Medical Debt, Aflac on Eroding Health Benefits, the CBO’s Uninsured Forecast & Who Pays for Rising Health Care Prices: A Health Consumer Financial Update
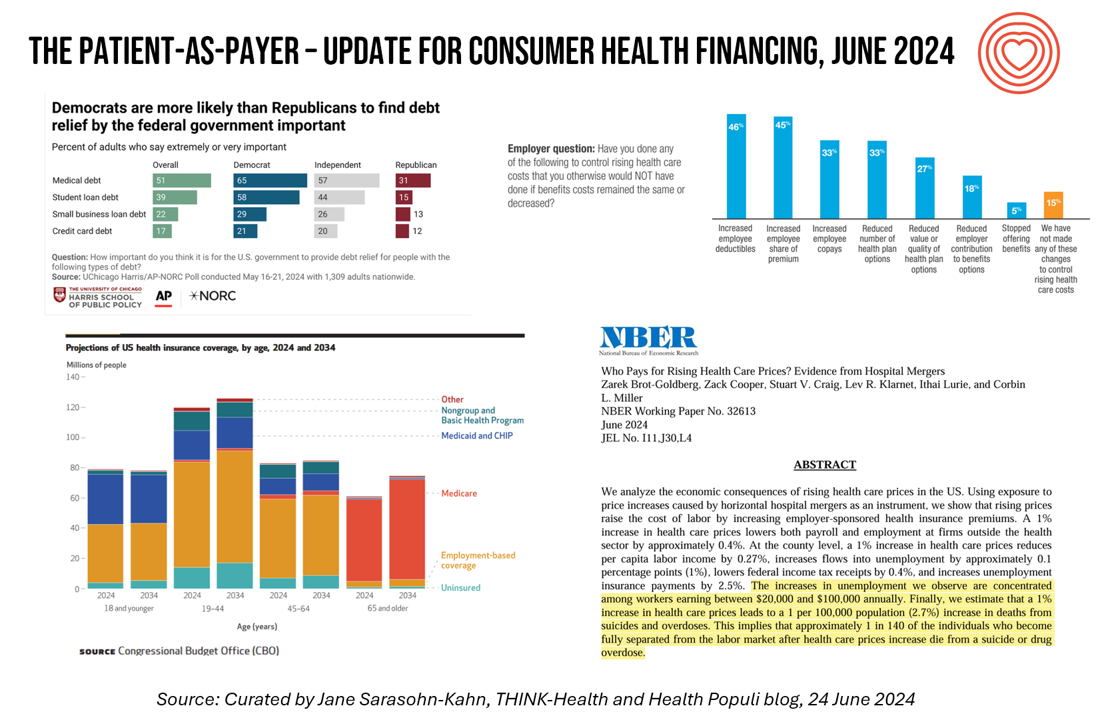
On June 11, Rohit Chopra, the Director of the Consumer Financial Protection Bureau (CFPB) announced the agency’s vision to ban Americans’ medical debt from credit reports. He called out that, “In recent years, however, medical bills became the most common collection item on credit reports. Research from the Consumer Financial Protection Bureau in 2022 showed that medical collections tradelines appeared on 43 million credit reports, and that 58 percent of bills that were in collections and on people’s credit records were medical bills.” Chopra further explained that medical debt on a consumer credit report was quite different than other kinds
A 2025 Subaru Forester, a Year at U-New Mexico, or a Health Plan for a Family of Four: the 2024 Milliman Medical Index
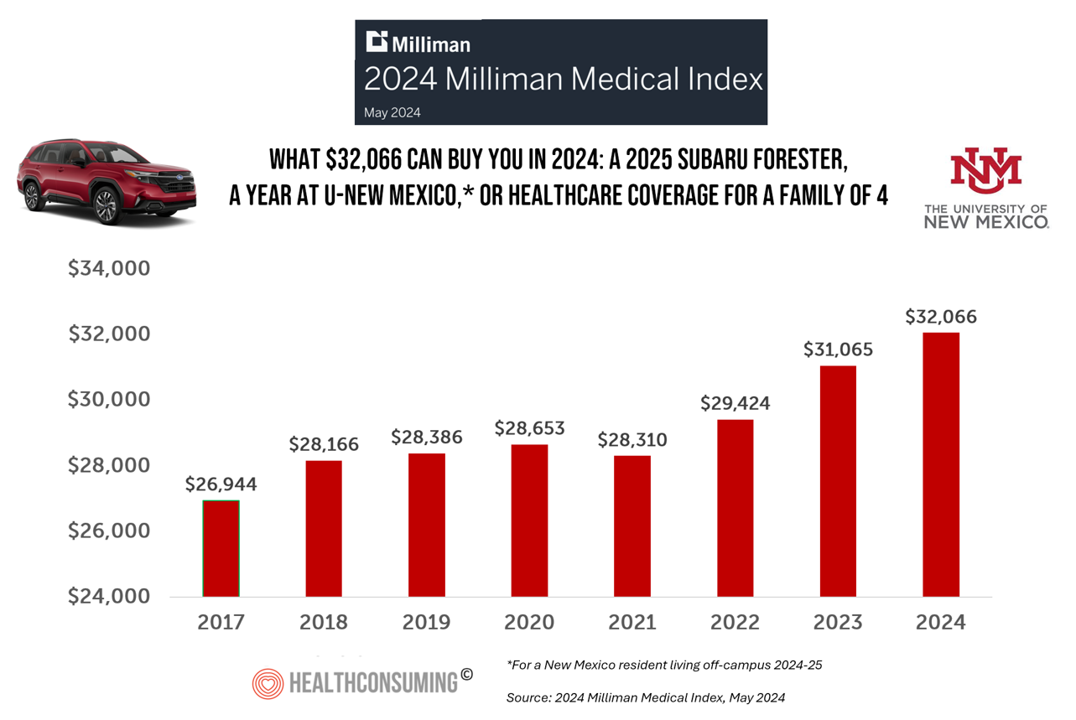
Health care costs for an “average” person covered by an employer-sponsored PPO in the U.S. rose 6.7% between 2023 and 2024, according to the 2024 Milliman Medical Index. Milliman also calculated that the largest driver of cost increase in health care, accounting for nearly one-half of medical cost increases, was pharmacy, the cost of prescription drugs, which grew 13% in the year. The big number this year is $32,066, which is the cost of that employer-sponsored PPO for a family of 4 in 2024. I’ve curated the chart of the MMI statistic for many
The Thematic Roadmap for AHIP 2024: What the Health Insurance Conference Will Cover

Health insurance plans make mainstream media news every week, whether coverage deals with the cost of a plan, the cost of out-of-network care, prior authorizations, or cybersecurity and ransomware attacks, among other front-page issues. This week, AHIP (the acronym for the industry association of America’s Health Insurance Plans) is convening in Las Vegas for its largest annual 2024 meeting. We expect at least 2,400 attendees registered for the meeting, and they’ll not just be representing the health insurance industry itself; folks will attend #AHIP2024 from other industry segments including pharmaceuticals, technology, hospitals and health systems, and the investment and financial services
Inflation, Health, and the American Consumer – “The Devil Wears Kirkland”
The Wall Street Journal reported yesterday that surging hospital prices are helping to keep inflation high. Hospital costs rose 7.7% last month, the highest increase in 13 years. This chart from WSJ’s reporting illustrates the >2x change in the CPI for hospitals vs the overall rate of price increases. Hospitals are not alone in price cliffs, with health insurance premiums spiking last year at the fastest rate in a decade, the Labor Statistics data showed. “For patients and their employers, the increases have meant higher health-insurance premiums, as well as limiting wage
Healthcare 2030: Are We Consumers, CEOs, Health Citizens, or Castaways? 4 Scenarios On the Future of Health Care and Who We Are – Part 2
This post follows up Part 1 of a two-part series I’ve prepared in advance of the AHIP 2024 conference where I’ll be brainstorming these scenarios with a panel of folks who know their stuff in technology, health care and hospital systems, retail health, and pharmacy, among other key issues. Now, let’s dive into the four alternative futures built off of our two driving forces we discussed in Part 1. The stories: 4 future health care worlds for 2030 My goal for this post and for the AHIP panel is to brainstorm what the person’s
Considering Equity and Consumer Impacts of GLP-1 Drugs – A UBS Economist Weighs In
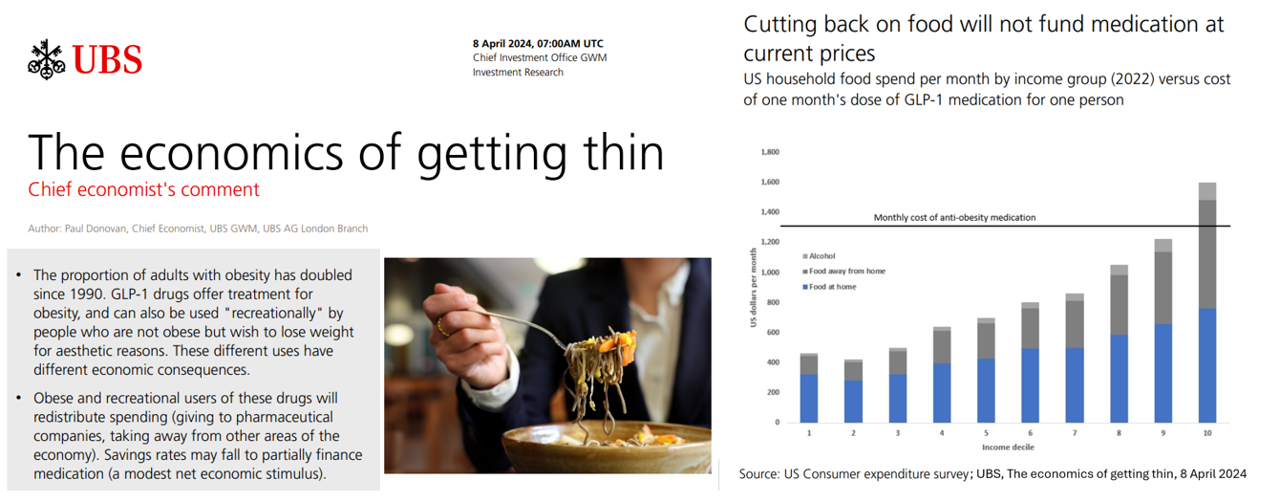
Since the introduction of GLP-1 drugs on the market, their use has split into two categories: for obesity and “recreationally,” according to the Chief Economist with UBS (formerly known as Union Bank of Switzerland). Paul Donovan, said economist, discusses The economics of getting thin in his regularly published comment blog. “These different uses have different economic consequences,” Donovan explains: Obese patients who use GLP-1s should become more productive employees, Donovan expects — less subject to prejudice, and less likely to be absent from work. While so-called recreational GLP-1 consumers may experience these
Peering Into the Hidden Lives of Patients: a Manifesto from Paytient and Nonfiction
Having health insurance in America is no guarantee of actually receiving health care. It’s a case of having health insurance as “necessary but not sufficient,” as the cost of deductibles, out-of-pocket coinsurance sharing, and delaying care paint the picture of The Hidden Lives of Workplace-Insured Americans. That’s the title of a new report that captures the results of a survey conducted in January 2024 among 1,516 employed Americans who received employer-sponsored health insurance. The study was commissioned by Paytient, a health care financial services company, engaging the research firm Nonfiction to conduct the study
