and Risk Factors Among US States. The first chart illustrates states down the left
Sounds Like A John Denver Song: Virginia and Colorado Towns Rank High As Healthy Communities

If it’s true that “your ZIP code is more important than your genetic code,” you’d look for a job in 22046, buy a house there, and plant your roots. You’d find yourself in Falls Church, Virginia, named number one in the Healthiest Communities rankings of 500 U.S. towns. You can see a list of all of the communities here. The project is a collaboration between the Aetna Foundation and U.S. News & World Report, with help from the University of Missouri Center for Applied Research and Engagement Systems (CARES) and a team from the National Committee on Vital and Health
How We Spend Versus What We Get: America’s Healthcare Spending Makes for Poor Health
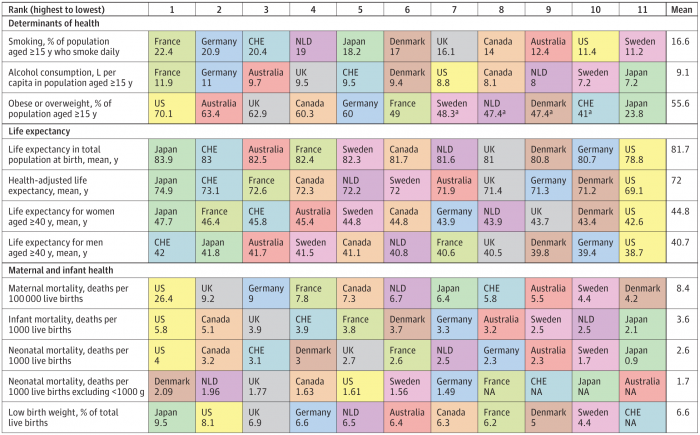
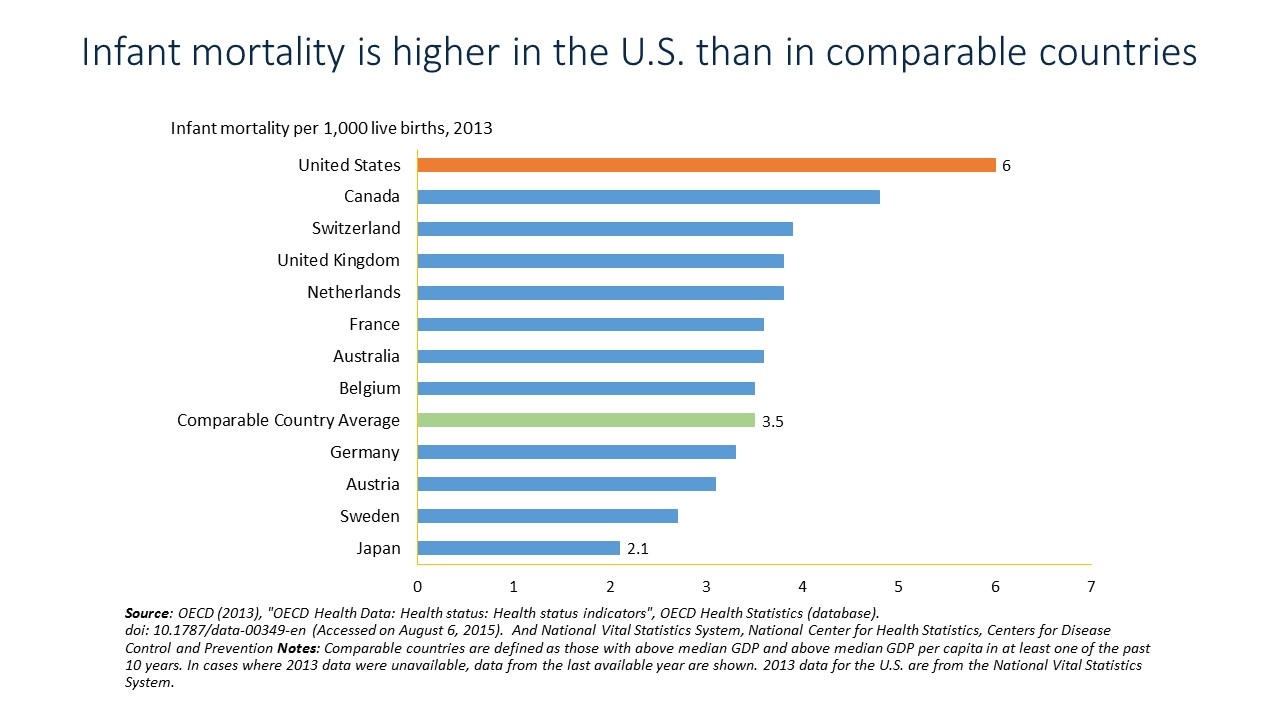
The U.S. spent nearly twice as much as other wealthy countries on healthcare, mostly due to higher prices for both labor and products (especially prescription drugs). And, America spends more on administrative costs compared to other high-income countries. What do U.S. taxpayers get in return for that spending? Lower life spans, higher maternal and infant mortality, and the highest level of obesity and overweight among our OECD peer nations. These sobering statistics were published in Health Care Spending in the United States and Other High-Income Countries this week in JAMA, the Journal of the American Medical Association. The study analyzes
Will People Enrolled in Medicaid Want to Be Amazon Prime’d?

Amazon is planning to extend Prime subscriptions to people enrolled in Medicaid for the discount price of $5.99 a month instead of the recent price increase to $12.99/month or $99 a year. The $5.99 a month calculates to a 27% break on the annual Prime membership cost. Medicaid enrollees who want to take advantage of the deal must provide Amazon with a scan or image of the card they use for their benefit (either Medicaid or EBT). These consumers can enroll annually, for a maximum of four years. Here’s what the Seattle Times, Amazon’s hometown newspaper, said about the program.
Getting Real About Social Determinants of Health
New research points out that real people live real lives, and our assumptions about social determinants of health (SDOH) may need to be better informed by those real lives. I read three reports in the past week sobering up my bullish #SDOH ethos dealing with food deserts, transportation, and health service access — three key social determinants of health. To remind you about the social determinants, here’s a graphic from Kaiser Family Foundation that summarizes the key pillars of SDOH. Assumption 1: Food deserts in and of themselves diminish peoples’ healthy nutrition lifestyles. Low-income households who are exposed to the same food-buying
The 2018 Edelman Trust Barometer – What It Means for Health/Care in America

Trust in the United States has declined to its lowest level since the Edelman Trust Barometer has conducted its annual survey among U.S. adults. Welcome to America in Crisis, as Edelman brands Brand USA in 2018. In the 2018 Edelman Trust Barometer, across the 28 nations polled, trust among the “informed public” in the U.S. “plunged,” as Edelman describes it, by 23 points to 45. The Trust Index in America is now #28 of 28 countries surveyed (that is, rock bottom), dropping below Russia and South Africa. “The public’s confidence in the traditional structures of American leadership is now fully
Calling Out Health Disparities on Martin Luther King Day 2018

On this day appreciating the legacy of Martin Luther King, Jr., I post a photo of him in my hometown of Detroit in 1963, giving a preliminary version of the “I Have a Dream” speech he would deliver two months later in Washington, DC. Wisdom from the speech: “But now more than ever before, America is forced to grapple with this problem, for the shape of the world today does not afford us the luxury of an anemic democracy. The price that this nation must pay for the continued oppression and exploitation of the Negro or any other minority group
U.S. Healthcare Spending & Outcomes in Five Charts: #EpicFail in the 2017 OECD Statistics
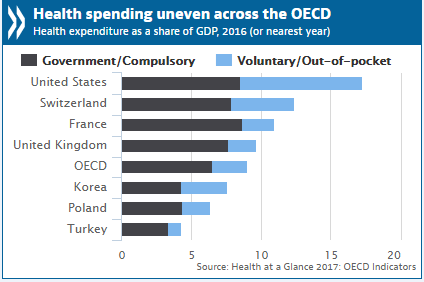
“Spend more. Get less.” If a retailer advertised using these four words, how many consumers would buy that product or service? This is the American reality of healthcare spending in 2016, told in the OECD report, Health at a Glance 2017. I present five charts from the study in this post, which together take the current snapshot health-economic lesson for the U.S. First, look at health expenditures as a share of gross domestic product: the U.S. is number one above Switzerland, France, and the UK, and about two times the OECD average. Note, too, the proportion of out-of-pocket and so-called
In the Post-Weinstein Era, How to Market Health to Women: Philips, Kalenji, and Libresse Getting It Right

“With Mad Men still in charge, ad campaigns miss the mark,” an editorial published this week in the Financial Times asserts. Leave it to a fiscally conservative British publication to be spot-on about a particularly, but not uniquely, American challenge, in this post-Weinstein (Miramax), -Price (Amazon), and today, -Halperin (MSNBC) moment of sexual harassment revelations. In health/care, women are key consumers, buyers and influencers, yet under-represented in the Mad Men demographic of senior advertising executives, as the data-driven FT essay points out. So it’s especially heartening to find this month a few examples of empowering, inspiring ad campaigns getting health/care marketing
Income Inequality For Older Americans Among Highest in the World – What This Means for Healthcare
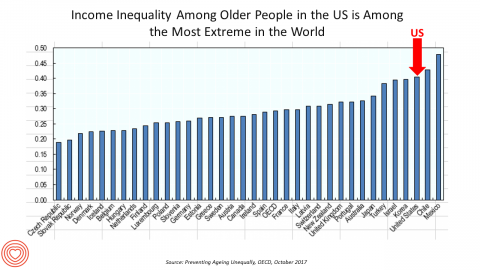
Old-age inequality among current retirees in the U.S. is already greater than in ever OECD country except Chile and Mexico, revealed in Preventing Ageing Unequally from the OECD. Key findings from the report are that: Inequalities in education, health, employment and income start building up from early ages At all ages, people in bad health work less and earn less. Over a career, bad health reduces lifetime earnings of low-educated men by 33%, while the loss is only 17% for highly-educated men Gender inequality in old age, however, is likely to remain substantial: annual pension payments to the over-65s today are
To Meet Health Consumers’ Digital Demands, Think Netflix and Verizon
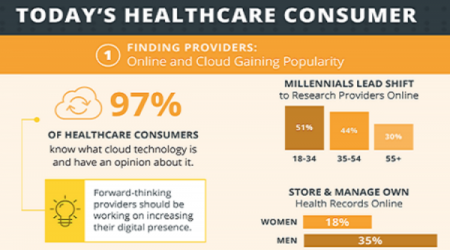
Health consumers have become savvy about the role of technology in their healthcare, according to a survey from Ambra, a company that is in the health cloud business. The survey paints a picture of health consumers hungry for digital health connections. The most popular activities patients do online for health were: To research symptoms and treatments To renew and/or fill prescriptions To view lab reports To make appointments To pay medical bills To correspond with the nurse or doctor To view imaging reports To get virtual care, and, To participate in patient communities. To meet patients where they want
Celebrating 10 Years of Health Populi, 10 Healthcare Milestones and Learnings