The Women’s Health Gap Is Especially Wide During Her Working Years – Learning from McKinsey, the World Economic Forum, and AARP in Women’s History Month
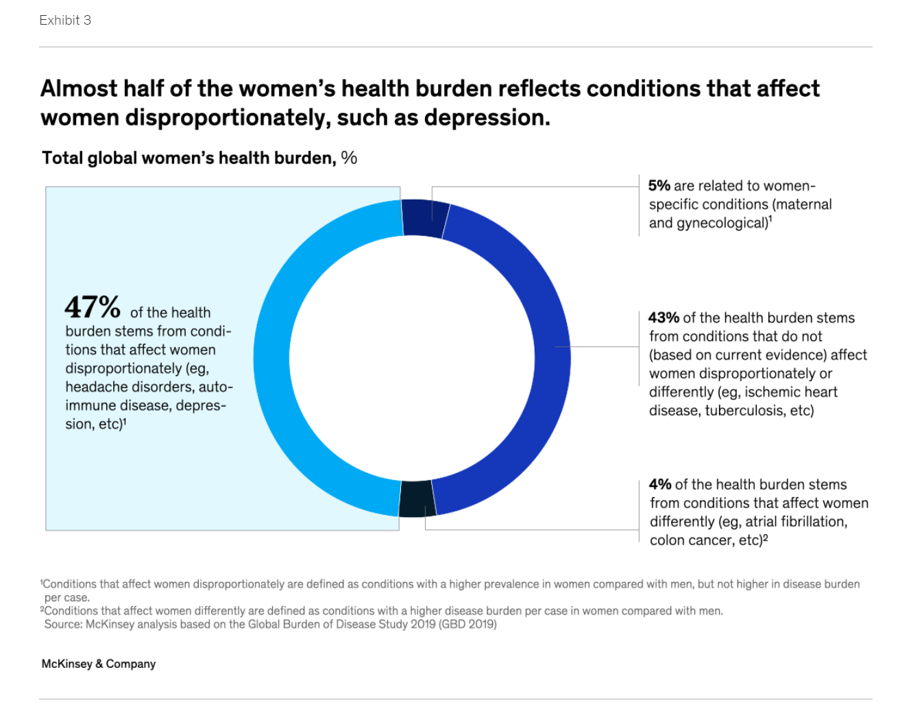
There’s a gender-health gap that hits women particularly hard when she is of working age — negatively impacting her own physical and financial health, along with that of the community and nation in which she lives. March being Women’s History Month, we’ve got a treasure-trove of reports to review — including several focusing on health. I’ll dive into two for this post, to focus in on the women’s health gap that’s especially wide during her working years. The reports cover research from the McKinsey Health Institute collaborating with the World Economic Forum on
A Health Consumer Bill of Rights: Assuring Affordability, Access, Autonomy, and Equity
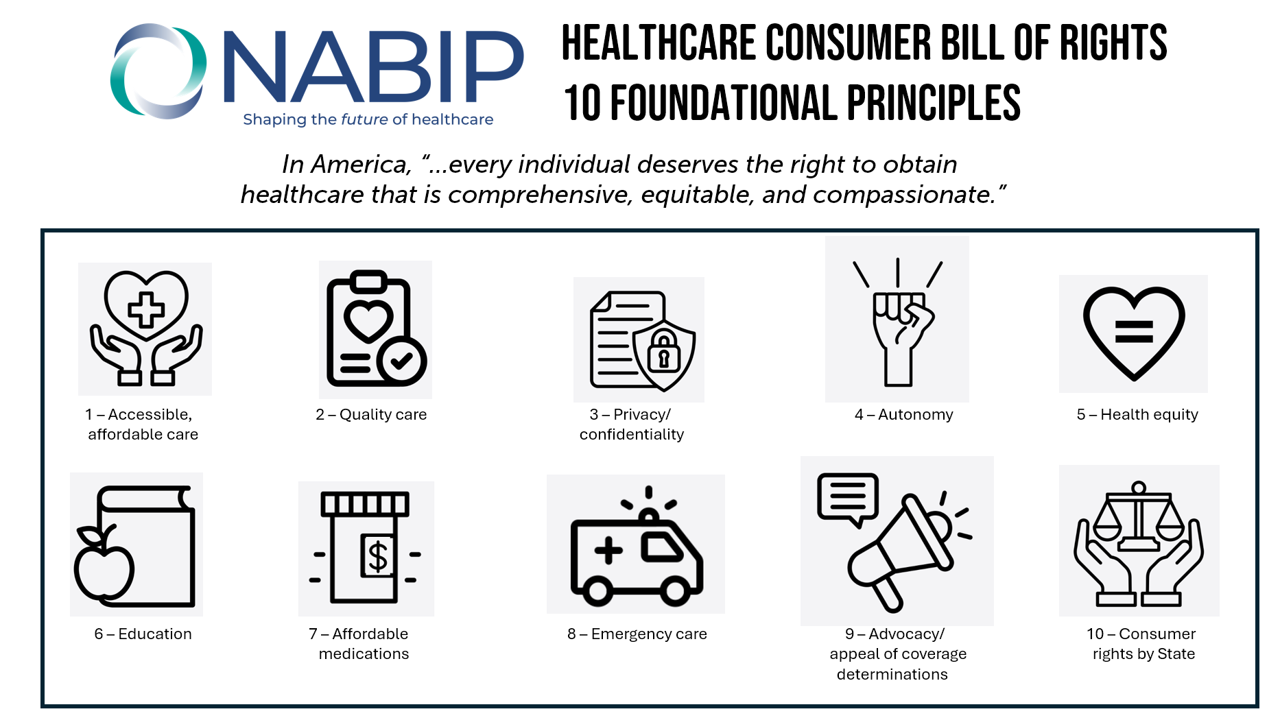
Let’s put “health” back into the U.S. health care system. That’s the mantra coming out of this week’s annual Capitol Conference convened by the National Association of Benefits and Insurance Professionals (NABIP). (FYI you might know of NABIP by its former acronym, NAHU, the National Association of Health Underwriters). NABIP, whose members represent professionals in the health insurance benefits industry, drafted and adopted a new American Healthcare Consumer Bill of Rights launched at the meeting. While the digital health stakeholder community is convening this week at VIVE in Los Angeles to share innovations in health tech, NABIP
The Trust-Innovation Gap – Welcome to the 2024 Edelman Trust Barometer
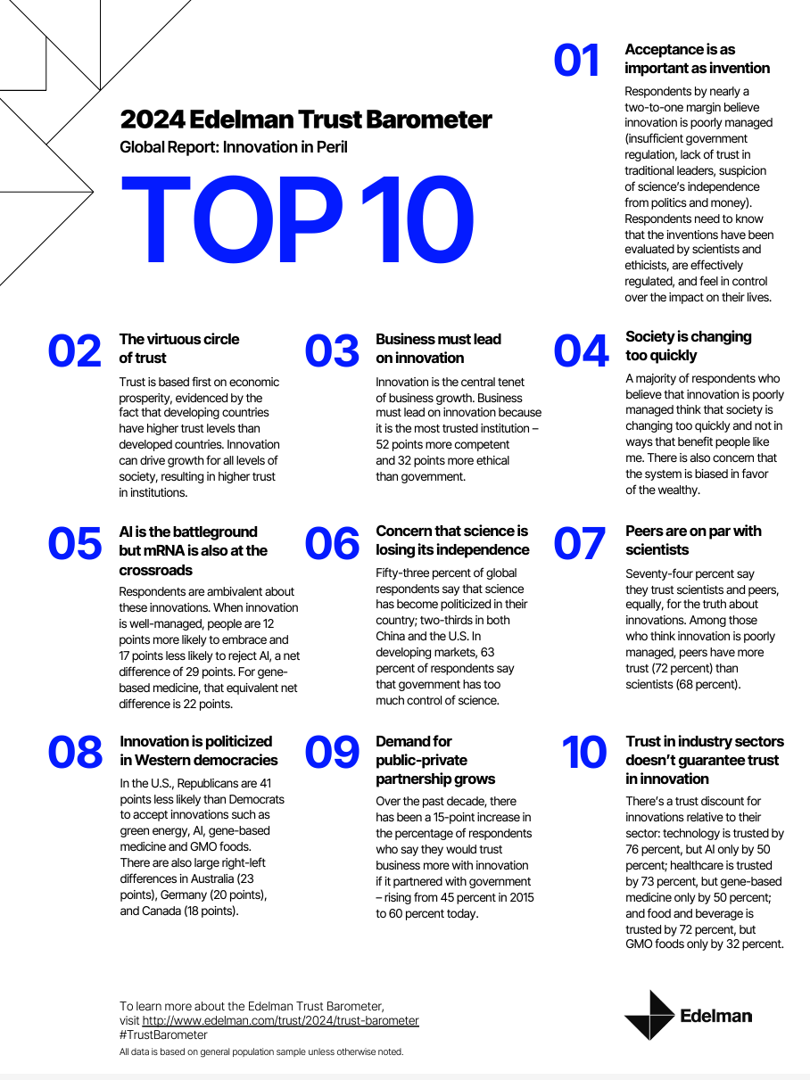
If it’s January, it’s Davos-time — that is the annual meeting of the World Economic Forum convening global experts and passionistas focused on big ideas and challenges facing us mere humans living on Planet Earth. Parallel with the WEF is the annual publication of the 2024 Edelman Trust Barometer, now in its 24th year, focusing on global citizens’ concerns that unite people around the world. For the 2024 study, Edelman’s team fielded the survey in November 2023, collecting input from over 32,000 people living in 28 countries. About 1,150 interviews (plus or minus) were done in each nation which included
In 2024 U.S. Consumers Will Mash Financial Resolutions With Those For Physical Health and Mental Health, Fidelity Finds
One-third of U.S. consumers feel in worse financial shape now than in 2022, with inflation a top concern, discovered in the 2024 New Year’s Financial Resolutions Study from Fidelity Investments. In this 15th annual update of Fidelity’s research into Americans’ New Year’s resolutions for financial health, we learn the mantra that 2024 will be the year of living practically, opening new chapters for saving and paying down debt. Fidelity conducted an online poll among 3,002 U.S. adults 18 and over in October 2023 to gauge peoples’ perspectives on personal finances, and well-being currently and into 2024. This
Money and Mental Health in the U.S. – How Difficulty Paying Medical Bills Can Hurt Healing and Well-Being
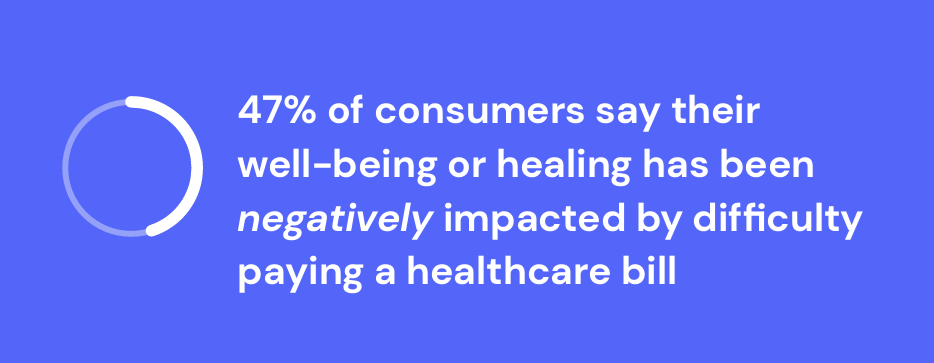
There is growing evidence on the connection between people’s financial health and their mental health, explored and explained in Understanding the Mental-Financial Health Connection, a study published by the Financial Health Network. Keep that relationship in mind in the context of a new forecast from Kaiser Family Foundation estimate the 2023 cost for employer-sponsored insurance for a family to reach nearly $24,000 in 2023. That cost is a 7% increase over last year, and is expected to be split with companies covering $17K (about 70%) and employees about $6600 (roughly 30%). KFF heard that
Working in America: AI Is the Next Major Job Stressor
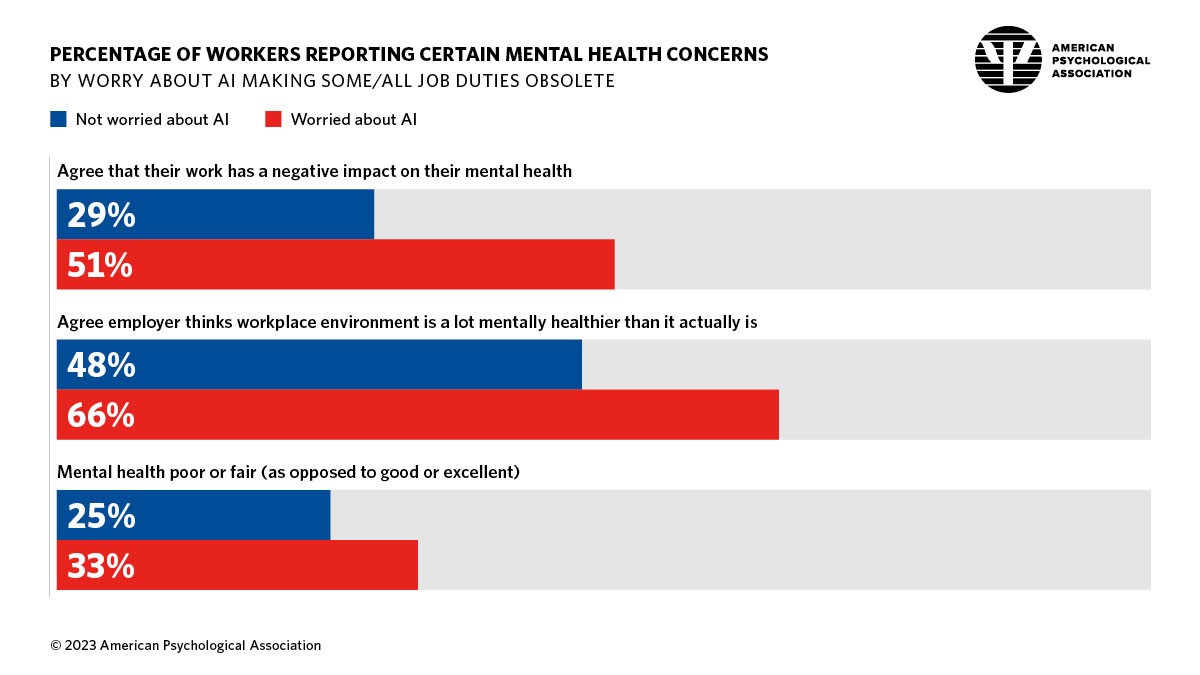
Workers in America are worried about the potential impacts that artificial intelligence (AI) could have on the workplace and jobs, according to Work in America: Artificial Intelligence, Monitoring Technology and Psychological Well-Being, a study from the American Psychological Association (APA). For many years, we’ve been tracking APA’s Stress in America studies gauging Americans’ mental health before the pandemic and during the pandemic. To social and political stress, we must now add in another stressor to peoples’ daily lives: concerns about AI and the potential for it to make one’s job obsolete, with the subsequent
Large Employers Expect More Employees Will Experience Prolonged Health Impacts Due to COVID-19. and a Note About Telehealth Engagement
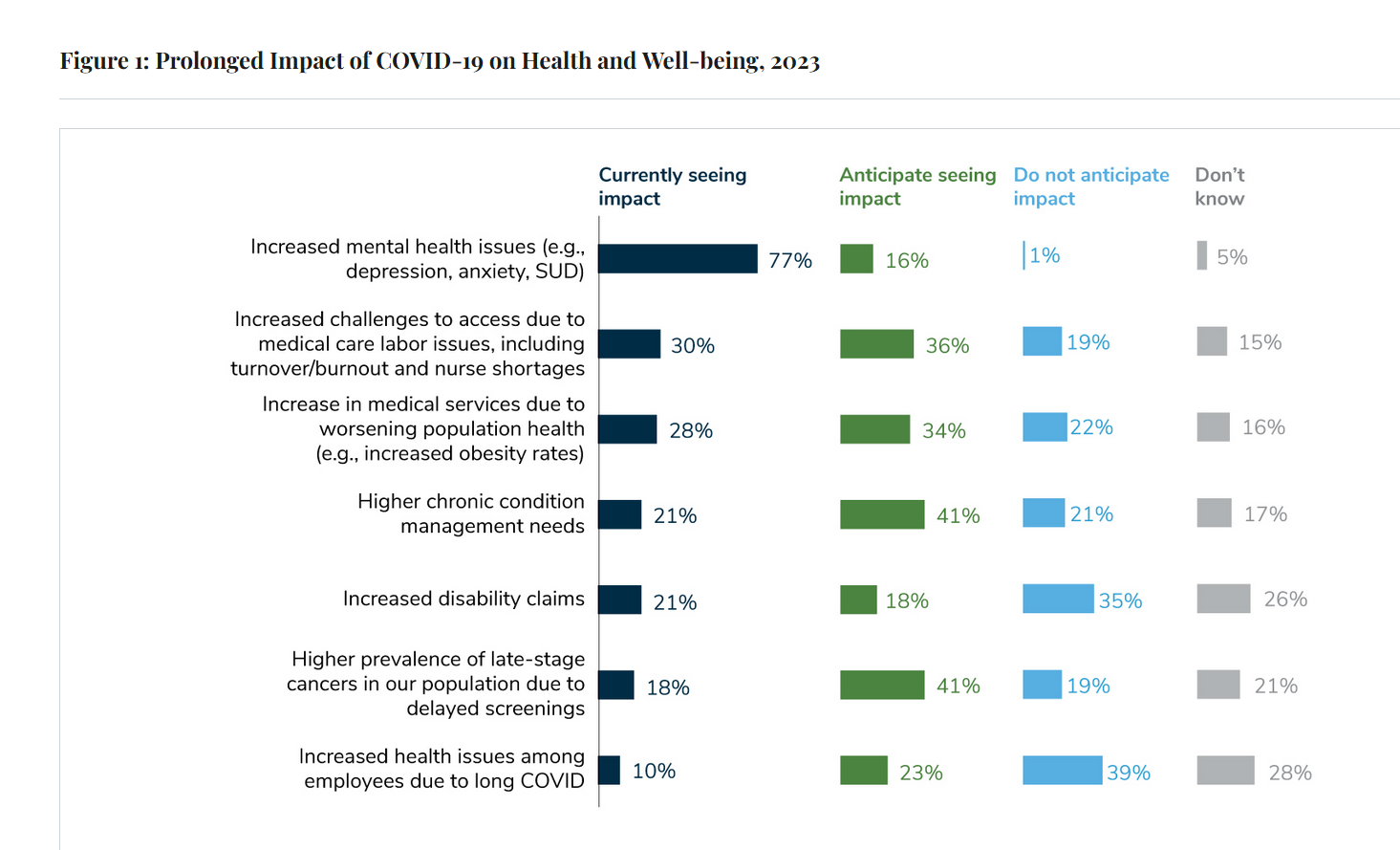
Due to their delayed return to medical services and diagnostic testing in the COVID-19 pandemic era, U.S. employees are expected to sustain serious health impacts that will drive employers’ health care costs, envisioned in the 2024 Large Employer Health Care Strategy Survey from the Business Group on Health (BGH). Dealing with mental health issues is the top health and well-being impact workers in large companies are addressing in 2023. Looking forward, large employers foresee their workers will be seeking care for chronic conditions and later-stage cancers that are diagnosed due to delayed screenings.
Hims and Hers and Hearts – Cardiology Blurs Into DTC Retail Health
Statin therapy has been used for decades to lower cholesterol with the goal of reducing mortality and preventing cardiovascular problems such as heart attacks and strokes. Hims & Hers announced a new service offering for health consumers and clinicians concerned about heart health called Heart Health by Hims. This is Hims & Hers’ first foray into cardiovascular health, working in collaboration with the American College of Cardiology (ACC). ACC clinical guidelines will inform the Hims’ provider platform for the program. “Prevention is the ideal mechanism to decrease cardiovascular events and ensure optimal heart
What $31,065 Can Buy You: a Toyota Corolla Cross Hybrid, a Year at Gnomon School, or Healthcare for a Family of 4 in America
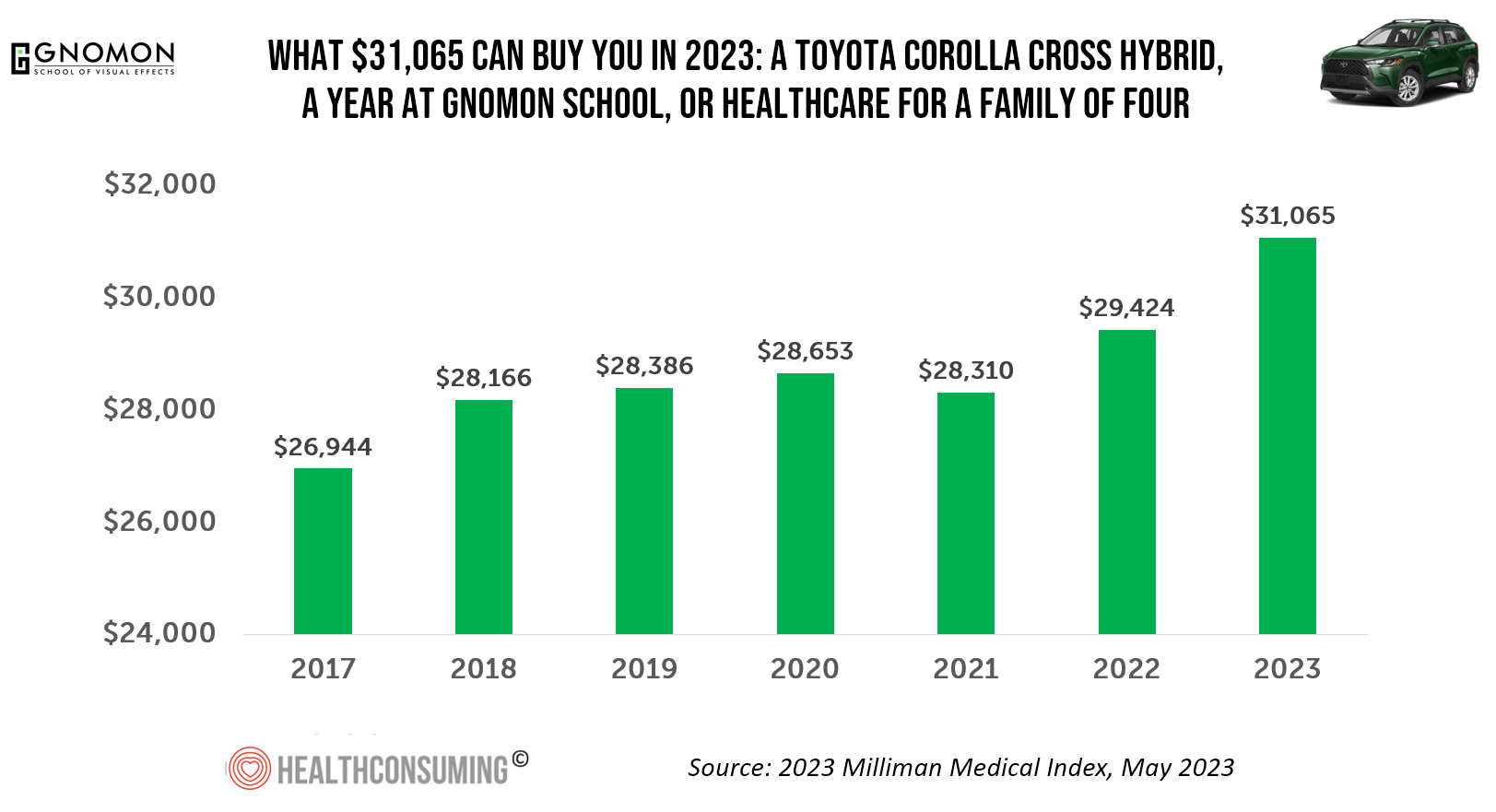
“Healthcare costs came roaring back in 2021” after falling in 2020. In 2023, that roaring growth in health care costs continues with expected growth of 5.6%. For 2023, you could take your $31K+ and buy a Toyota Corolla Cross Hybrid auto, fund a year at the Gnomon School in Hollywood toward a degree in animation or game design, or buy healthcare for your family of 4. Welcome to this year’s annual look at health care costs for a “typical” U.S. family explained in the 2023 Milliman Medical Index (MMI).
Getting Health Care at a Retail Pharmacy vs a Retail Store: Consumers May Be Favoring the Pharmacist Versus the Retailer
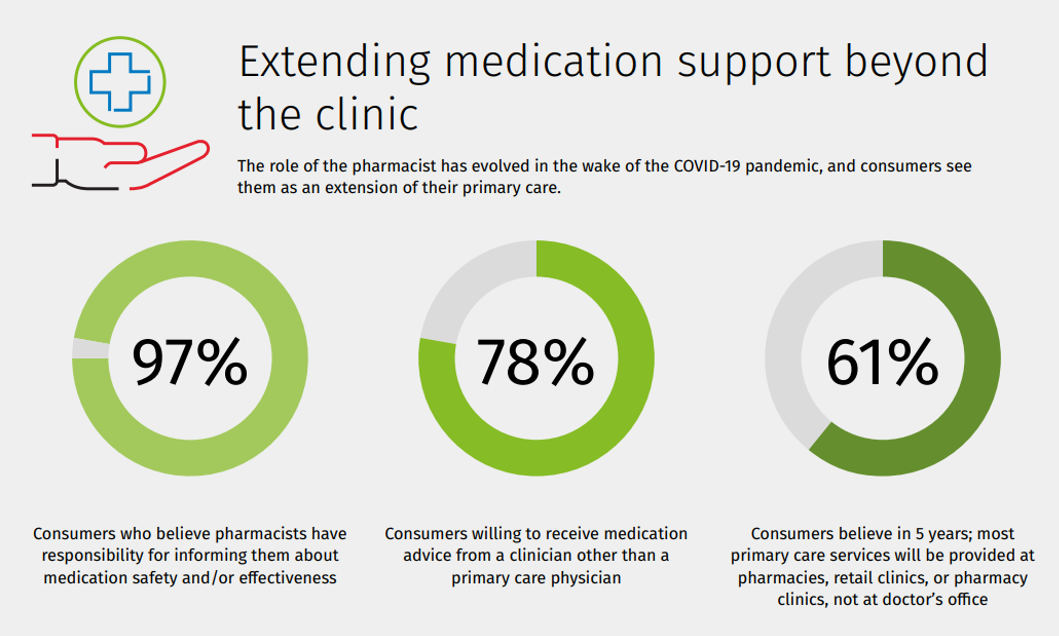
Not all “retail health” sites are created equal, U.S. consumers seem to be saying in a new study from Wolters Kluwer Health, the company’s second Pharmacy Next: Consumer Care and Cost Trends survey. Specifically, consumers have begun to differentiate between health care delivered at a retail pharmacy versus care offered at a retail store — such as Target or Walmart (both named as sites that offer “health clinics in department stores” in the study press release). While 58% of Americans were likely to visit a local pharmacy as a “first step” when faced with a non-emergency medical situation and 79%
The ROI on Feeling Cared-For At Work – Employer Trust, Love, and Building the Joyconomy
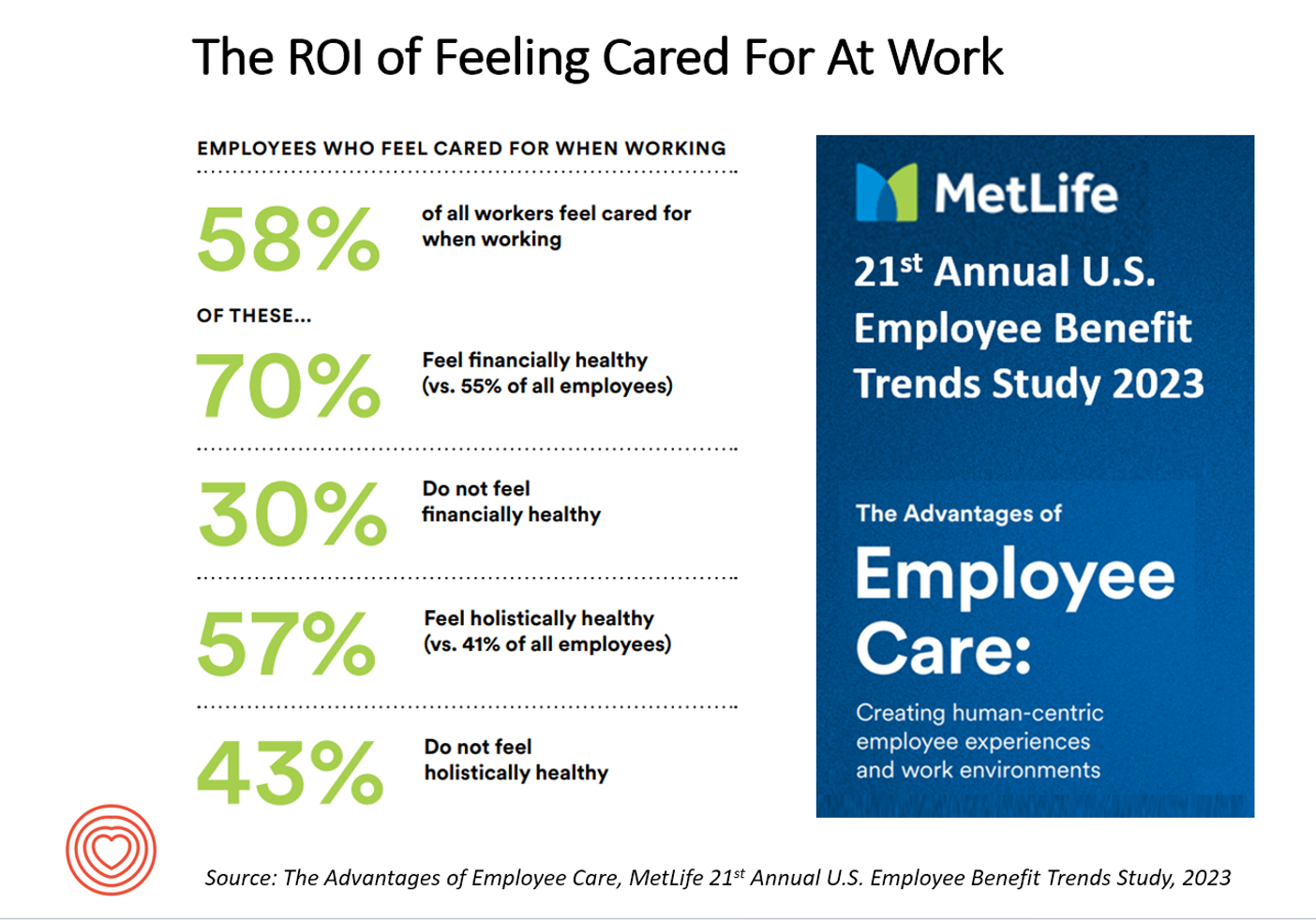
“Can employers afford not to care?” MetLife’s 21st annual U.S. Employee Benefit Trends Study asks and answers that question, with a resounding and evidence-based “NO.” I’m in Salt Lake City today discussing the drivers of health, “yesterday, today, and tomorrow” at the Virgin Pulse Thrive Summit, celebrating the ten-year anniversary of the company. As you would expect from an organization that is part of Richard Branson’s business ecosystem, the meeting will be energetically produced, delivering insights wrapped in info-taining ways. One of those features will be my being invited to create a
People Using Health Apps and Wearable Tech Most Likely Track Exercise and Heart Rate, Sleep and Weight – But Cost Is Still A Barrier
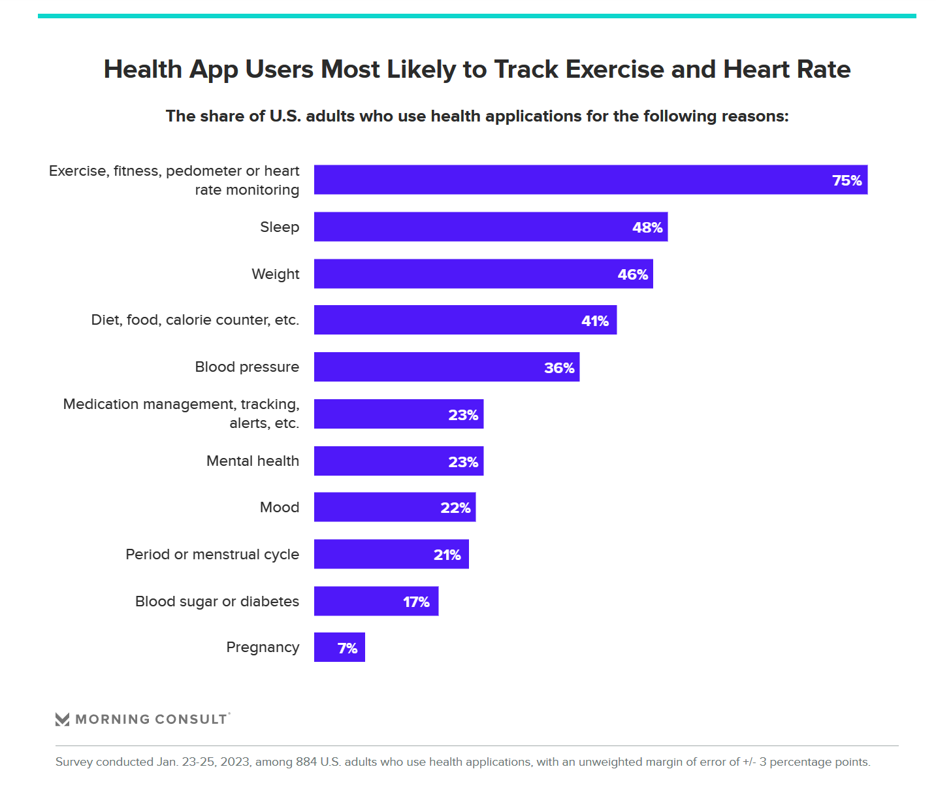
Over one in three U.S. consumers use a health app or wearable technology device to track some aspect of their health. “The public’s use of health apps and wearables has increased in recent years but digital health still has room to grow,” a new poll from Morning Consult asserts, published today. Among digital health tech users, most check into them at least once every day in the past month. One in four use these tech’s multiple times a day, the first pie chart illustrates. Eighteen percent of people use their digital
Wellness in 2023 Is About Connections, Mental Health and Science – Global Wellness Summit’s 2023 Trends

Consumers’ wellness life-flows and demands in 2023 will go well beyond exercise resolutions, eating more greens, and intermittent fasting as a foodstyle. It’s time for us to get the annual update on health consumers from the multi-faceted team who curated the Global Wellness Summit’s annual report on The Future of Wellness 2023 Trends. In this year’s look into wellness for the next few years, we see that health-oriented consumers are seeking solutions for dealing with loneliness and mental health, weight and hydration, travel-as-medicine as health destinations, and — not surprisingly —
When Household Economics Blur with Health, Technology and Trust – Health Populi’s 2023 TrendCast
People are sick of being sick, the New York Times tells us. “Which virus is it?” the title of the article updating the winter 2022-23 sick-season asked. Entering 2023, U.S. health citizens face physical, financial, and mental health challenges of a syndemic, inflation, and stress – all of which will shape peoples’ demand side for health care and digital technology, and a supply side of providers challenged by tech-enabled organizations with design and data chops. Start with pandemic ennui The universal state of well-being among us mere humans is pandemic ennui: call it languishing (as opposed to flourishing), burnout, or
Thinking Value-Based Health Care at HLTH 2022 – A Call-to-Action