Happy anniversary to me…well, to the Health Populi blog! It’s ten years this week since I launched this site, to share my (then) 20 years of experience advising health care stakeholders in the U.S. and Europe at the convergence of health, economics, technology, and people. To celebrate the decade’s worth of 1,791 posts here on Health Populi (all written by me in my independent voice), I’ll offer ten health/care milestones that represent key themes covered from early September 2007 through to today… 1. Healthcare is one-fifth of the national U.S. economy, and the top worrisome line item in the American
Women’s Access to Health Care Improved Under the Affordable Care Act
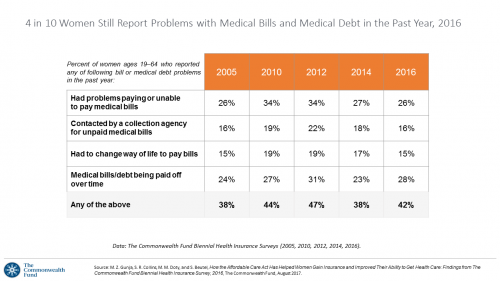
The Affordable Care Act (ACT) was implemented in 2010. Since the inception of the ACA, the proportion of uninsured women in the U.S. fell by nearly one-half, from 19 million in 2010 to 11 million in 2016. The Commonwealth Fund has documented the healthcare gains that American women made since the ACA launch in their issue brief, How the Affordable Care Act Has Helped Women Gain Insurance and Improved Their Ability to Get Health Care, published earlier this month. The first chart talks about insurance: health care plan coverage, which is the prime raison d’être of the ACA. It’s
Healthcare Quality and Access Disparities Persist in the U.S.
In 2015, poor and low-income people in America had worse health care than high-income households; care for nearly half of the middle-class was also worse than for wealthier families. Welcome to the 2016 National Healthcare Quality and Disparities Report from the Agency for Healthcare Research and Quality (AHRQ). The report assesses many measures quantifying peoples’ access to health care, such as uninsurance rates (which improved between 2010 and 2016), and quality of health care — including person-centered care, patient safety, healthy living, effective treatment, care coordination, and care affordability. While some disparities lessened between 2000 and 2015, disparities
Most Americans, Including Republicans, Want President Trump’s Administration to Make the ACA Work – Not Fail
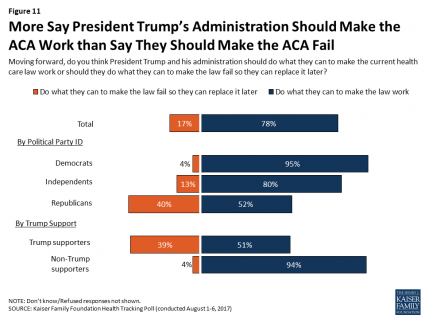
8 in 10 Americans want President Trump and his administration to do what they can to make the Affordable Care Act work, according to the latest August 2017 health tracking poll from Kaiser Family Foundation (KFF). By political party affiliation, this includes 95% of Democrats, 80% of Independents, and 52% of Republicans (that is, to emphasize the point, just over half, a majority, of Republicans). More Americans are also relieved and happy, versus disappointed and angry, that the ACA repeal did not occur (thus far), the second chart illustrates. To be sure, a majority of Republicans register anger and disappointment,
Health Equity Lessons from July 23, 1967, Detroit
On July 23, 1967, I was a little girl wearing a pretty dress, attending my cousin’s wedding at a swanky hotel in mid-town Detroit. Driving home with my parents and sisters after the wedding, the radio news channel warned us of the blazing fires that were burning in a part of the city not far from where we were on a highway leading out to the suburbs. Fifty years and five days later, I am addressing the subject of health equity at a speech over breakfast at the American Hospital Association 25th Annual Health Leadership Summit today. In my talk,
Fix the ACA, Most Americans Say
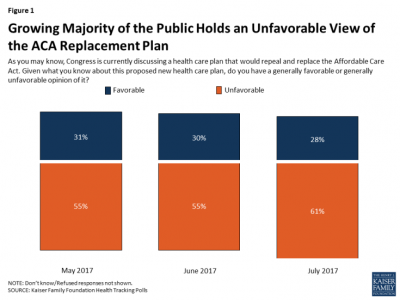
61% of Americans hold negative views of repealing-and-replacing the Affordable Care Act, according to the July 2017 Health Tracking Poll from the Kaiser Family Foundation. This month’s survey focused on Americans’ views on Republican legislative efforts to repeal and replace the Affordable Care Act (ACA). As of the writing of this post, the majority of the Senate rejected the full repeal of the ACA, but the situation is very fluid. Note that this poll was conducted by phone between July 5-10, 2017, among 1,183 U.S. adults ages 18 and older. The column chart here illustrates that the proportion of people
Note to Mooch: The ER is Not Universal Health Care
I quote directly from the Twitter feed of Anthony Scaramucci, @scaramucci: “@dhank2525 agree. We already have Univ Health Care, we made decision long ago to treat everyone that enters an emergency room.” Mr. Scaramucci is President Trump’s Communications Chief, replacing Sean Spicer. Mr. Scaramucci is neither veteran journalist nor healthcare policy wonk. He’s a successful businessman, which I respect for his savvy and ability to build a fund, attract investors, and create a media persona which he has telegenically broadcast on CNBC and elsewhere over the past decade. He’s got a engaging public personality, and goes by the moniker, “Mooch.” But
Is There Political Will for Healthcare Access in the US?
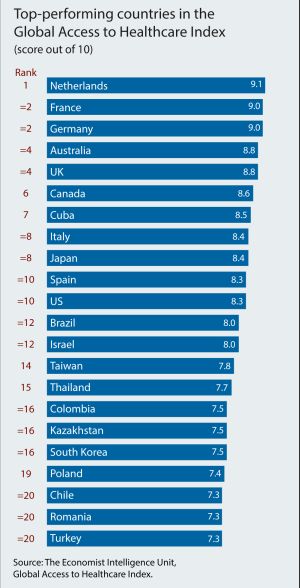
The Netherlands, France and Germany are the best places to be a patient, based on the Global Access to Healthcare Index, developed by the Economist Intelligence Unit (EIU). Throughout the world, nations wrestle with how to provide healthcare to health citizens, in the context of stretched government budgets and demand for innovative and accessible services. The Global Access to Healthcare Index gauges countries’ healthcare systems in light of peoples’ ability to access services, detailed in Global Access to Healthcare: Building Sustainable Health Systems. The United States comes up 10th in line (tied with Spain) in this analysis. Countries that score the
Amazon’s Health Care Building Blocks

In the past few weeks, two announcements from Amazon point to a strategy, whether intended or my dot-connecting, that the ecommerce leader has the health of its customers in its sights. In late May, CNBC first published the news that Amazon was seeking out a candidate to be a general manager for a pharmacy business. Here’s the video telling the story. Getting into the retail pharmacy channel is in itself a huge message to this health industry segment, which is very competitive between chain pharmacies (led by CVS, Walgreens, and Rite-Aid), grocery pharmacies (the largest of which are Kroger and
12% of Americans Have At Least 5 Chronic Conditions and Spend 41% of Healthcare Dollars
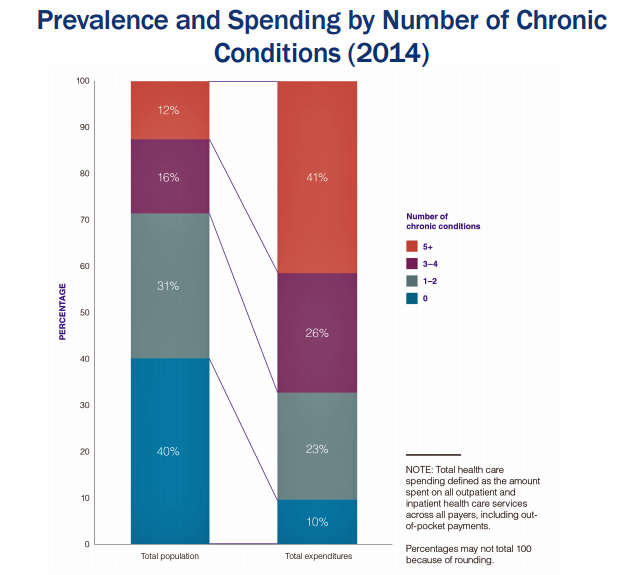
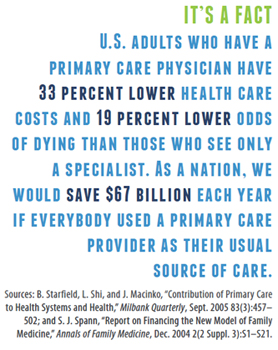
Forget about the 80/20 Rule. Welcome to the 41/12 Metric: 12% of U.S. adults account for 41% of healthcare spending in America, calculated by RAND Corporation in their new report, Multiple Chronic Conditions in the United States. RAND’s report quantifies the growing chronic care landscape in America that will be a burdensome legacy for younger Americans in terms of financial and social costs. First, a definition: RAND defines a chronic condition as a physical or mental health issue that lasts more than one year and causes functional restrictions or requires ongoing monitoring or treatment. Older adults are more likely to
Shopping Food for Health is Mainstream, But Nutrition Confusion is Super-Sized
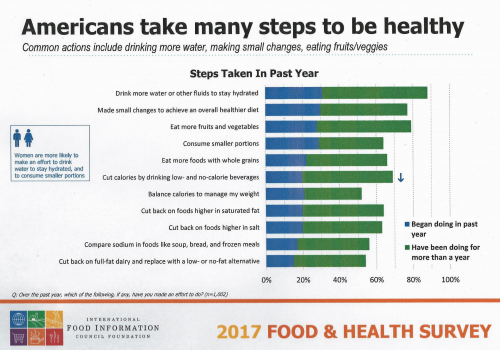
Americans are overwhelmingly keen to use food for their health, and overwhelmed by the amount of nutrition information they face to make good shopping and eating decisions. Welcome to “food confusion,” a phenomenon gleaned from the 12th Annual Food and Health Survey conducted by the International Food Information Council Foundation (IFIC). This 12th annual survey from IFIC finds that most Americans take many steps to be healthy. In the past year, the most popular health-steps include drinking more for hydration, making small changes to achieve a healthier diet, consuming smaller portions, eating more fruits and vegetables, and eating more whole grains.
Americans Say Healthcare is the Nation’s #1 Problem – Tied with Dissatisfaction with Government
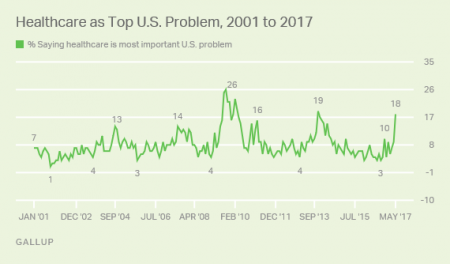
Healthcare tops the list of Americans’ concerns, tied with a dissatisfaction for government, this month (May 2017). According to a Gallup poll published 12 May, poor government leadership and healthcare are together the most important problem currently facing the U.S. Immigration, the economy, jobs, and race relations are distance 3rd places in this survey, which was conducted during the first week of May 2017 among 1,011 U.S. adults 18 years and older. The highest percent of Americans citing healthcare as America’s most important problem was 26%, found in August/September 2008 when town hall meetings round the country were protesting healthcare
Healthier Eating Is the Peoples’ Health Reform: the Gallup-Sharecare Well-Being Index