The cost of health insurance for a worker who buys into a health plan at work in 2022 reached $22,463 for their family. The average monthly mortgage payment was $1,759 in mid-2022. “When housing and health both rank as basic needs in Maslow’s hierarchy, what’s a health system to do?” I ask in an essay published today on Crossover Health’s website titled Value-Based Care: Driving a Social Contract of Trust and Health. The answer: embrace value-based care. Warren Buffett wrote Berkshire Hathaway shareholders in 2008, asserting that, “Price is what you pay. Value
$22,463 Can Get You a Year of College in Connecticut, a Round of Ref Work in the Stanley Cup Playoffs, or Health Benefits for a Worker’s Family
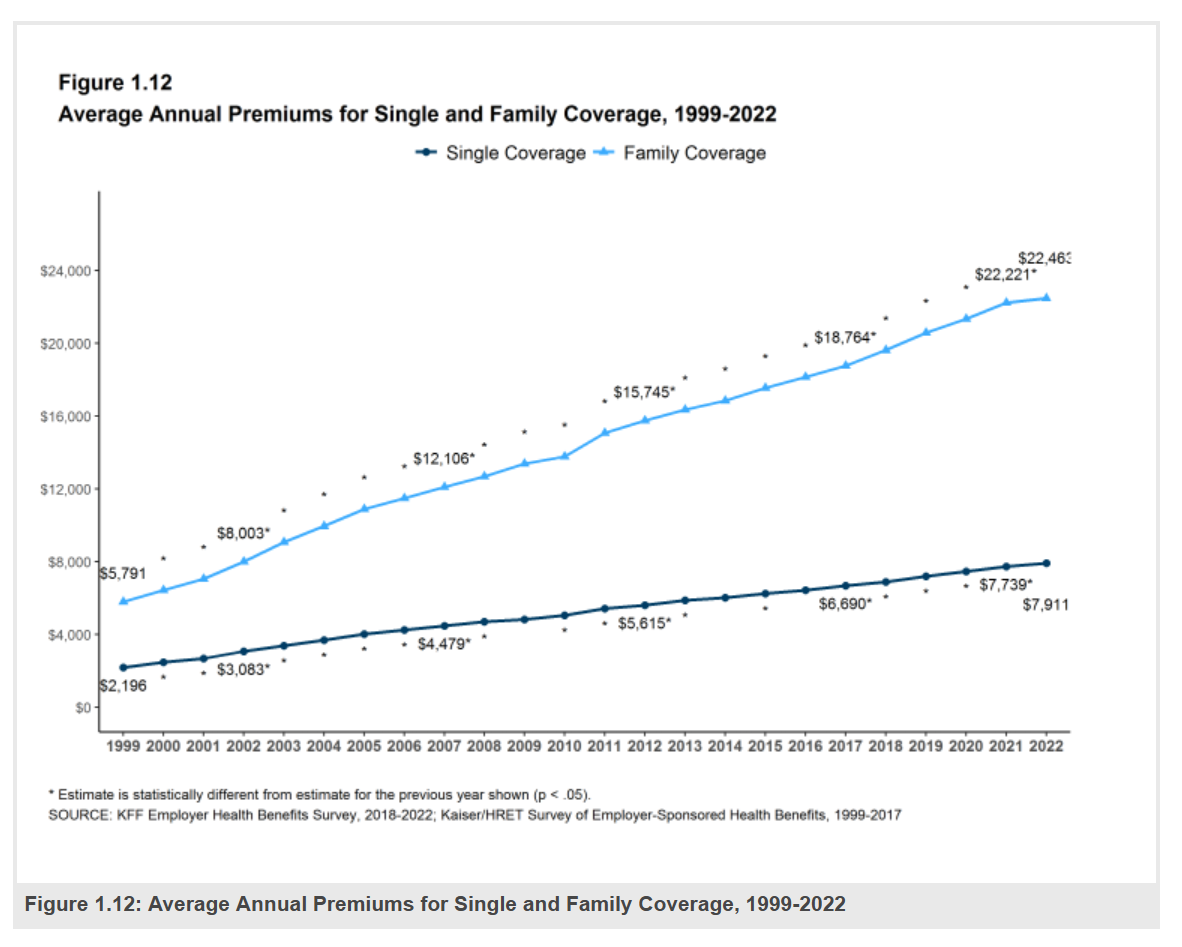
Employers covering health insurance for workers’ families will face insurance premiums reaching, on average, $22,463. That is roughly what a year at an independent college in Connecticut would cost, or a round of pay for a ref in the Stanley Cup playoffs. With that sticker-shock level of health plan costs, welcome to the 2022 Employer Health Benefits Survey from Kaiser Family Foundation, KFF’s annual study of employer-sponsored health care. Each year, KFF assembles data we use all year long for strategic and tactical planning in U.S. health care. This mega-study looks at
Virtual Care and Mental Health Top of Mind for Employers’ Workplaces in 2023
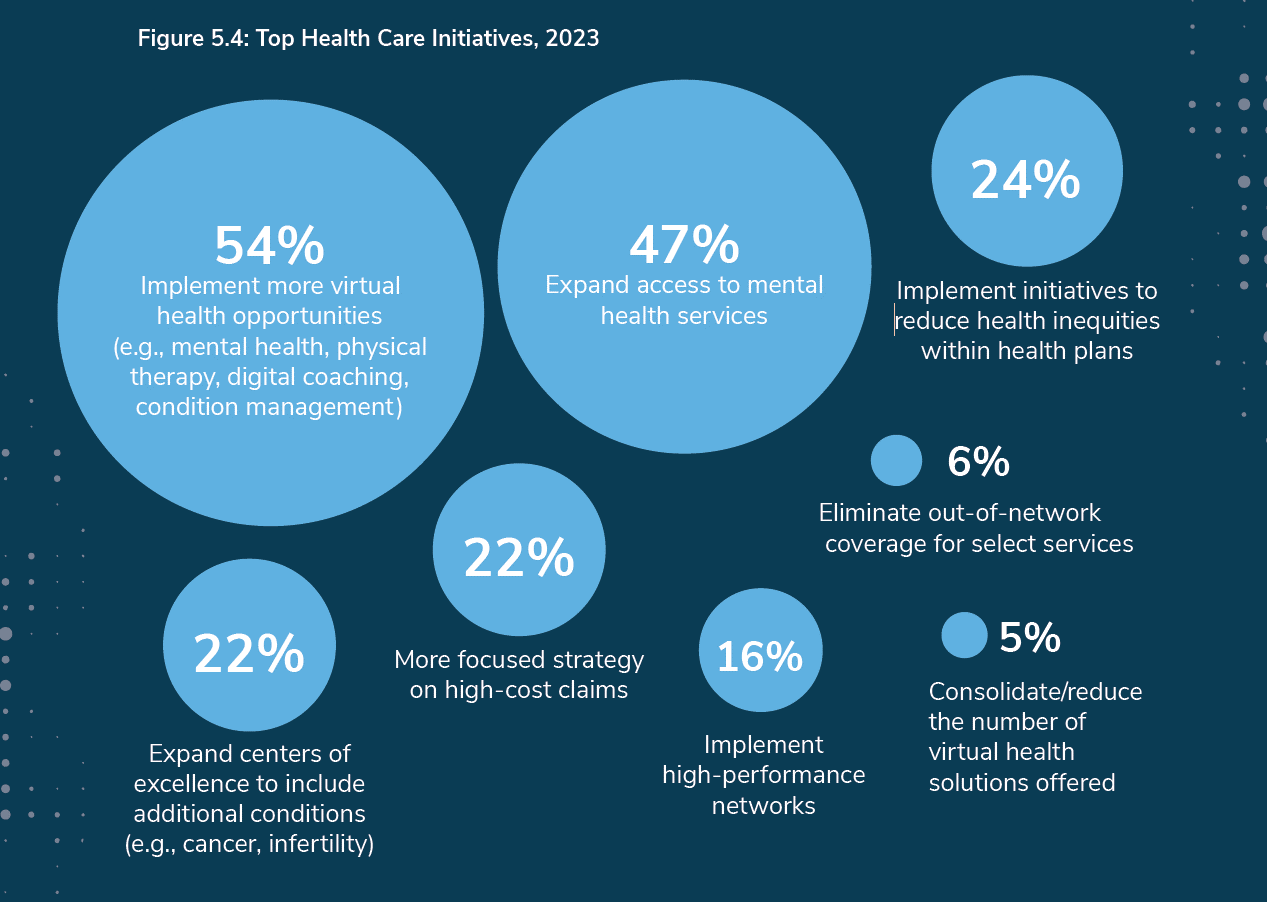
The concept that all companies are “health care companies” takes on greater import in the wake of the pandemic. The 2023 Large Employers’ Health Care Strategy and Plan Design Survey from the Business Group on Health (BGH) found that two in three large employers see their health and well-being strategy as an integral part of their overall workforce strategy. This is our annual go-to study guiding us on the private sector’s big thinking about health care plans and investments on workers’ behalf. The first line chart illustrates how this phenomenon shot up in importance for
The More Chronic Conditions, the More Likely a Patient Will Have Medical Debt
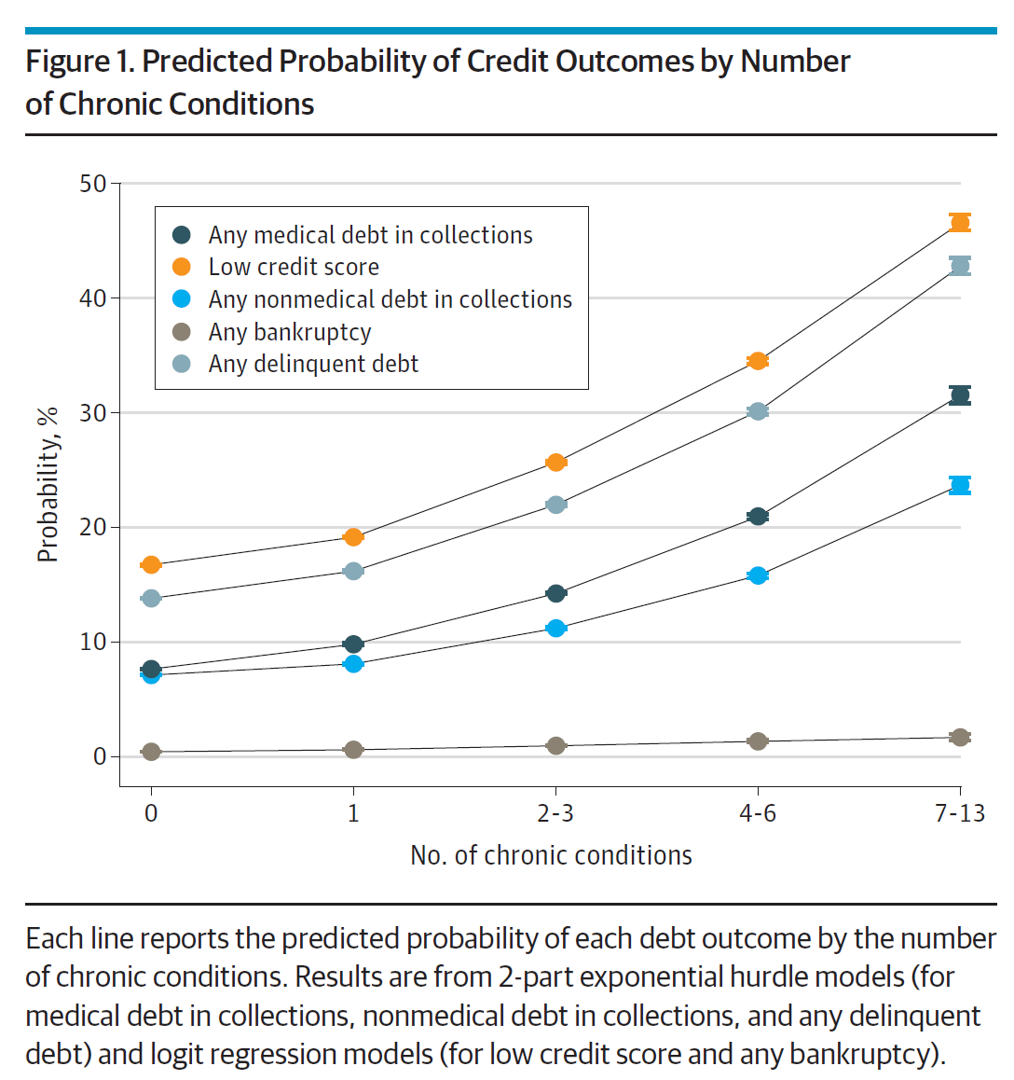
There is a direct association between a person’s health status and patient outcomes and their financial health, quantified in original research published this week in JAMA Internal Medicine. Researchers from the University of Michigan (my alma mater) Medical School and Institute for Healthcare Policy and Innovation analyzed two years of commercial insurance claims data generated between January 2019 and January 2021, linking to commercial credit data from January 2021 for patients enrolled in a preferred providers organization in Michigan. The first chart illustrates the predicted probability of credit outcomes based on the
The Retail Health Battle Royale in the U.S. – A Week-Long Brainstorm, Day 2 of 5 – Amazon and One Medical

Today we review the various viewpoints on Amazon’s announced acquisition of One Medical (ONEM, aka 1life Healthcare) which has been a huge story in both health care trade publications, business news, and mainstream media outlets. Welcome to Day 2 of The Retail Health Battle Royale in the U.S., my week-long update of the American retail health/care ecosystem weaving the latest updates from the market and implications and import for health care consumers. The deal was announced on 21 July, with Amazon striking the price at about $3.9 billion. Goldman Sachs and Morgan Stanley put the deal together,
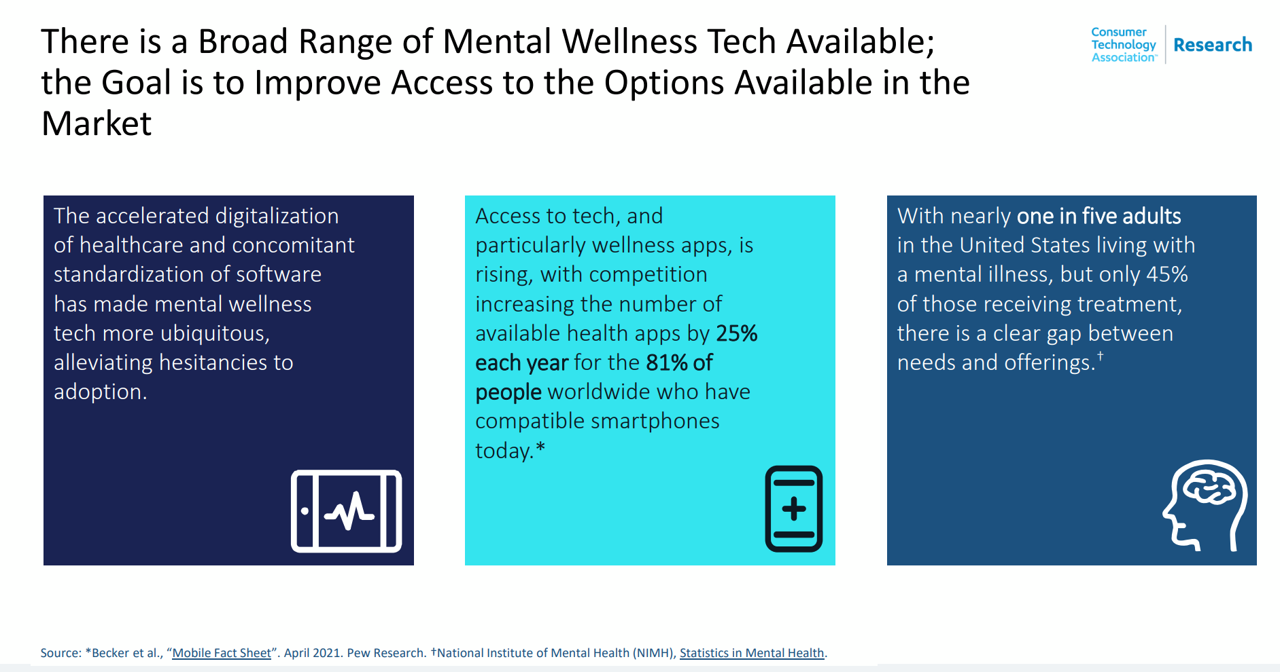
In A Declining Consumer Tech Spending Forecast, Consumer Health Tech Will Grow in 2022: Reading the CTA Tea Leaves
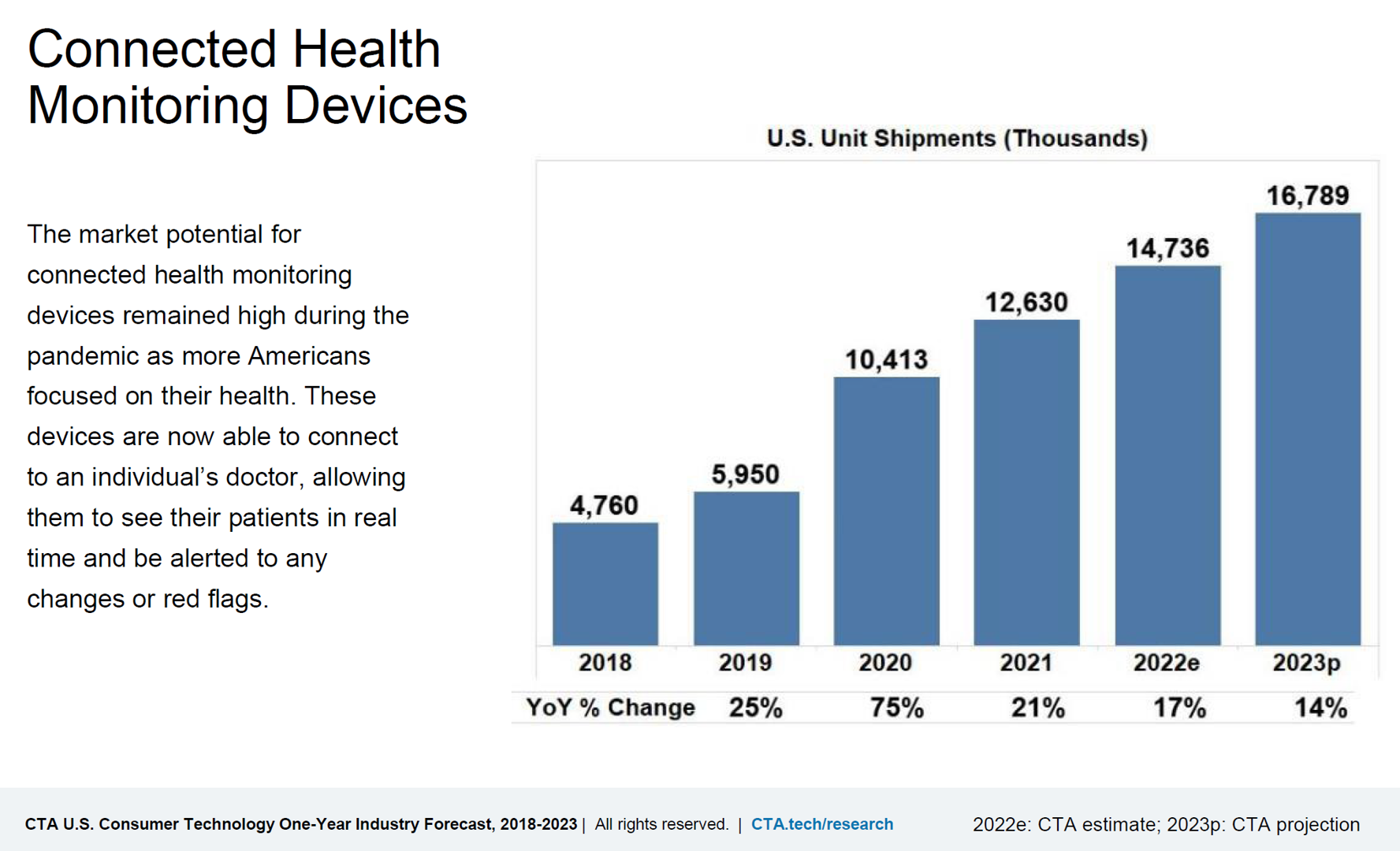
Supply chain challenges, inflation, and plummeting consumer economic sentiment are setting the stage for a decline in consumer electronics revenues for 2022. However, there will be some bright spots of growth for consumer tech spending, for 5G smartphones, smart home applications, gaming, and health technologies, noted in the Consumer Technology Association’s CTA U.S. Consumer Technology One-Year Industry Forecast, 2018-2023. Underneath the overall industry spend of $503 billion, a 0.2% drop from 2021, CTA expects software, gaming, video and audio streaming spending will grow by 3.5% and hardware to fall by 1.4% this year. With
Consumers’ Dilemma: Health and Wealth, Smartwatches and Transparency

Even as spending on healthcare per person in the United States is twice as much as other wealthy countries in the world, Americans’ health status ranks rock bottom versus those other rich nations. The U.S. health system continues to be marred by health inequalities and access challenges for man health citizens. Furthermore, American workers’ rank top in the world for feeling burnout from and overworked on the job. Welcome to The Consumer Dilemma: Health and Wellness,, a report from GWI based on the firm’s ongoing consumer research on peoples’ perspectives in the wake of
Changing Views of Retirement and Health Post-COVID: Transamerica’s Look At Workers’ Disrupted Futures
As more than 1 in 3 U.S. workers were unemployed during the pandemic and another 38% had reductions in hours and pay, Americans’ personal forecasts and expectations for retirement have been disrupted and dislocated. In its look at The Road Ahead: Addressing Pandemic-Related Setbacks and Strengthening the U.S. Retirement System from the Tramsamerica Center for Retirement Studies (TCRS), we learn about the changing views of U.S. workers on their future work, income, savings, dreams and fears. Since 1988, TCRS has assessed workers’ perspectives on their futures, this year segmented the 10,003 adults
Use of Preventive Health Services Declined Among Commercially Insured People – With Big Differences in Telehealth for Non-White People, Castlight Finds
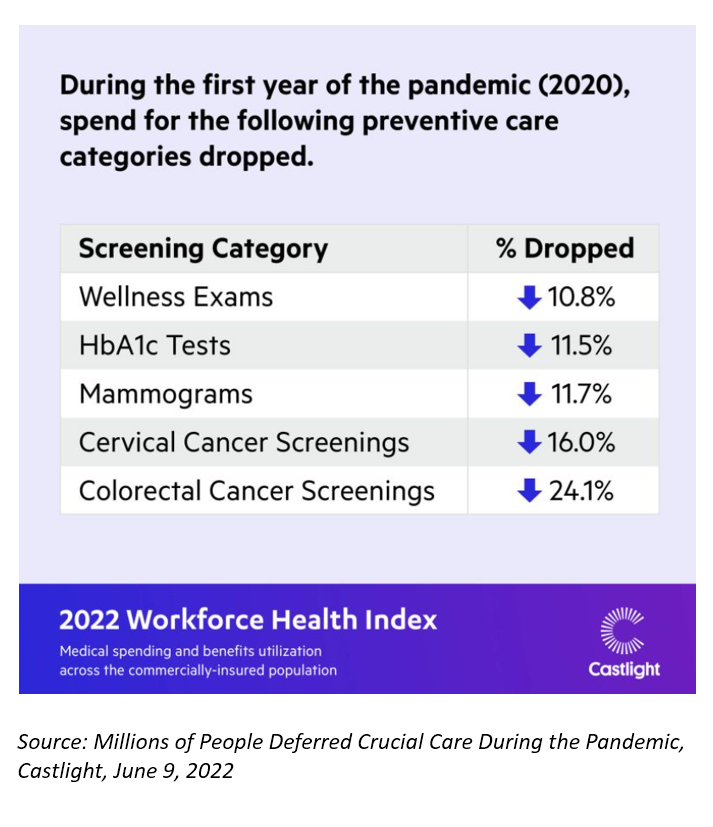
Declines in preventive care services like cancer screenings and blood glucose testing concern employers, whose continued to cover health insurance for employees during the pandemic. “As we enter the third year of the COVID-19 pandemic, employers continue to battle escalating clinical issues, including delayed care for chronic conditions, postponed preventive screenings, and the exponential increase in demand for behavioral health services,” the Chief Medical Officer for Castlight Health notes in an analysis of medical claims titled Millions of People Deferred Crucial Care During the Pandemic, published in June. The
A New Chevy Equinox SUV, a Year in Grad School, or Health Care for Four – The 2022 Milliman Medical Index
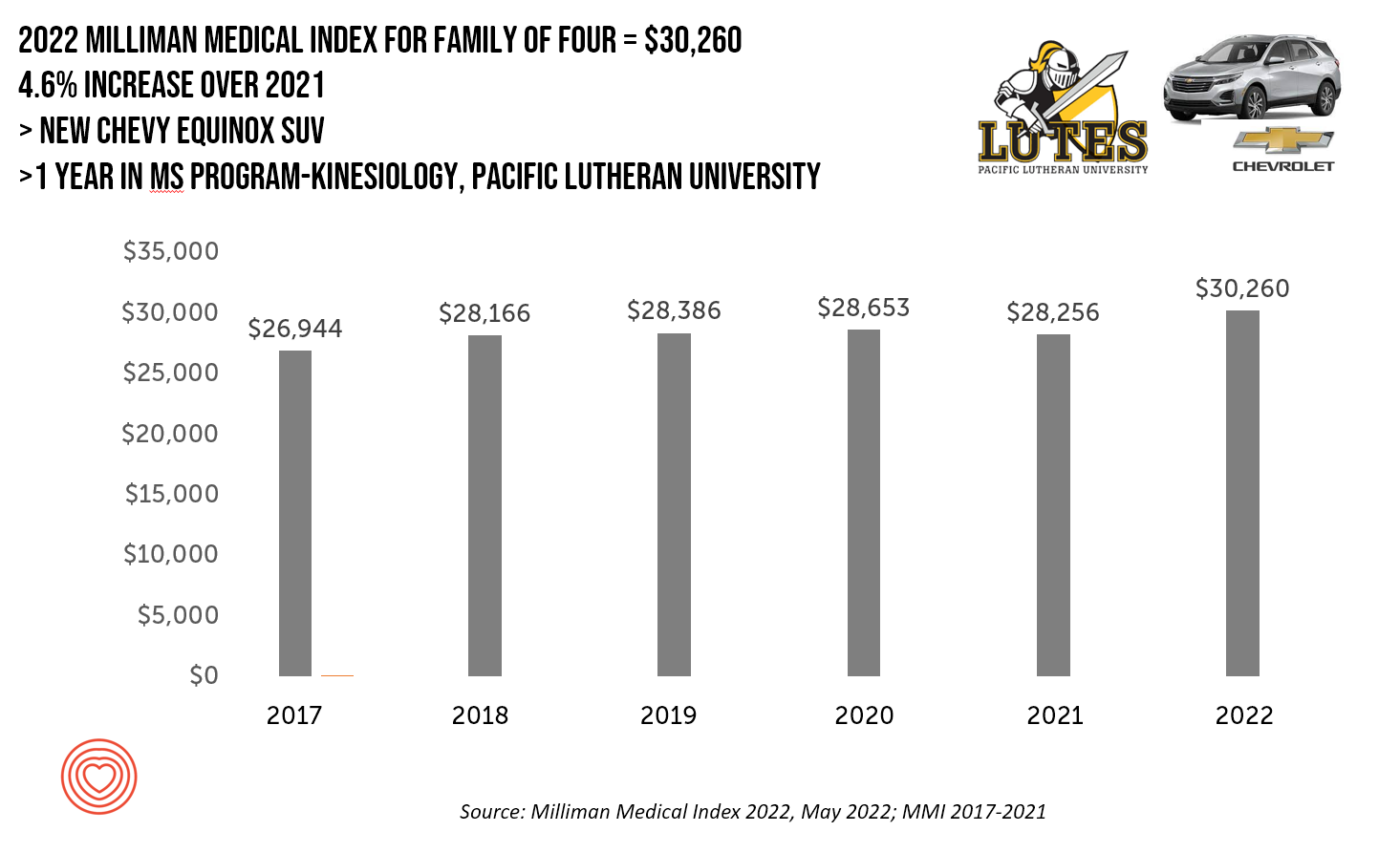
A new Chevy Equinox SUV, a year in an MS program in kinesiology at Pacific Lutheran U., or health care for a family of four. At $30,260, you could pick one of these three options. Welcome to this year’s 2022 Milliman Medical Index, which annually calculates the health care costs for a median family of 4 in the U.S. I perennially select two alternative purchases for you to consider aligning with the MMI medical index. I have often picked a new car at list price and a year’s tuition at a U.S. institution of
How Business Can Bolster Determinants of Health: The Marmot Review for Industry
“Until now, focus on….the social determinants of health has been for government and civil society. The private sector has not been involved in the discussion or, worse, has been seen as part of the problem. It is time this changed,” asserts the report, The Business of Health Equity: The Marmot Review for Industry, sponsored by Legal & General in collaboration with University College London (UCL) Institute of Health Equity, led by Sir Michael Marmot. Sir Michael has been researching and writing about social determinants of health and health equity for decades, culminating publications
McKinsey’s Six Shifts To Add Life to Years — and One More to Consider
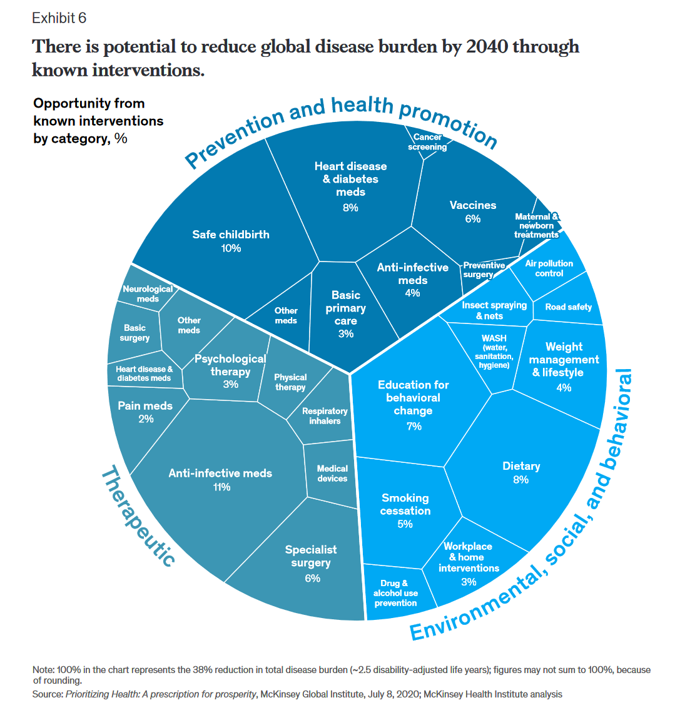
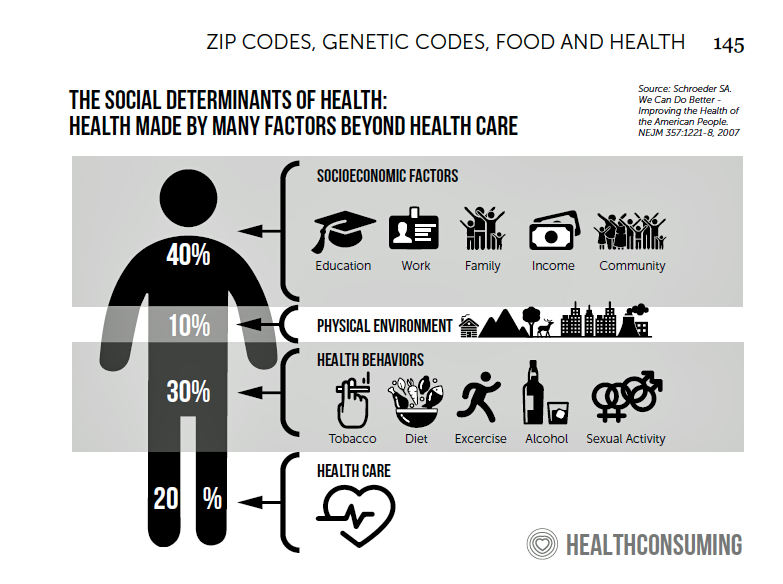
People spend one-half of their lives in “less-than-good health,” we learn early in the paper, Adding years to life and life to years from the McKinsey Health Institute. In this data-rich essay, the McKinsey team at MHI sets out an agenda that could help us add 45 billion extra years of higher-quality life equal to an average of six years per person (depending on your country and population demographics). The first graphic from the report illustrates four dimensions of health and the factors underneath each of them that can bolster or diminish our well-being: personal behaviors (such as sleep and diet),
Go Local and Go Beyond Medical Care: What Hospitals, Health Plans, and Pharma Can Do to Rebuild Trust

Without trust, people do not engage with health care providers, health plans, or life science companies….nor do many people accept “science fact.” I explore the sad state of Trust and Health Care. published in the Medecision Liberate Health blog, with a positive and constructive call-to-action for health care industry stakeholders to consider in re-building this basic driver of well-being. That is, trust as a determinant of health. Edelman’s 2022 Trust Barometer came out in January 2022, coinciding as it annually does with the World Economic Forum’s meeting in Davos, Switzerland. Every year, WEF convenes the world’s biggest thinkers to wrestle with the
The Trust Deficit Is Bad for Health: A Health/Care Lens on the 2022 Edelman Trust Barometer
“Health is the cornerstone to our core needs, thereby the cornerstone to trust.” So wrote Kirsty Graham, Global Leader of Sectors and Global Chair of Health at Edelman, in an essay explaining the 2022 Edelman Trust Barometer. If it’s January, it must be time for the World Economic Forum in Davos, the annual setting for Edelman’s launch of the company’s Trust Barometer. While WEF is mostly virtual this year due to the pandemic, Edelman has released the survey of global citizens’ views on trust in institutions right on-time and in full and sobering detail. I welcome and dig into the
Mental Health at CES 2022 – The Consumer’s Context for Wellbeing in the New Year