The top healthiest eating communities tend to circle the perimeter of the map of the lower 48 U.S. states. In these towns, more than 72% of health citizens report healthy eating. These areas are located in California, Florida, and Massachusetts, among others. Areas with the lowest rates of healthy eating are concentrated generally south of the Mason-Dixon Line, in places like Arkansas, Kentucky, and Mississippi, and other states. In these places, fewer than 57% of people eat healthy. Eating healthy foods in moderation is a mighty contributor to personal and public health, discussed in the report, State of American Well-Being
The Power of Joy in Health and Medicine – Learning From Dr. Regina Benjamin

Former Surgeon General Dr. Regina Benjamin was the first person who quoted to me, “Health isn’t in the doctor’s office. It’s where people live, work, play and pray,” imparting that transformational mantra to me in her 2011 interview with the Los Angeles Times. I wrote about that lightbulb moment here in Health Populi. Dr. Benjamin was the 18th Surgeon General, appointed by President Obama in 2009. As “America’s Doctor,” she served a four-year term, her mission focused on health disparities, prevention, rual health, and children’s health. Today, Dr. Benjamin wears many hats: she’s the Times Picayune/NOLA.com professor of medicine at
Health Inequity in the United States – A View From Across the Pond
The statistics on the health of people living in America illustrate a divide between have’s and have-not’s. Average life expectancy is lower in the US compared with other wealthy nations: the wealthiest Americans live 10 to 15 years longer than the poorest, according to a landmark article in JAMA from 2016 studying the relationship between income inequality and mortality. See the first chart: this illustrates that people living in the US whose income reaches the top 95th percentile far outlive folks in the bottom 5th percentile of income. I find myself in London, England, this week, across the Pond (that is,
States That Expanded Medicaid Improved Healthcare Access & Patient Outcomes
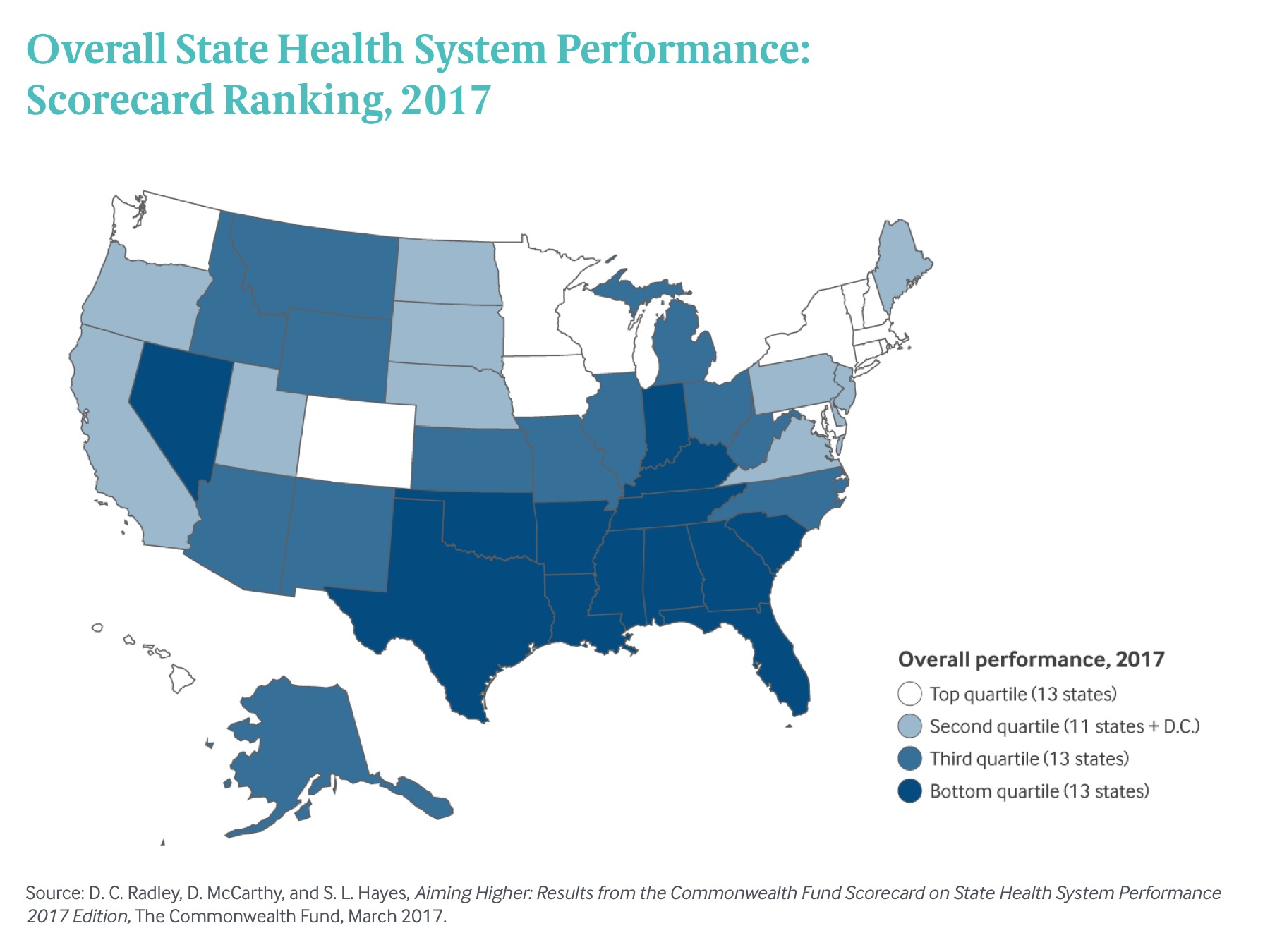
States that expanded Medicaid since the start of the Affordable Care Act made greater health system access improvements than those States that did not expand Medicaid, according to Aiming Higher: Results from the Commonwealth Fund Scorecard on State Health System Performance. There’s good news and bad news in this report: on the upside, nearly all states saw health improvements between 2013 and 2015, and in particular, for treatment quality and patient safety. Patient re-admissions to hospitals also fell in many states. But on the downside, premature deaths increased in nearly two-thirds of states, a reversal in the (improving) national mortality
Americans Are Not Sold On the American Health Care Act
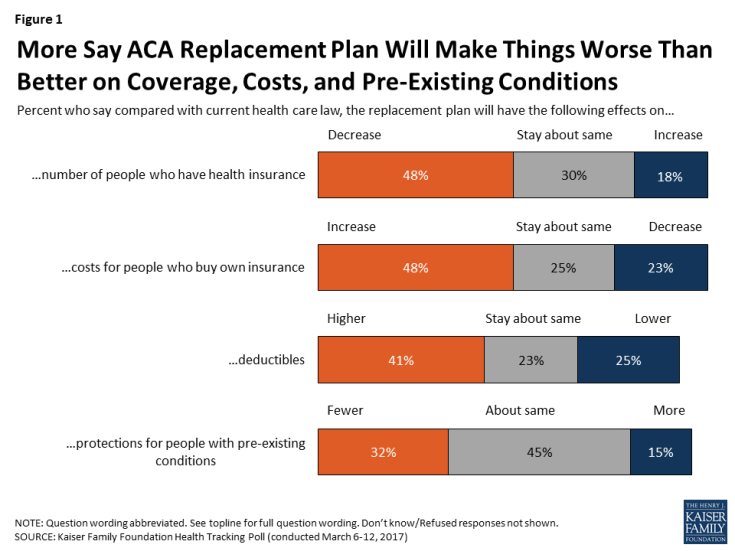
Most Americans do not believe that TrumpCare, the GOP plan to replace the Affordable Care Act (the ACA, aka ObamaCare), will make things better for U.S. health citizens when it comes to peoples’ health insurance coverage, the premium costs charged for those health plans, and protections for people with pre-existing medical conditions. The March 2017 Kaiser Family Foundation Health Tracking Poll examined U.S. adults’ initial perceptions of AHCA, the American Health Care Act, which is the GOP’s replacement plan for the ACA. There are deep partisan differences in perceptions about TrumpCare, with more Republicans favorable to the plan — although not
Your Zip Code Is Your Wellness Address

Geography is destiny, Napoleon is thought to have first said. More recently, the brilliant physician Dr. Abraham Verghese has spoken about “geography as destiny” in his speeches, such as “Two Souls Intertwined,” The Tanner Lecture he delivered at the University of Utah in 2012. Geography is destiny for all of us when it comes to our health and well-being, once again proven by Gallup-Healthways in The State of American Well-Being 2016 Community Well-Being Rankings. The darkest blue circles in the U.S. map indicate the metro areas in the highest-quintile of well-being. The index of well-being is based on five metrics, of consumer self-ranking
Stress Is A Social Determinant of Health – Money and Politics Top the List in 2017

The American Psychological Association reports that Americans are experiencing greater levels of stress in 2017 for the first time since initiating the Stress in America Survey ten years ago in 2007. This is a statistically significant finding, APA calculated. The member psychologists of the American Psychological Association (APA) began to report that patients were coming to appointments increasingly anxious about the 2016 Presidential election. So the APA polled U.S. adults on politics for the first time in ten years of conducting the Stress in America survey. Two-thirds of Americans are stressed and/or anxious about the future of the nation, and
How Amazon Has Primed Healthcare Consumers