As we enter COVID-19’s “junior year,” one unifying experience shared by most humans are feelings of pandemic fatigue: anxiety, grief, burnout, which together diminish our mental health. There are many signposts pointing to the various flavors of mental and behavioral health challenges, from younger peoples’ greater risk of depression and suicide ideation to increased deaths of despair due to overdose among middle-aged people. And about one-in-three Americans has made a 2022 New Year’s resolution involving some aspect of mental health, the American Psychiatric Association noted approaching the 2021 winter holiday season. Underneath this overall statistic are important differences across various
The 2022 Health Populi TrendCast for Consumers and Health Citizens
I cannot recall a season when so many health consumer studies have been launched into my email inbox. While I have believed consumers’ health engagement has been The New Black for the bulk of my career span, the current Zeitgeist for health care consumerism reflects that futurist mantra: “”We tend to overestimate the effect of a technology in the short run and underestimate the effect in the long run,” coined by Roy Amara, past president of Institute for the Future. That well-used and timely observation is known as Amara’s Law. This feels especially apt right “now” as we enter 2022,
3 in 4 Insured Americans Worried About Medical Bills — Especially Women
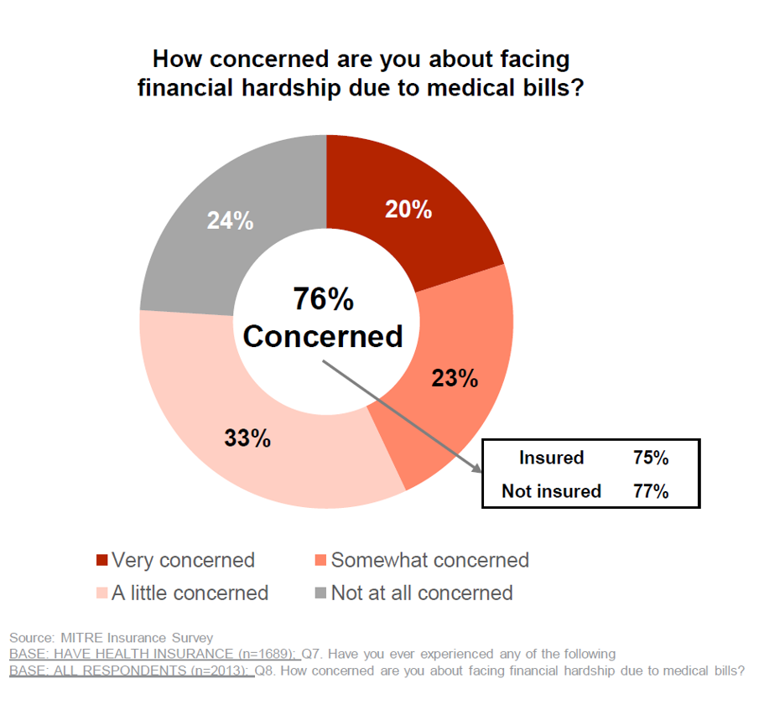
In the U.S., being covered by health insurance is one of the social determinants of health. Without a health plan, an uninsured person in America is far more likely to file for bankruptcy due to medical costs, and lack access to needed health care (and especially primary care). But even with health insurance coverage, most health-insured people are concerned about medical costs in America, found in a MITRE-Harris Poll on U.S. consumers’ health insurance perspectives published today. “Even those fortunate to have insurance struggle with bills that result from misunderstanding or underestimating costs of treatments and procedures,” Juliette Espinosa of
The Cost to Cover Health Insurance for a Family in America Is $22,221
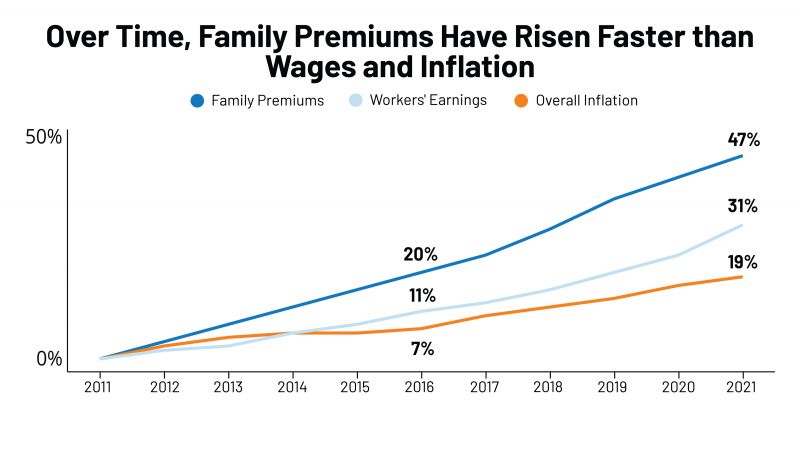
Even with growing inflation in the U.S. and post-pandemic job growth in 2021, the cost of health insurance premiums rose faster than either the price of goods or wages. That family health plan premium reached $22,221, an increase of 22% since 2016, we learn in the annual report from Kaiser Family Foundation, 2021 Employer Health Benefits Survey. This report is our go-to encyclopedia of statistics on health insurance year-after-year, surveying companies’ annual health insurance strategies for coverage and tactics for managing spending and workers’ health outcomes. This 2021 update takes into account the impacts and influence of COVID-19 on workers’
Be Mindful About What Makes Health at HLTH
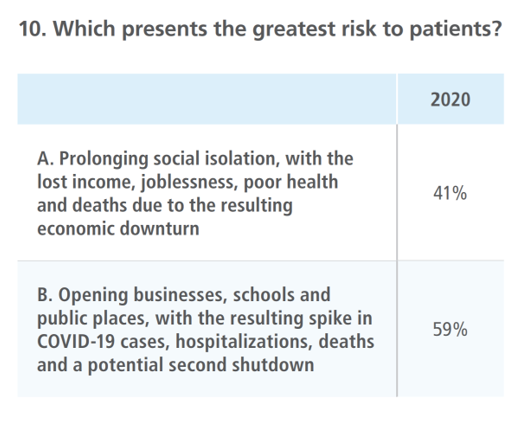
“More than a year and a half into the COVID-19 outbreak, the recent spread of the highly transmissible delta variant in the United States has extended severe financial and health problems in the lives of many households across the country — disproportionately impacting people of color and people with low income,” reports Household Experiences in America During the Delta Variant Outbreak, a new analysis from the Robert Wood Johnson Foundation, NPR, and the Harvard Chan School of Public Health. As the HLTH conference convenes over 6,000 digital health innovators live, in person, in Boston in the wake of the delta
Genentech’s Look Into the Mirror of Health Inequities

In 2020, Genentech launched its first study into health inequities. The company spelled out their rationale to undertake this research very clearly: “Through our work pursuing groundbreaking science and developing medicines for people with life-threatening diseases, we consistently witness an underrepresentation of non-white patients in clinical research. We have understood inequities and disproportionate enrollment in clinical trials existed, but nowhere could we find if patients of color had been directly asked: ‘why?’ So, we undertook a landmark study to elevate the perspectives of these medically disenfranchised individuals and reveal how this long-standing inequity impacts their relationships with the healthcare system
Chronic Medical Conditions, Mental Health, and Equity On Employers’ Minds for 2022 – Employee Health in the Wake of COVID-19
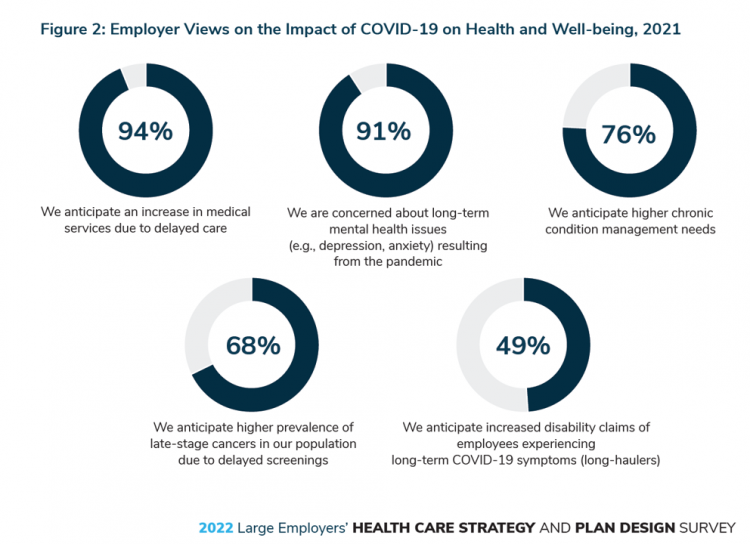
One in two people in the U.S. receive health insurance through employers. As large employers tend to be on the vanguard of benefit plan design, it’s useful to understand how these companies are thinking ahead on behalf of their employees. With that objective, it’s always instructive to explore the annual study from the Business Group on Health, the 2022 Large Employers’ Health Care Strategy and Plan Design Survey. As a result of the COVID-19 pandemic, large employees have many concerns about worker and dependents’ health. The biggest firms in America providing health insurance for workers are expecting an increase in
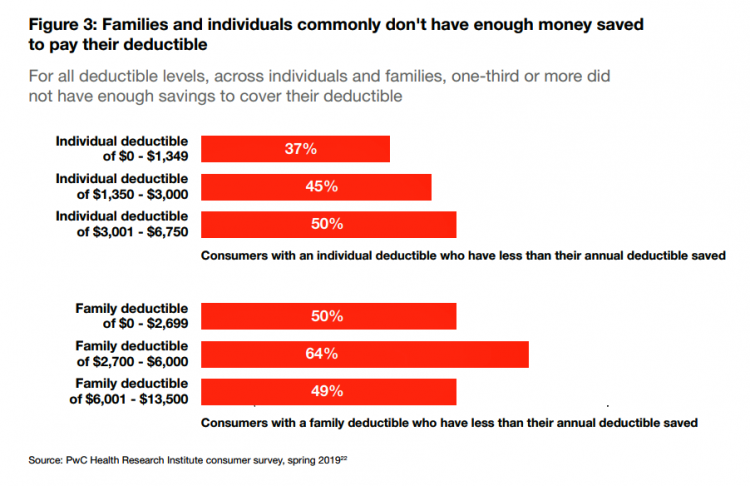
Why Is So Much “Patient Experience” Effort Focused on Financial Experience?
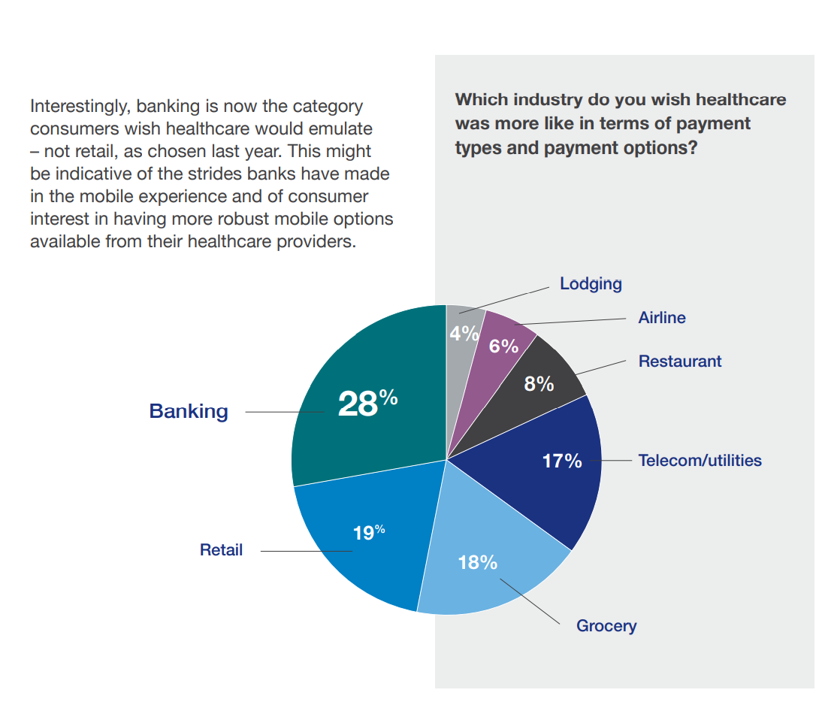
Financial Experience (let’s call it FX) is the next big thing in the world of patient experience and health care. Patients, as health consumers, have taken on more of the financial risk for health care payments. The growth of high-deductible health plans as well as people paying more out-of-pocket exposes patients’ wallets in ways that implore the health care industry to serve up a better retail experience for patients. But that just isn’t happening. One of the challenges has been price transparency, which is the central premise of this weekend’s New York Times research-rich article by reporters Sarah Kliff and
Nurses and Aides Are Beloved and Deserve Higher Pay; and a Spotlight on the Filipinx Frontline
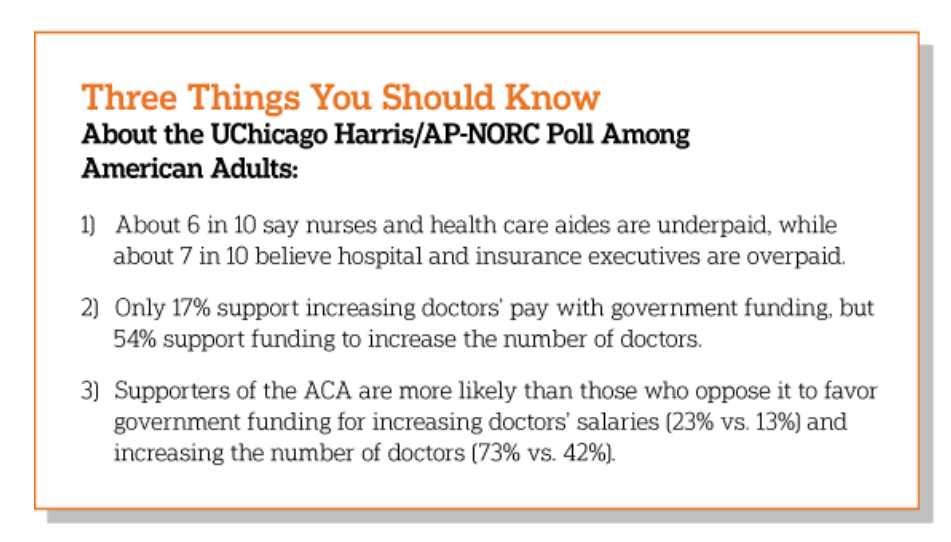
A majority of Democrats, Independents, and Republicans agree that nurses are underpaid. Most Americans across political parties also believe that hospital executives are overpaid, according to a poll from The Associated Press-NORC Center for Public Affairs Research. The survey analysis is aptly titled, Most Americans Agree That Nurses and Aides Are Underpaid, While Few Support Using Federal Dollars to Increase Pay for Doctors, . Insurance executives are also overpaid, according to 73% of Americans — an even higher percent of people than the 68% saying hospital execs make too much money. In addition to nurses being underpaid, 6 in 10
Our Pandemic Lessons: Listening to Michael Dowling – a #HIMSS21 Wrap-Up

“We don’t un-learn,” Dr. Amy Abernethy asserted as she shared her pandemic perspectives on a panel with 2 other former U.S. health policy and regulatory leaders. The three spoke about navigating compliance (think: regulations and reimbursement) in an uncertain world. An uncertain world is our workplace in the health/care ecosystem, globally, in this moment. So to give us some comfort in our collective foxhole, my last post for this week of immersion in #HIMSS21 is based on the keynote speech of Michael Dowling, CEO of Northwell Health. Dowling keynoted on the theme of “Leading for the Future,” sharing his lessons
Reimagining Life After the Pandemic – Seeking Health, Safety, Sustainability, and Trust
COVID-19 reshaped people around the world, one-half of whom are re-defining their personal purpose and life-goals. This sense of purpose extends to peoples’ willingness to buy or patronize companies who do not meet their needs for health, safety, sustainability and trust. For example, two in three of these people would switch travel brands if they felt health and safety weren’t up to par, discovered in Life Reimagined – Mapping the motivations that matter for today’s consumers, from Accenture’s Voices of Change series. In May 2021, Accenture polled over 25,000 consumers globally, in 22 countries, and found that one-half of people
One in Two Americans with Work-Based Insurance Worries That Healthcare Costs Could Lead to Bankruptcy
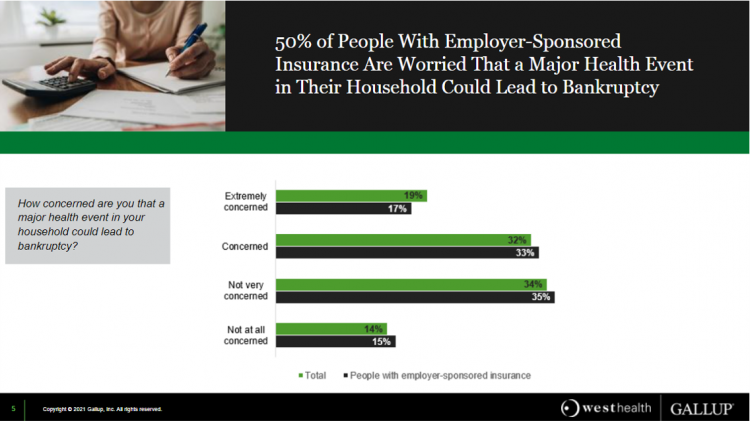
One in two people in the U.S. with employer-sponsored health insurance worry that a major health event in their household could lead to bankruptcy, according to research gathered by West Health and Gallup in Business Speaks: The Future of Employer-Sponsored Insurance. Gallup and West Health presented their study in a webinar earlier this week; in today’s post, I feature a few key data points that particularly resonate as I celebrate/appreciate yesterday’s U.S. Supreme Court’s ruling on the Affordable Care Act (i.e., California v. Texas) combined with a new study published in JAMA Network Open, discussed below the digital fold in
Post-Pandemic, U.S. Healthcare is Entering a “Provide More Care For Less” Era – Pondering PwC’s 2022 Forecast

In the COVID-19 pandemic, health care spending in the U.S. increased by a relatively low 6.0% in 2020. This year, medical cost trend will rise by 7.0%, expected to decline a bit in 2022 according to the annual study from PwC Health Research Institute, Medical Cost Trend: Behind the Numbers 2022. What’s “behind these numbers” are factors that will increase medical spending (the “inflators” in PwC speak) and the “deflators” that lower costs. Looking around the future corner, the inflators are expected to be: A COVID-19 “hangover,” leading to increased health care services utilization Preparations for the next pandemic, and
The Cost of Health Care for a Family of 4 in America Will Reach $28,256 in 2021
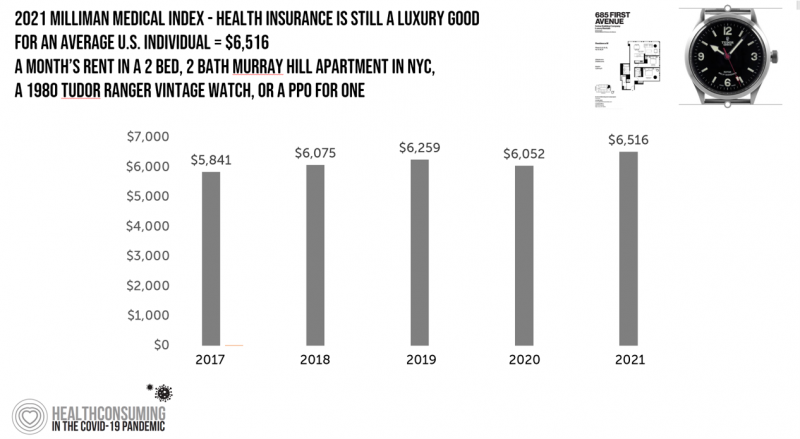
The good news for health care costs for a family of four in America is that they fell, for the first time in like, ever, in 2020. But like a déjà vu all over again, annual health care costs for a family of four enrolled in a PPO will climb to over $28,000 in 2021, based on the latest 2021 Milliman Medical Index (MMI). The first chart shows how health care costs declined in our Year of COVID, 2020, by over $1,000 for that hypothetical U.S. family. But costs rise with a statistical vengeance this year, by nearly $2,200 per family–about
Virtual Health Tech Enables the Continuum of Health from Hospital to Home

In the COVID-19 pandemic, as peoples’ daily lives shifted closer and closer to home, and for some weeks and months home-all-the-time, health care, too, moved beyond brick-and-mortar hospitals and doctors’ offices. The public health crisis accelerated “what’s next” for health care delivery, detailed in A New Era of Virtual Health, a report published by TripleTree. TripleTree is an investment bank that has advised health care transactions since 1997. As such, the team has been involved in digital health financing and innovation for 24 years, well before the kind of platforms, APIs, and cloud computing now enabling telehealth and care, everywhere. The
The Pandemic’s Death Rate in the U.S.: High Per Capita Income, High Mortality
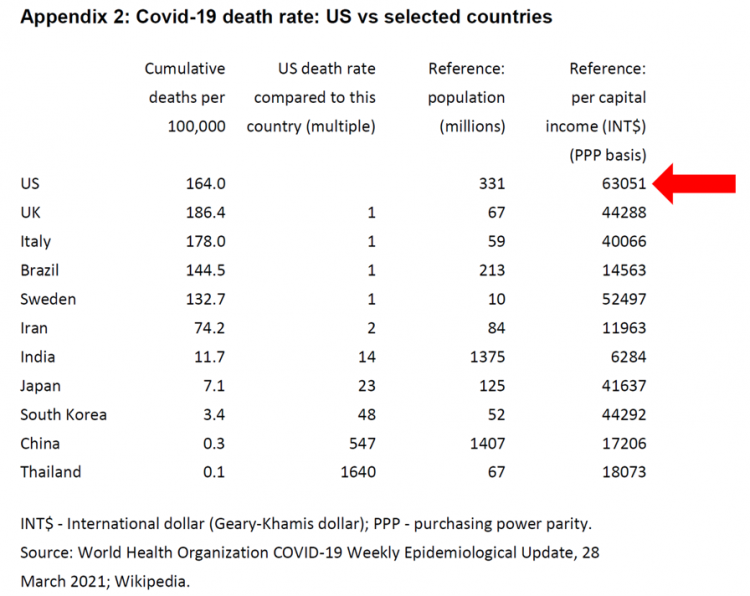
The United States has among the highest per capita incomes in the world. The U.S. also has sustained among the highest death rates per 100,000 people due to COVID-19, based on epidemiological data from the World Health Organization’s March 28, 2021, update. Higher incomes won’t prevent a person from death-by-coronavirus, but risks for the social determinants of health — exacerbated by income inequality — will and do. I have the good fortune of access to a study group paper shared by Paul Sheard, Research Fellow at the Mossaver-Rahmani Center for Business and Government at the Harvard Kennedy School. In reviewing
The Continued Erosion of Trust in the Age of COVID
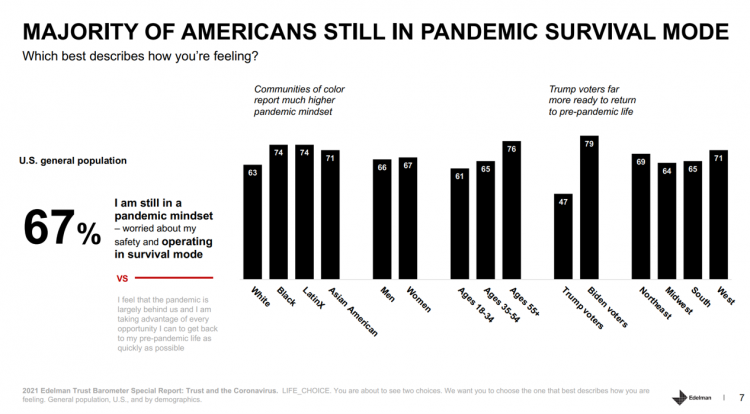
A year into the COVID-19 pandemic, most Americans are still in “survival mode,” according to an update of the 2021 Edelman Trust Barometer, Trust and the Coronavirus in the U.S. Updating the company’s annual Trust Barometer, Edelman conducted a new round of interviews in the U.S. among 2,500 people in early March. [For context, you can read my take on the 2021 Edelman Trust Barometer published during the World Economic Forum in January 2021 here in Health Populi]. The first chart shows that two in three people in the U.S. are still in a pandemic mindset, worried about safety and