We are all Amazon Prime primed as consumers now. So it should not surprise healthcare providers, plans and suppliers that consumers expect just-in-time convenience for their healthcare, Accenture has found. Mind the gap: 8 in 10 U.S. patients would welcome some aspect of virtual healthcare, but only 1 in 5 providers is meeting that need. The consumer demand for virtual care is palpable for: Tracking biometrics, among 77% of consumers (say, for measuring blood pressure or blood glucose for people managing diabetes) Following up appointments, for 76% of people after seeing a doctor or being discharged from hospital Receiving reminders
The Health Disparity of Information Access
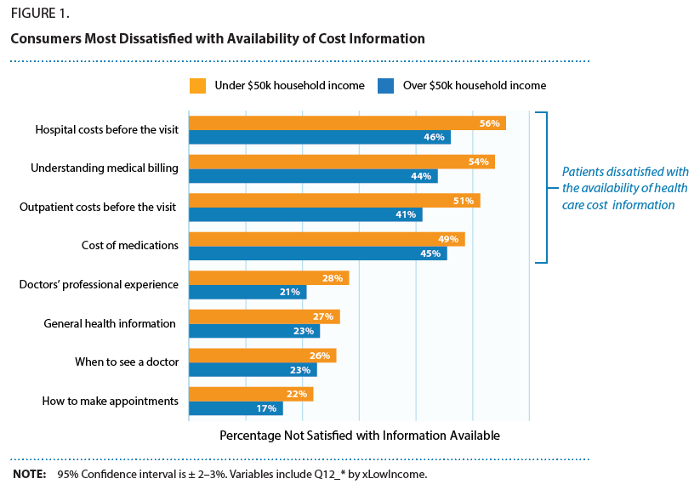
Among many health disparities which mar healthcare quality in the United States, there’s another one to add to the list: health and healthcare information access. Access to health care is underpinned in large part on a health consumer’s access to information about available health care services, their location, price, and if the patient is very fortunate to glean, quality. As people take on more responsibility for managing their health care utilization and financing in America, their access to information that is easy-to-find, clear, comprehensive and current is critical to personal and public health outcomes. But consumers are dissatisfied with the
Replacing Opioids with Digital Tech for Pain at CES 2017

Pain management is a growing story at CES 2017. I covered the topic of Sleep and Pain at CES one year ago in the Huffington Post, and this year, the category has grown in both number of innovations and mode of pain management. At CES 2017, there were exhibitors of FDA-approved devices, sleep-and-pain focused tech, wristbands for relaxation and nausea-management, and a $5,999 device for calming meditation that’s being used in addiction programs. What’s driving growth and acceptance of this health tech segment is the opioid crisis which has become a public health epidemic across the U.S. The maps with increasing orange
The Digital Health Gap For High-Cost, High-Need Patients
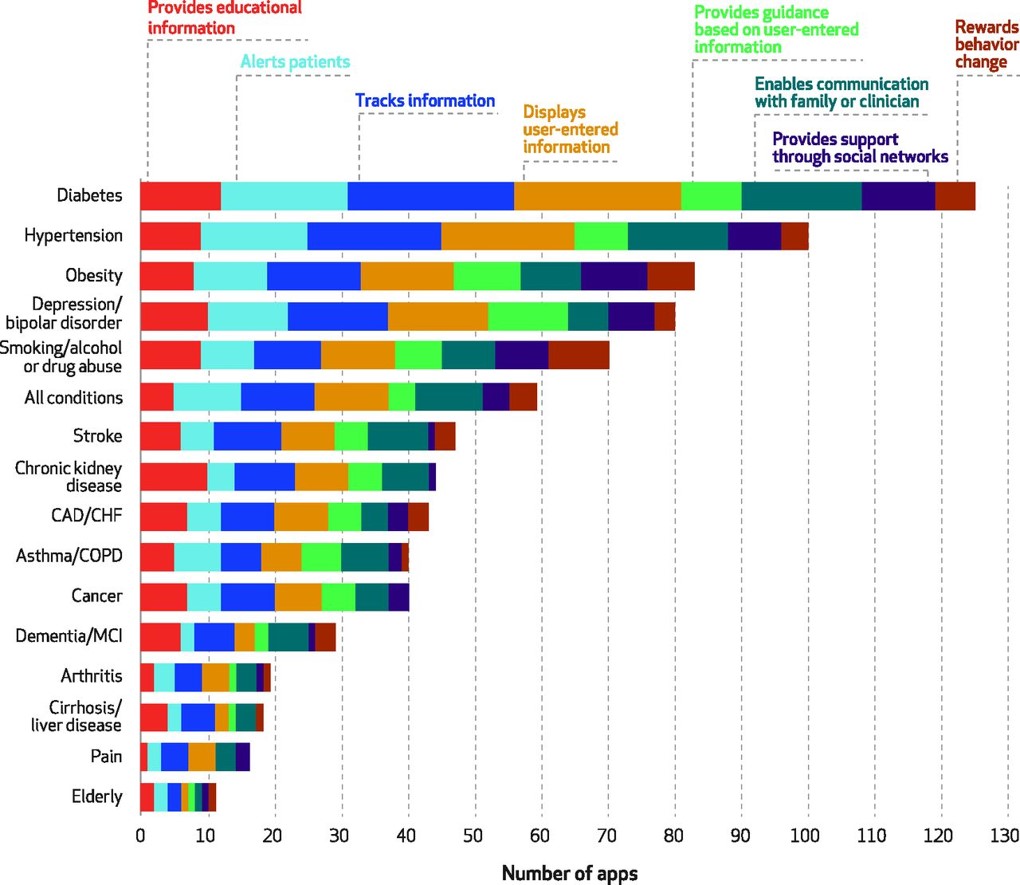
Several market forces are converging that boost patients’ ability to engage in their health and self-care, including peoples’ growing adoption of smartphones, demand for self-service and DIY lifestyles, and Americans’ growing responsibility as health consumers. Health consumers are using a growing array of self-health tools, enabled through digital technologies. However, these tools aren’t yet engaging some of the very people who need them the most: high-need, high-cost patients. Research into this situation is discussed in the December 2016 Health Affairs article, Many Mobile Heaath Apps Target High-Need, High-Cost Populations, But Gaps Remain, published in the December 2016 issue of Health Affairs. For
1 in 3 Americans Still Self-Rations Healthcare
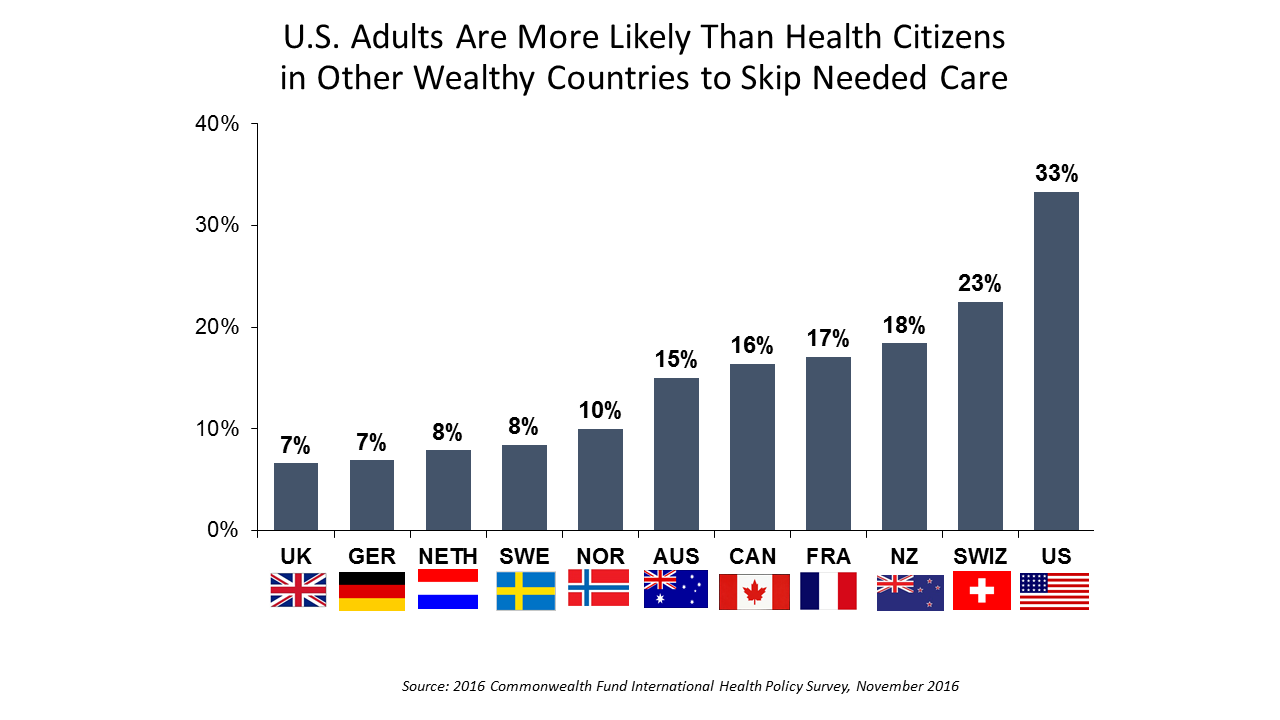
People in the U.S. are much more likely to go without health care they need compared with health citizens in 10 other wealthy countries, according to the Commonwealth Fund’s 2016 international survey. One-third of Americans did not seek care due to costs, including going without recommended care, failing to fill a prescription drug, and/or not seeing a doctor when sick. While this self-rationing proportion of Americans dropped from 37% in 2013, the U.S. still ranks #1 in foregoing necessary healthcare due to cost. “In comparison to adults in the other 10 countries, adult sin the U.S. are sicker and more
Healthcare Reform in President Trump’s America – A Preliminary Look

It’s the 9th of November, 2016, and Donald Trump has been elected the 45th President of the United States of America. On this morning after #2016Election, Health Populi looks at what we know we know about President Elect-Trump’s health policy priorities. Repeal-and-replace has been Mantra #1 for Mr. Trump’s health policy. With all three branches of the U.S. government under Republican control in 2018, this policy prescription may have a strong shot. The complication is that the Affordable Care Act (aka ObamaCare in Mr. Trump’s tweet) includes several provisions that the newly-insured and American health citizens really value, including: Extending health
Americans Have Begun to Raid Retirement Savings for Current Healthcare Costs
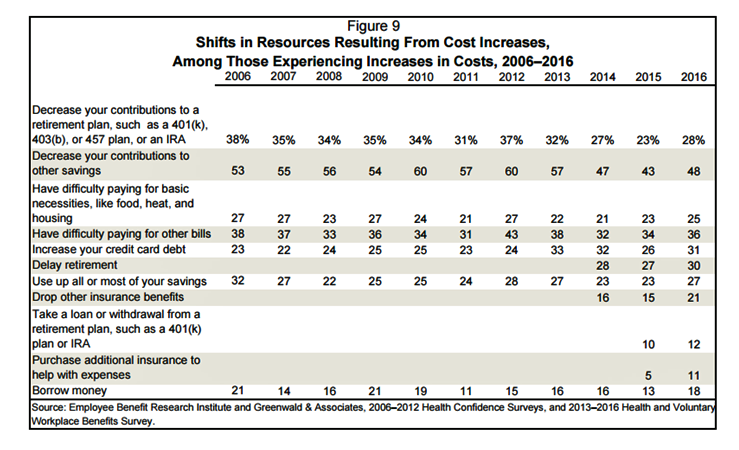
While American workers appreciate the benefits they receive at work, people are concerned about health care costs. And consumers’ collective response to rising health care costs is changing the way they use health care services and products, like prescription drugs. Furthermore, 6 in 10 U.S. health citizens rank healthcare as poor (27%) or fair (33%). This sober profile on healthcare consumers emerges out of survey research conducted by EBRI (the Employee Benefit Research Institute), analyzed in the report Workers Like Their Benefits, Are Confident of Future Availability, But Dissatisfied With the Health Care System and Pessimistic About Future Access and
The Drug Epidemic-Testing and Data Arm the Battle
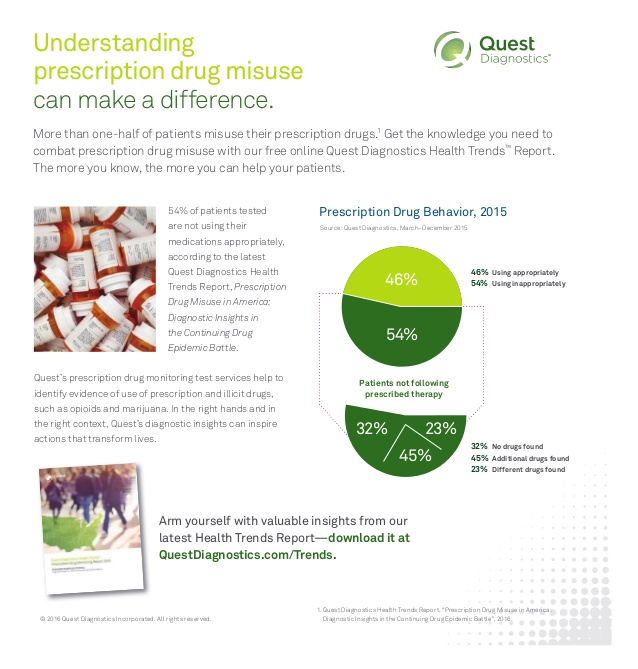
More than 40 Americans die every day from prescribed opiate overdoses, Dr. Tom Frieden of the CDC has recognized. The harms of pain-killing drugs have been substantial: Dr. Frieden observed, “the prevalence of opioid dependence may be as high as 26% among patients in primary care receiving opioids for chronic non-cancer-related pain.” There were more deaths due to drug overdoses in 2014 than in any previous year, 61% of which involved opioid pain relieving medications such as oxycodone and hydrocodine, and heroin which has grown in use over the past few years. The CDC has recommended that healthcare providers do
Broadband – A Social Determinant of Health
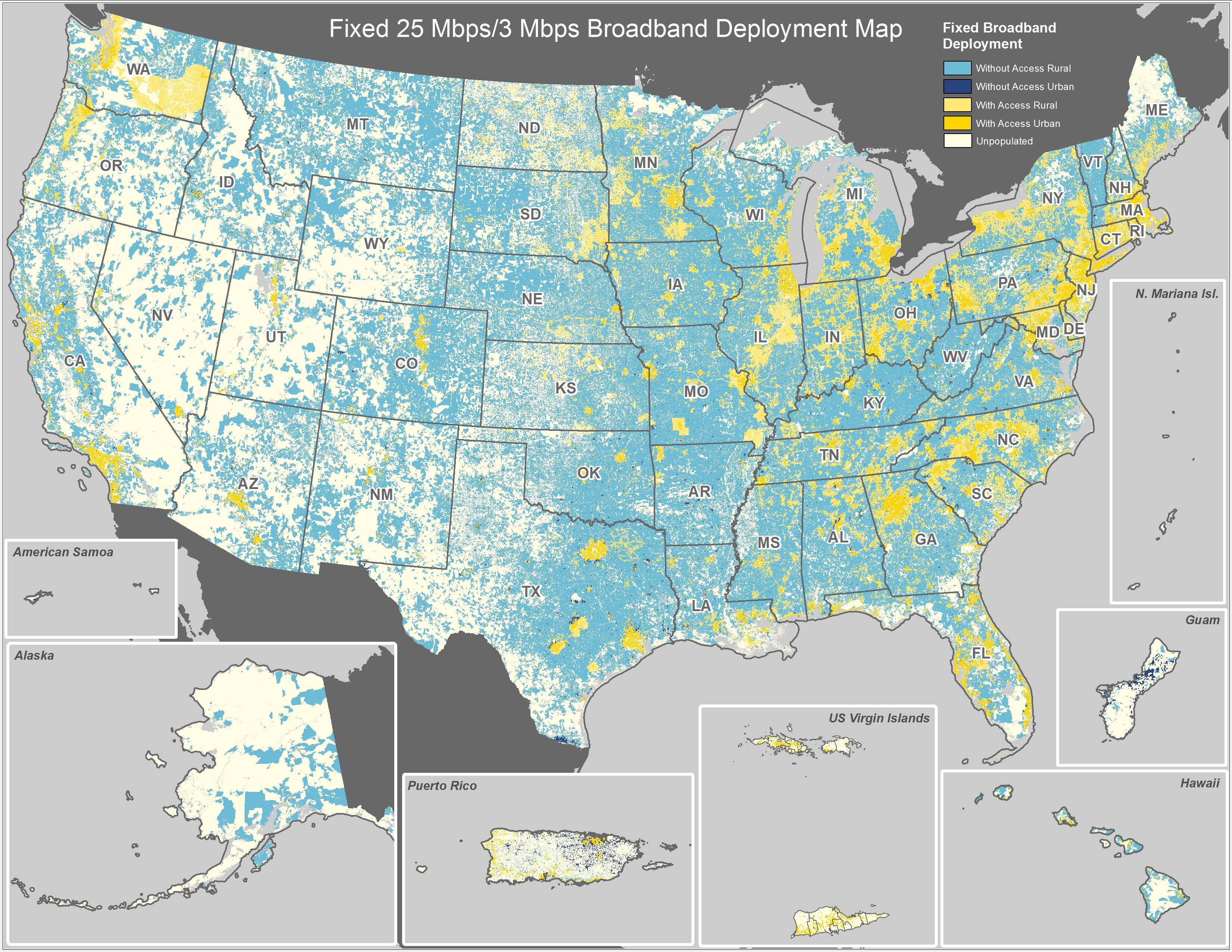
The promise of digital, connected health to engage all health citizens cannot be fully realized until people have access to the new social determinant of health: broadband connectivity. The World Health Organization considers social determinants of health inputs like education, safe drinking water, nutritious food, safe neighborhoods for walking, employment and transportation access. Together, these factors bolster personal/individual and public health. See the map of the U.S., and note whee the concentrations of aqua blue are. These are areas that lack broadband access. Telehealth and other digital health tools can get health care to under-served people in under-served geographic areas….where broadband
Health in America: Improving, But Disparities Need Policy Prescriptions
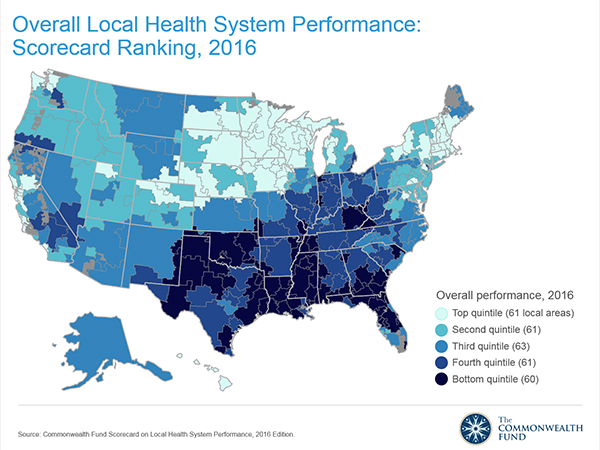
The bad news: mortality rates haven’t improved much and obesity rates rose in one-third of communities. The good news: public health gains can be made in resource-poor communities with the right health policies, based on research from The Commonwealth Fund, Rising to the Challenge, the Fund’s Scorecard on local health system performance for 2016. The top-line of this benchmark report is that health care in the U.S. has, overall, improved more than it’s declined. Among the big levers driving health care improvement in the past year have been the further expansion of health citizens covered with insurance through the Affordable
The Health Disparities of Being Gay
#PrayForOrlando The club Pulse, site of the biggest mass gun shooting in U.S. history, was named to honor one of the co-owner’s brothers, who succumbed to AIDS in 1991. In today’s Health Populi, I soberly ponder the lost lives in the Orlando massacre of people who joyfully convened in a safe haven to celebrate life, liberty, and their pursuits of happiness. Over fifty people ended up dead, and there will be more mortalities as the health workers at Orlando Regional Medical Center continue to fight the post-trauma battle to save gunned-down lives. We define “health” broadly in Health Populi and
For Healthcare Costs, Geography is Destiny
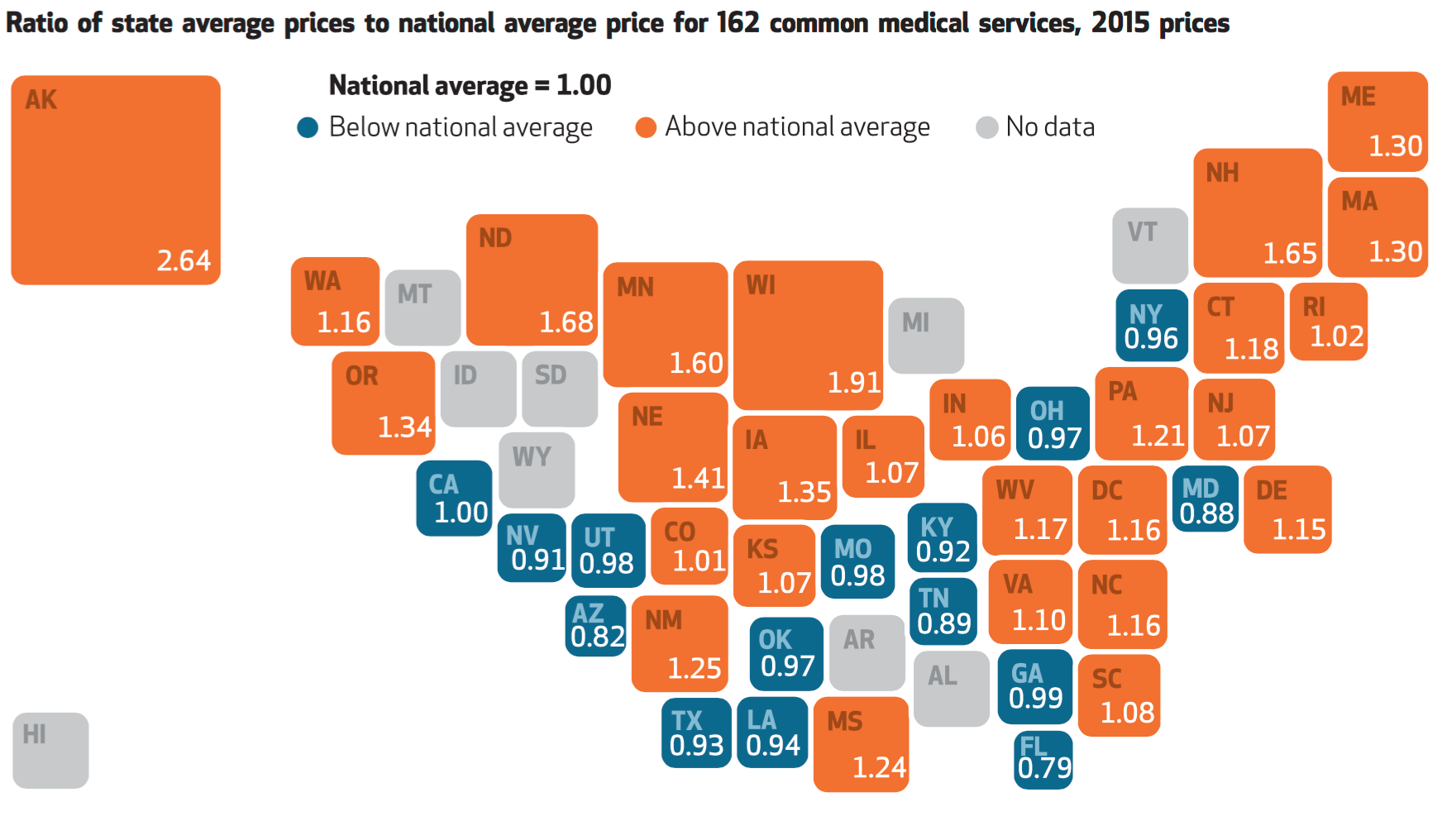
Where you live in America determines what you might pay for healthcare. In this health economic scenario, as Napoleon is rumored to have said, “geography is destiny.” If you’re searching for low-cost health care, Ohio may just be your state of choice. The map illustrates these health care disparities across the U.S. in 2015, when the price of a single service could vary by more than 200% between one state and another: say, Alaska versus Arizona, or Wisconsin compared to Florida. Even within states, like Ohio, the average price of a pregnancy ultrasound in Cleveland ran nearly three times that received in
Rural Hospitals in America – Health Disparities, Hospital Disparities
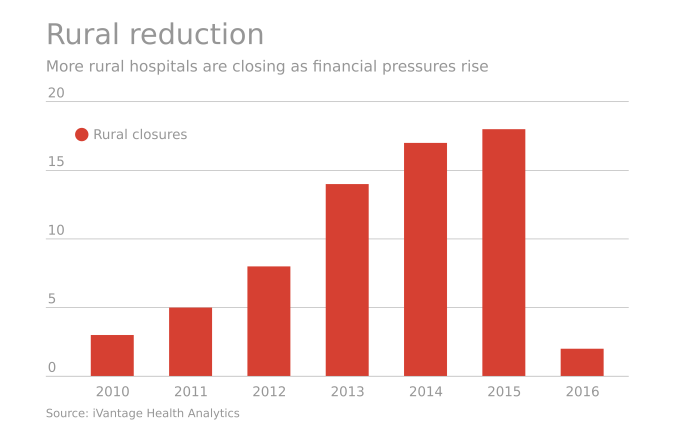
Rural hospitals operating in the U.S. have a higher risk of mortality — closure — than other hospitals in America. The U.S. health care landscape is littered with examples of health disparities among the nation’s health citizens – for example, women’s lower access to heart-health care, Latinos’ higher rates of Type 2 Diabetes, and African-Americans’ greater risks of stroke, many cancers, maternal mortality, and many other causes of mortality and diminished health. A report from iVantage, Rural Relevance – Vulnerability to Value, documents the fiscally challenging environment for rural hospitals in America. There are at least 673 facilities at-risk of closure
Building Health Bridges — Health:Further Goes Beyond the Disruptive

Most people in the U.S. acknowledge that their richest country in the world has a broken healthcare system, especially when it comes to costs. A handful of think tanks and lawmakers offer fixes for American healthcare. Now there’s a new problem-solver in healthcare town, Health:Further, and they aim to move U.S. health forward by building bridges between stakeholders in the U.S. health ecosystem. My longtime colleague and friend, Andre Blackman of Pulse+Signal, has joined the organization as “Producer.” Here, we’ll learn more from my (JSK) interview with Andre (AB) about the organization, their mission, and plans to go beyond “disruption”
Let’s Make a Deal: Patients Weigh Privacy Paybacks
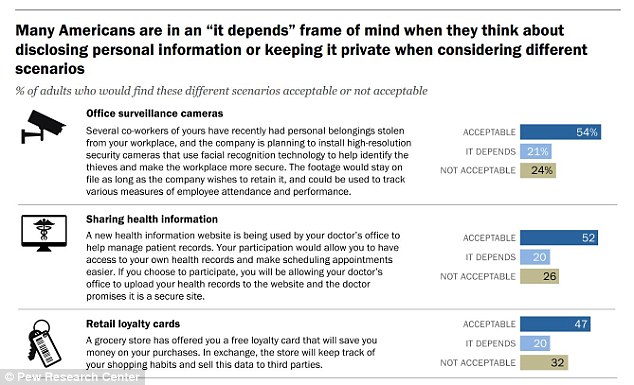
“It depends” is the hedge-phrase that characterizes how Americans see disclosing personal information versus keeping private information private, according to the consumer survey report, Privacy and Information Sharing, published by the Pew Research Center (PRC) in January 2016. U.S. adults see a privacy trade-off, living in the convenience-context of 21st century digital economy in exchange for some form of value. The “it depends” is a factor of what kind of data is geing collected, especially by third parties, how long that data area retained, for what use — vis-à-vis what a person is trading in return which could be a hard dollar
Retailers will morph into health destinations in 2016
Retailers in the U.S. are morphing into health destinations in 2016. Members of Target’s management team attended the 2016 Consumer Electronics Show (CES) and shared their perspectives in the company blog. Among the Target teams observations came from the Chief Marketing Officer, Jeff Jones, who observed, “A tidal wave of newness is coming to fitness technology and many companies are on the cusp of changing the game. From nutrition and sleep to how you exercise, it’s all going to be measured, linked and tracked. Wearables are here to stay and getting smarter every year.” The Senior Vice President for Hardlines,
Talking Infant Mortality At the 2016 Consumer Electronics Show
The rate of infant mortality — that is, babies dying in their first year of life — in the United States ranks lowest among the world’s developed countries, and below some less wealthy nations, as well. Shiny new things for digital health will be launching at the 2016 CES, the Consumer Electronics Show, in Las Vegas this week. And in the midst of virtual reality devices, connected cars, drones, and 4K TVs, I’ll be moderating a panel to kick off the Digital Health Summit at CES on Thursday focusing on The Wizards of Maternal Health — and how digital +
The 2016 THINK-Health Health/Care Forecast
It’s time to get the tea leaves out and mash up trends in my world of health, health care, technology, policy and people for 2016. We’ll start with the central player: people, consumers, patients, caregivers all. Health consumerism on the rise. People – call us patients, consumers, caregivers – will take on even more financial and clinical decision making risk in 2016. Growing penetration of high-deductible and consumer-driven health plans will push (not just nudge) people into the role of health care consumers, and the emerging businesses and programs serving the transparency market for price and quality will gain traction
The Internet of Healthy Things According to Dr. Kvedar
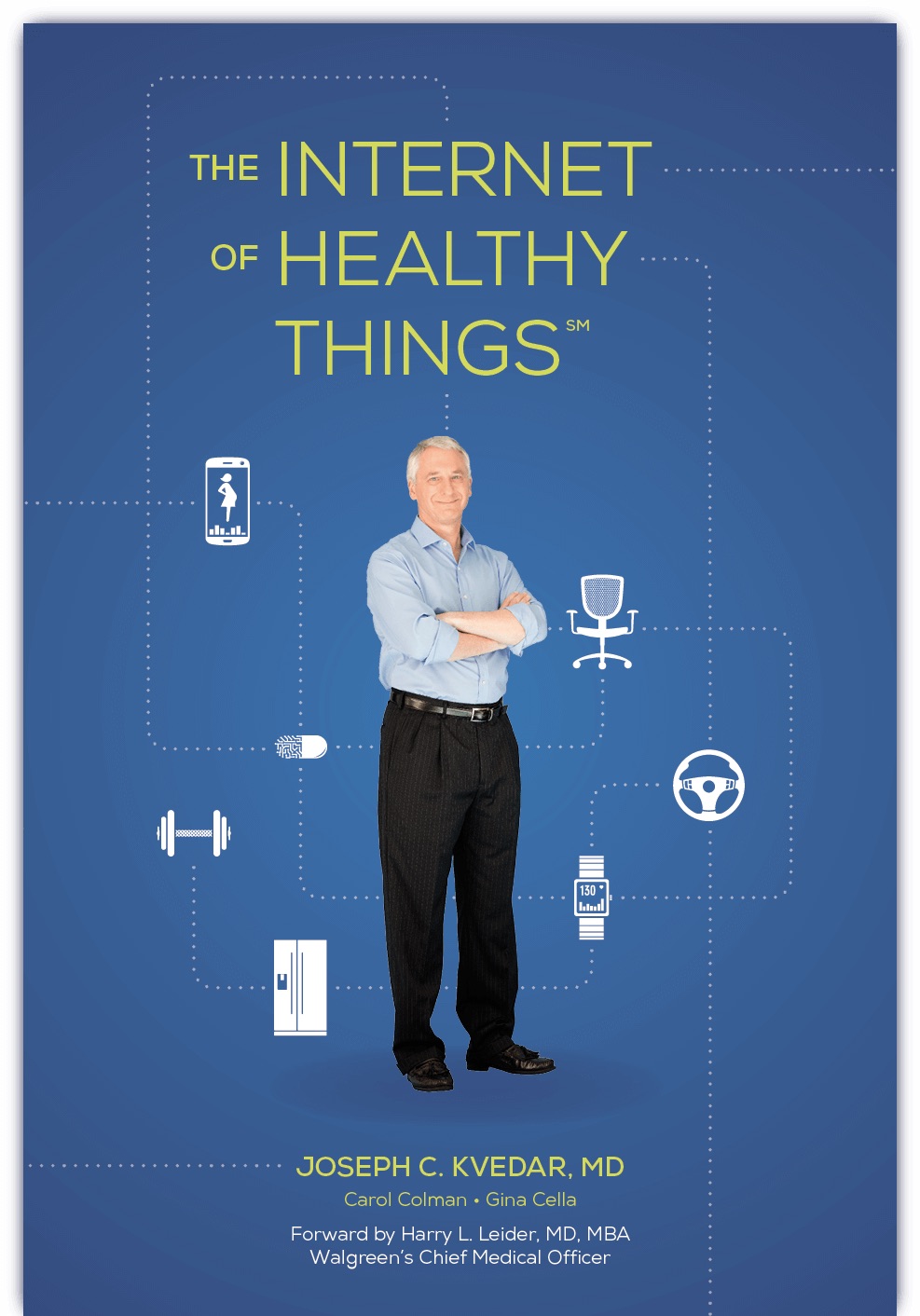
By 2020, according to the World Economic Forum, more than 5 billion people and 30 billion “things” will be connected to the Internet — cars, refrigerators, TVs, washing machines and coffeemakers, among those 5 bn folks’ electronic stuff. But so will medical devices, activity trackers, and a host of sensor-enabled “things” to help people and clinicians optimize health and manage illness. The Internet of Things (IoT) phenomenon, which is already penetrating households with energy management and security applications, is reaching health care. One of the pioneers in this connected health market is Dr. Joseph Kvedar, who leads the Center for
Getting to Connected Health Is A Marathon, Not A Sprint
Consumers may demand connected experiences in daily living, but there have been many barriers to health care industry stakeholders delivering on that expectation: among them, privacy and security concerns, and provider resistance. This demand-and-supply chasm is noted in Deloitte’s Center for Health Solutions’ latest look into the healthcare landscape, Accelerating the adoption of connected health. The objectives of connected health, or cHealth, are: To improve digital connectivity among consumers, providers, health plans and life sciences companies To facilitate self-managed care in a secure environment that protects privacy To deliver care outside of traditional institutional settings To enable chronic care management
U.S. Health At A Glance – Not So Healthy
People in the U.S. have lower life expectancy, a growing alcohol drinking problem, and relatively high hospital inpatient rates for chronic conditions compared with other OECD countries. And, the U.S. spends more on health care as a percent of GDP than any other country in the world. This isn’t new-news, but it confirms that U.S. health citizens aren’t getting a decent ROI on health spending compared with health citizens around the developed world. In the OECD’s latest global look at member countries’ health care performance, Health at a Glance 2015, released today, the U.S. comes out not-so-healthy in the context
The rise and rise of noncommunicable diseases
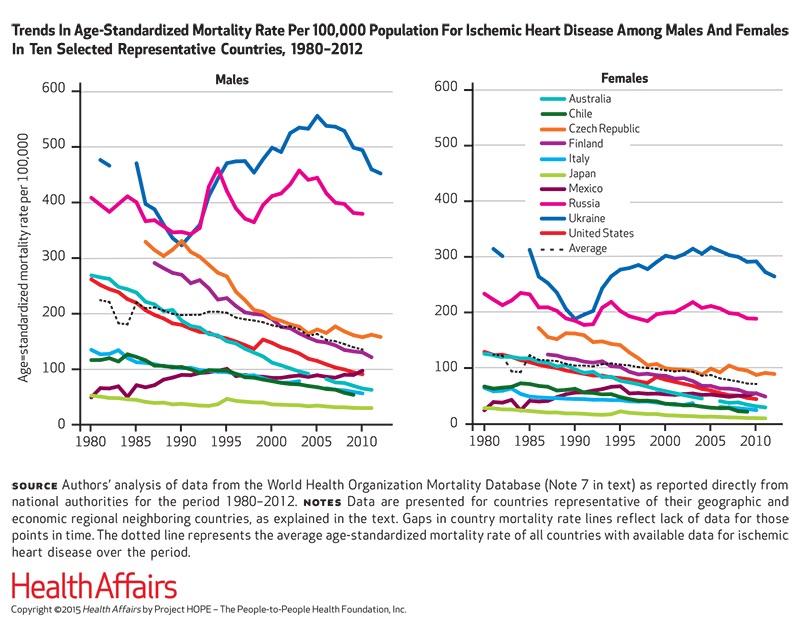
Noncommunicable diseases (NCDs) are the #1 cause of death in the world. NCDs are the yin to the yang of infectious diseases. Mortality from infectious disease has fallen as national economies have developed, while NCDs such as heart disease, respiratory disease, cancer, diabetes, and other NCDs are a growing burden. Health Affairs devotes its September 2015 issue to The Growing Burden of Noncommunicable Diseases, featuring research focusing both on global trends and U.S.-specific challenges. In their look into the relationships between NCDs, unhealthy lifestyles and country wealth, Thomas Bollyky et. al. note that NCDs aren’t only the “diseases of affluence,”
How Growing Income Inequality Hurts Everyone, and Especially Our Health
Income inequality has increased in most developed countries, and especially in the U.S., according to the OECD’s report, In It Together: Why Less Inequality Benefits All, published in May 2015. The red arrow in the first chart shows where the U.S. ranks versus other developed nations in income inequality, which is defined as the wealth gap between rich and poor people. The U.S. has the greatest income inequality in the developed world. The second chart shows data for the U.S. on benefits provided to low-wage workers (the bottom 25% of wage earners) versus high-wage workers (the top 25% of earners).
What Mavis Staples taught us about health at SXSW
While I am all health, all-the-time when I’m at the annual South-by-Southwest meet-up in Austin, I had the opportunity to attend the premiere of the documentary, Mavis! (exclamation point included and appropriate, given the energy and joy in the title’s subject). “Mavis” is Mavis Staples, who you should know for her music, as singer with her family’s group, The Staple Singers; and, for as a positive force for good. In fact, she’s a lesson in whole health, which is why I’m writing about here on Health Populi which is dedicated to health where we live, work, play, pray…and sing. For
A health agenda comes to the 2015 Oscars
The 87th annual 2015 Oscars show (#Oscars15) feted more than the movie industry: the event celebrated health in both explicit and subtle ways. Julianne Moore took the golden statuette for Best Actress, playing the title role in Still Alice, the story a woman diagnosed with early-onset Alzheimer’s Disease. In accepting her award, Moore spoke of the need to recognize and “see” people with Alzheimer’s – so many people feel isolated and marginalized, Moore explained. Movies help us feel seen and not alone – and people with Alzheimer’s need to be seen so we can find a cure, she asserted. See Moore’s lovely
Telehealth is in demand, driven by consumer convenience and cost – American Well speaks
Evidence of the rise of retail health grows, with the data point that on-demand health care is in-demand by 2 in 3 U.S. adults. American Well released the Telehealth Index: 2015 Consumer Survey, revealing an American health public keen on video visits with doctors as a viable alternative to visiting the emergency room. Virtual visits are especially attractive to people who have children living at home. [For context, this survey defines “telehealth” as a remote consultation between doctor and patient]. Convenience drives most peoples’ interest in telehealth: saving time and money, not leaving home if feeling unwell, and “avoiding germs
Thinking about health disparities on Martin Luther King Day 2015
On this day celebrating Martin Luther King, Jr., I post a photo of him in my hometown of Detroit in 1963, giving a preliminary version of the “I Have a Dream” speech he would give two months later in Washington, DC. As I meditate on MLK, I think about health equity. By now, most rational Americans know the score on the nation’s collective health status compared to other developed countries: suffice it to say, We’re Still Not #1. But underneath that statistic is a further sad state of health affairs: that people of color in the U.S. have lower quality of
Who is perfect? Advocacy ads for real people.
What is the nature of disability? What is the nature of beauty? What is perfection? Who among us is perfect? These questions are at the heart (literally and figuratively) of a project undertaken by Pro Infirmis, a Switzerland-based advocacy organization raising awareness of people with disabilities, promoting the International Day of Persons with Disabilities in December 2013. Mannequins in fashionable shops on Zurich’s tony street the Bahnhofstrasse were replaced by new ones, artfully, painstakingly and lovingly created, as shown in the video. Pro Infirmis’s website tells us “who” we are looking at in human and 3-D life-size mannequin form: Miss Handicap 2010,
The Internet of Healthy Me – putting digital health in context for #CES2015
Men are from Mars and Women, Venus, when it comes to managing health and using digital tools and apps, based on a poll conducted by A&D Medical, who will be one of several hundred healthcare companies exhibiting at the 2015 Consumer Electronics Show this week in Las Vegas. Digital health, connected homes and cars, and the Internet of Things (IoT) will prominently feature at the 2015 Consumer Electronics Show in Las Vegas this week. I’ll be attending this mega-conference, meeting up with digital health companies and platform providers that will enable the Internet of Healthy “Me” — consumers’ ability to self-track,
Women-centered design and mobile health: heads-up, 2014 mHealth Summit
This post is written as part of the Disruptive Women on Health’s blog-fest celebrating the 2014 mHealth Summit taking place 7-11 December 2014 in greater Washington, DC. Women and mobile health: let’s unpack the intersection. On the supply side of the equation, Good Housekeeping covered health tracking-meets-fashion bling in the magazine a few weeks ago in article tucked between how to cook healthy Thanksgiving side dishes and tips on getting red wine stains out of tablecloths. This ad appeared in a major sporting goods chain’s 2014 Black Friday pre-print in my city’s newspaper last week. And along with consumer electronics brand faves like
Health info disconnect: most people view accessing online records important, but don’t perceive the need to do so
There’s a health information disconnect among U.S. adults: most people believe online access to their personal health information is important, but three-quarters of people who were offered access to their health data and didn’t do so didn’t perceive the need to. The first two graphs illustrate each of these points. When people do access their online health records, they use their information for a variety of reasons, including monitoring their health (73%), sharing their information with family or care providers (44%), or downloading the data to a mobile device or computer (39%). In this context, note that 1 in 3
NephCure – a rare disease community that’s patient-powered
The burden of chronic kidney disease (CKD) is growing, with one in 10 U.S. adults having some level of CKD. End-stage renal disease (ESRD) is the last phase of CKD, when dialysis or an organ transplant are required. Nephrotic syndrome is one of the most common forms of CKD, and focal segmental glomerulosclerosis — FSGS — is the fastest-growing cause of nephrotic syndrome in children, and the second-leading cause of kidney failure in children. I spoke with Gigi Peterkin, a longtime colleague of mine who has helped guide my own digital footprint in health. Gigi is Global Director of Marketing at
Stress Is US
“Reality is the leading cause of stress among those in touch with it,” Lily Tomlin once quipped. Perhaps in 2014, America is the land of stress because we’re all so in touch with reality. THINK: reality TV, social networks as the new confessional, news channeling 24×7, and a world of too much TMI. So no surprise, then, that one-half of the people in the U.S. have had a major stressful event or experience in the last year. And health tops the list of stressful events in This American Life in the forms of illness and disease (among 27% of people)
In pursuit of healthiness – Lancet talks US public health
It’s Independence Day week in America, and our British friends at The Lancet, the UK’s grand peer reviewed medical journal, dedicate this week’s issue to the Health of Americans – exploring life, death (mortality), health costs, chronic disease, and the Pursuit of Healthiness. This project is a joint venture between The Lancet and the U.S. Centers for Disease Control (CDC) which took 18 months to foster, called The Health of Americans Series. Americans mostly die from chronic diseases, aka non-communicable diseases, which are largely amenable to lifestyle changes like eating right, quitting smoking, drinking alcohol in moderation, and moving around more. 1 in
Affordable medicine: a preferred future
The price of medicines is a barrier for about one billion people on the planet, for citizens in developing countries as well as middle-class families in the richest country in the world, the United States. Today is World Health Day, when for 24 hours public health advocates (including me) are calling out key issues preventing people from fully living life. One obstacle for too many people is the cost of drugs and supplies that save lives and help people add life to years. For example, bug bites can be deadly if you’re talking about the 50% of the world’s population
U.S. families face medical financial burdens; health care in the SOTU
A growing proportion of American families are facing money problems related to health care, according to the report, Financial Burden of Medical Care: A Family Perspective, No. 142 in the NCHS Data Brief series from the CDC, published January 2014 and based on 2012 data. 1 in 4 families are dealing with some financial burden due to medical care. “Financial burdens” in health include problems paying medical bills in the past 12 months, shared by 16.5% of families; and medical bills being paid over time, faced by 21.4% of families. 1 in 10 families (9%) have medical bills they are
Food and money matter for health – more hospital admissions at the end of the month
If your wallets are lighter at the end of the month, you’re likely to have less access to quality food, and more likely to be admitted to the hospital if you have diabetes. The hypothesis that people with low incomes whose household budgets are spent before the end of the month have greater health inequities was tested in the article, Exhaustion of Food Budgets At Month’s End And Hospital Admissions For Hypoglycemia, published in the January 2014 issue of Health Affairs. Researchers from the University of California – San Francisco found that, indeed, the health in households with low-income suffer from
Mobile health apps – opportunity for patients and doctors to co-create the evidence
There are thousands of downloadable apps that people can use that touch on health. But among the 40,000+ mobile health apps available in iTunes, which most effectively drive health and efficient care? To answer that question, the IMS Institute for Healthcare Informatics analyzed 43,689 health, fitness and medical apps in the Apple iTunes store as of June 2013. These split into what IMS categorized as 23,682 “genuine” health care apps, and 20,007 falling into miscellaneous categories such as product-specific apps, fashion and beauty, fertility, veterinary, and apps with “gimmicks” (IMS’s word) with no obvious health benefit. Among the 23,682 so-called
7 Women and 1 Man Talking About Life, Health and Sex – Health 2.0 keeping it real
Women and binge drinking…job and financial stress…sleeplessness…caregiving challenges…sex…these were the topics covered in Health 2.0 Conference’s session aptly called “The Unmentionables.” The panel on October 1, 2013, was a rich, sobering and authentic conversation among 7 women and 1 man who kept it very real on the main stage of this mega-meeting that convenes health technology developers, marketers, health providers, insurers, investors, patient advocates, and public sector representatives (who, sadly, had to depart for Washington, DC, much earlier than intended due to the government shutdown). The Unmentionables is the brainchild of Alexandra Drane and her brilliant team at the Eliza
Chief Health Officers, Women, Are In Pain
Women are the Chief Health Officers of their families and in their communities. But stress is on the rise for women. Taking an inventory on several health risks for American women in 2013 paints a picture of pain: of overdosing, caregiver burnout, health disparities, financial stress, and over-drinking. Overdosing on opioids. Opioids are strong drugs prescribed for pain management such as hydrocodone, morphine, and oxycodone. The number of opioid prescriptions grew in the U.S. by over 300% between 1999 and 2010. Deaths from prescription painkiller overdoses among women have increased more than 400% since 1999, compared to 265% among men.
Americans’ health insurance illiteracy epidemic – simpler is better
Consumers misunderstand health insurance, according to new research published in the Journal of Health Economics this week. The study was done by a multidisciplinary, diverse team of researchers led by one of my favorite health economists, George Loewenstein from Carnegie Mellon, complemented by colleagues from Humana, University of Pennsylvania, Stanford, and Yale, among other research institutions. Most people do not understand how traditional health plans work: the kind that have been available on the market for over a decade. See the chart, which summarizes top-line findings: nearly all consumers believe they understand what maximum out-of-pocket costs are, but only one-half do.
Healthways buys into Dr. Ornish’s approach: will “Ornish-inside” scale wellness in America?
People who live in U.S. cities with low levels of well-being have twice the rate of heart attacks as people who live in healthier America. That’s 5.5% of the population in sicker America versus 2.8% of the population living in healthy America. The first chart illustrates this disparity, taken from the Gallup-Healthways index that examined 190 metropolitan areas in 2012. Based on this study, it’s good to live in parts of Utah, Nebraska and Colorado, but not so healthy to be a resident in West Virginia, Alabama, and parts of Kentucky and Ohio. Heart disease and diabetes are killing a plurality
Americans’ health not keeping up with the world: why to spend more on social determinants of health
The American health infrastructure is not First World or First Rate, based on the outcomes. This, despite spending more on health care per-person than any country on the planet. Two seminal reports are out this week reminding Americans that our return-on-investment in health spending is poor. The first research comes from JAMA titled The State of US Health, 1990-2010: Burden of Diseases, Injuries, and Risk Factors. There is some good news in this report at the top line: that life expectancy for Americans increased in the two decades from 75.2 years to 78.2 years. But this positive quantitative outcome comes with
The health and wellness gap between insured and uninsured people
If you have health insurance, chances are you take several actions to bolster your health such as take vitamins and supplements (which 2 in 3 American adults do), take medications as prescribed (done by 58% of insured people), and tried to improve your eating habits in the past two years (56%). Most people with insurance also say they exercise at least 3 times a week. Fewer people who are uninsured undertake these kinds of health behaviors: across-the-board, uninsured people tend toward healthy behaviors less than those with insurance. This is The Prevention Problem, gleaned from a survey conducted by TeleVox
A physical activity shortage: Let’s Move!
Only 1 in 5 Americans got the minimum recommended amount of physical activity in 2011, based on guidelines offered by the U.S. Centers for Disease Control. More men than women met the standard: 23.4% of men versus 17.9% of women. There are wide variations across the 50 states, as the map shows, with the healthiest folks exercise-wise living in the west, Alaska, upper midwest, and New England. The range runs from a 12.7% low in West Virginia and Tennessee to 27.3 at the high end in Colorado. That bar is set at 150 minutes a week (that’s 2.5 hours) of
Dietitians provide a health bridge between food and pharmacy
The registered dietitian is an in-demand labor resource for grocery stores around the U.S. Advertising Age covered the phenomenon of the growing clout of dietitians in food chains (April 14, 2013). Let’s dig further into this phenomenon through the Health Populi lens on healthcareDIY and peoples’ ability to bend their personal health care cost curves. Stores such as Giant Eagle, Hy-Vee, Safeway and Wegmans are morphing into wellness destinations, with pharmacies and natural food aisles taking up valuable square footage to meet consumers’ growing demands for healthy choices. Some stores are formalizing their approach to food = health by formulating a
The value of big data in health care = $450 billion
Exploiting Big Data in industry is Big News these days, and nowhere is the potential for leveraging the concept greater than in health care. McKinsey & Company estimates that harnessing big data across five dimensions of health care could yield nearly one-half trillion dollars’ worth of value in The ‘big data’ revolution in healthcare. The chart summarizes McKinsey’s calculations on the value of Big Data in health care at its maximum. Before digging into the value potential, just what is Big Data in health care? Statistics and information are generated in the health care system about patients: say, during visits
The Not-So-Affordable Care Act? Cost-squeezed Americans still confused and need to know more
While health care cost growth has slowed nationally, most Americans feel they’re going up faster than usual. 1 in 3 people believe their own health costs have gone up faster than usual, and 1 in 4 feel they’re going out about “the same amount” as usual. For only one-third, health costs feel like they’re staying even. As the second quarter of 2013 begins and the implementation of the Affordable Care Act (ACA, aka “health reform” and “Obamacare”) looms nearer, most Americans still don’t understand how the ACA will impact them. Most Americans (57%) believe the law will create a government-run health plan,
An American Nanny State? Most Americans support government tactics addressing lifestyle impacts on chronic disease
Most people like government policies targeting reducing tobacco use, requiring food manufacturers and restaurants to reduce salt content, and mandating schools to require 45 minutes of daily activity for students. A large majority of Americans (at least 8 in 10 people) support government actions to promote public health that stem chronic disease, from preventing cancer (89%) and heart disease (86%) to helping people control their diabetes (84%) and preventing childhood obesity (81%). A Survey Finds Public Support For Legal Interventions Directed At Health Behavior To Fight Noncommunicable Disease (NCD). This poll, published in the March 2013 issue of Health Affairs, profiles the





 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.