Primary Care 2.0 – How Crossover Health is “Re-Bundling” Health Care

In 2020, investments in digital health reached $14.1 bn, much of which went into niche applications like lab testing, medication adherence, and on-demand triage for urgent care. These companies targeting primary care components represent the “unbundling of the family doctor,” as CB Insights recently coined the market trend. Fragmentation is a hallmark of the U.S. health care system, or more aptly “non-system” as my old friend J.D. Kleinke noted in his book titled Oxymorons….published in 2001. Twenty years later, we confront primary care as a dichotomy: as unbundled pieces of (we hope) innovation, and in organizations re-imagining a new continuity
Nurses, doctors, pharmacists join with teachers in Gallup’s 2021 honest and ethics poll
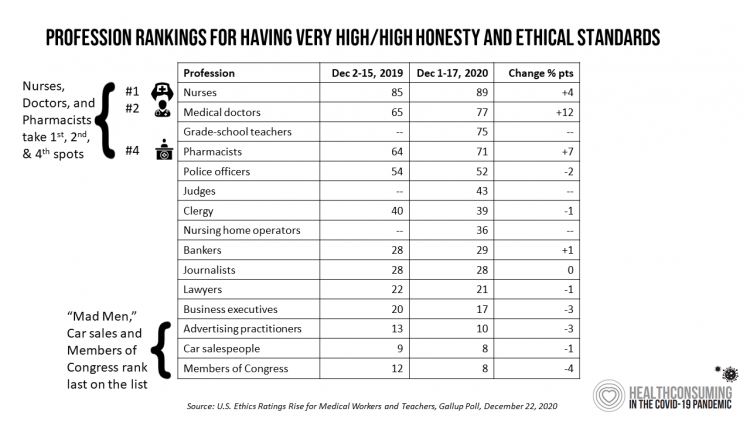
Each year, Americans rank nurses as the most honest and ethical professionals along, generally followed by doctors and pharmacists. In the middle of the coronavirus pandemic in the U.S., grade school teachers join the three medical professions in the annual Gallup Poll on the top-ranked professions for honest and ethical behavior in America as we enter 2021 with many U.S. hospitals’ intensive care units at full capacity….and schools largely emptied of students. The three health care professions scored their highest marks ever achieved in this Gallup Poll, which has been assessing honesty and ethics in America since 1999. Nurses are
The Comforts of Home Drive Demand for Healthcare There
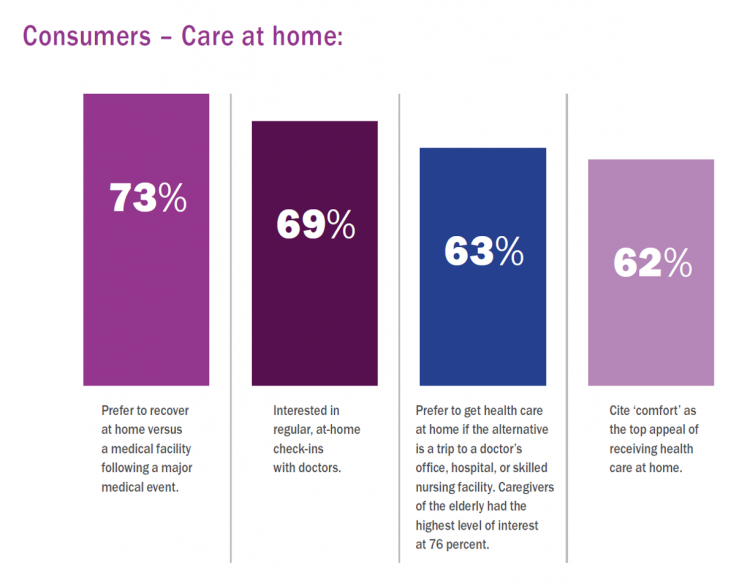
Two in three U.S. consumers skipped or delayed getting in-person medical care in 2020. One in 2 people had a telehealth visit int he last year. Most would use virtual care again. The coronavirus pandemic has mind-shifted how patients envision a health care visit. Today, most consumers prefer the idea of getting health care at home compared with going to a doctor’s office. Most Americans also like the idea of recovering at home instead of at a medical facility after a major medical event, according to the report, Health-at-Home 2020: The New Standard of Care Delivery from CareCentrix. COVID-19 has
The COVID-19 Era Has Grown Health Consumer Demand for Virtual Care
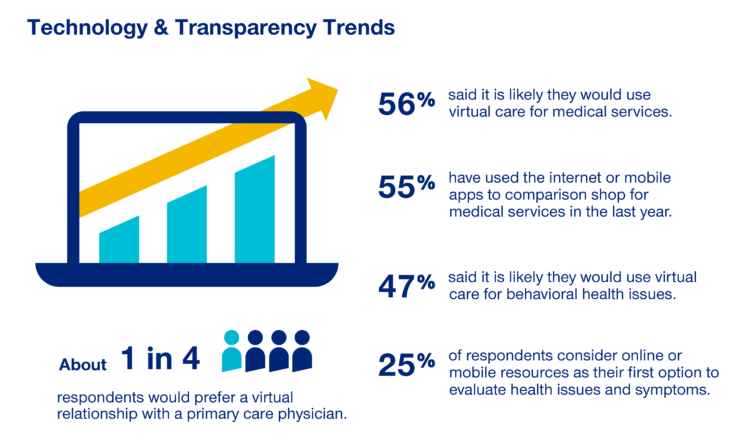
Over one-half of Americans would likely use virtual care for their healthcare services, and one in four people would actually prefer a virtual relationship with a primary care physician, according to the fifth annual 2020 Consumer Sentiment Survey from UnitedHealthcare. What a difference a pandemic can make in accelerating patients’ adoption of digital health tools. This survey was conducted in mid-September 2020, and so the results demonstrate U.S. health consumers’ growing digital health “muscles” in the form of demand and confidence in using virtual care. One in four people would consider online options as their first-line to evaluating personal health
In the Past Ten Years, Workers’ Health Insurance Premiums Have Grown Much Faster Than Wages
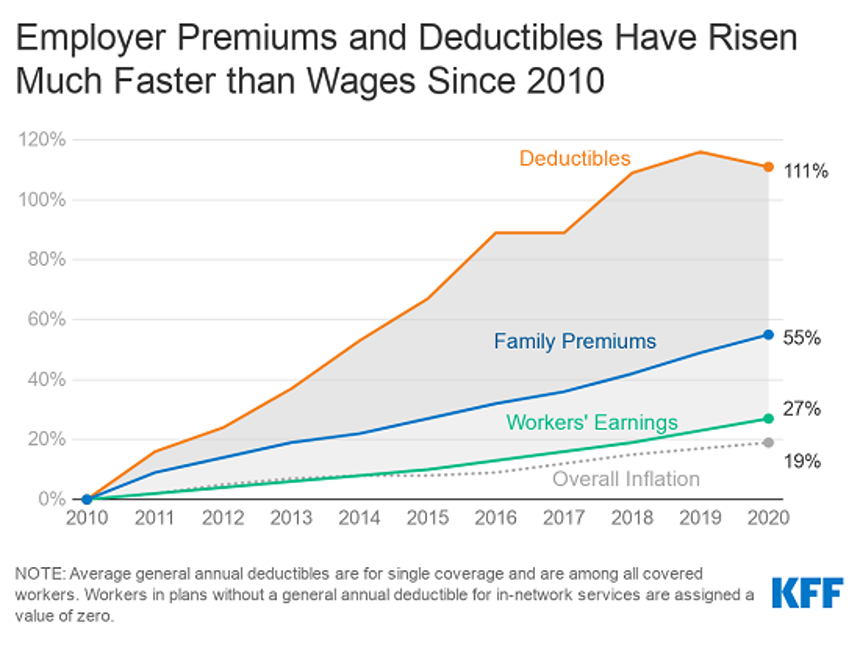
For a worker in the U.S. who benefits from health insurance at the workplace, the annual family premium will average $21,342 this year, according to the 2020 Employer Health Benefits Survey from the Kaiser Family Foundation. The first chart illustrates the growth of the premium shares split by employer and employee contributions. Over ten years, the premium dollars grew from $13,770 in 2010 to $21K in 2020. The worker’s contribution share was 29% in 2010, and 26% in 2020. Single coverage reached $7,470 in 2020 and was $5,049 in 2010. Roughly the same proportion of companies offered health benefits to
Only in America: The Loss of Health Insurance as a Toxic Financial Side Effect of the COVID-19 Pandemic

In terms of income, U.S. households entered 2020 in the best financial shape they’d been in years, based on new Census data released earlier this week. However, the U.S. Census Bureau found that the level of health insurance enrollment fell by 1 million people in 2019, with about 30 million Americans not covered by health insurance. In fact, the number of uninsured Americans rose by 2 million people in 2018, and by 1.9 million people in 2017. The coronavirus pandemic has only exacerbated the erosion of the health insured population. What havoc a pandemic can do to minds, bodies, souls, and wallets. By September 2020,
Health Insurance Affordability in the Time of the Coronavirus Pandemic
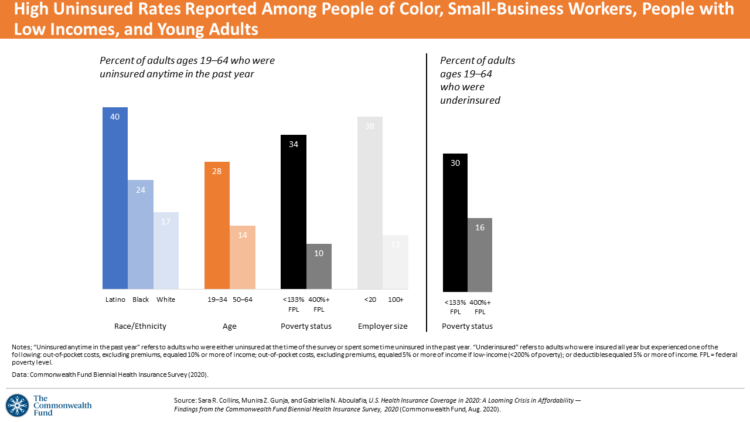
The coronavirus pandemic has revealed many flaws in the U.S. healthcare system, first and foremost the nation’s patchwork public health infrastructure and health inequities in mortality rates due to COVID-19. The Commonwealth Fund‘s biennial report, published as the pandemic continues into and beyond the third quarter of 2020, sheds light on another weakness in U.S. healthcare: the cost of health insurance relative to working Americans’ relatively flat incomes. I explored the details of this study in a post titled Health Insurance Affordability: A Call-to-Action for Healthcare Industry Stakeholders in the Pandemic, published on the Medecision Liberation blog site. The survey
Physicians Practicing in the Age of COVID-19: Lower Incomes, More Telehealth
In the midst of the coronavirus pandemic, two certainties emerge in the lives of physicians: they are generating less revenue, and they have adopted more virtual care in practices. The Physicians Foundation surveyed 3,513 physicians in July 2020 on their perspectives on COVID-19 and how the pandemic has impacted practices and patients. This study is part one of three conducted by the Foundation this year, subtitled the “COVID-19 Impact Edition” of the 2020 Survey of America’s Physicians which the Foundation conducts each year. Merritt Hawkins conducted the study on behalf of the Foundation, shifting the focus to the pandemic. This
The Median Hospital Charge In the U.S. for COVID-19 Care Ranges From $34-45K
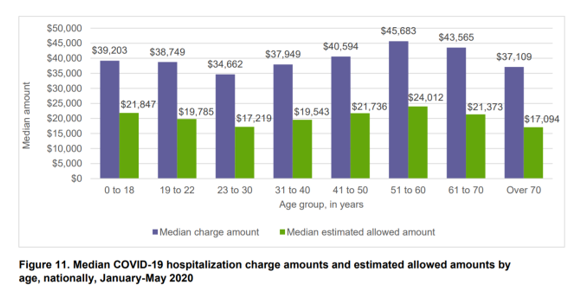
The median charge for hospitalizing a patient with COVID-19 ranged from $34,662 for people 23 to 30, and $45,683 for people between 51 and 60 years of age, according to FAIR Health’s research brief, Key Characteristics of COVID-19 Patients published July 14th, 2020. FAIR Health based these numbers on private insurance claims associated with COVID-19 diagnoses, evaluating patient demographics (age, gender, geography), hospital charges and estimated allowed amounts, and patient comorbidities. They used two ICD-10-CM diagnostic codes for this research: U07.1, 2019-nCoV acute respiratory disease; and, B97.29, other coronavirus as the cause of disease classified elsewhere which was the original code
As Americans Start to Return-to-Work in the Summer of COVID, Mental Health is a Top Concern Among Employers
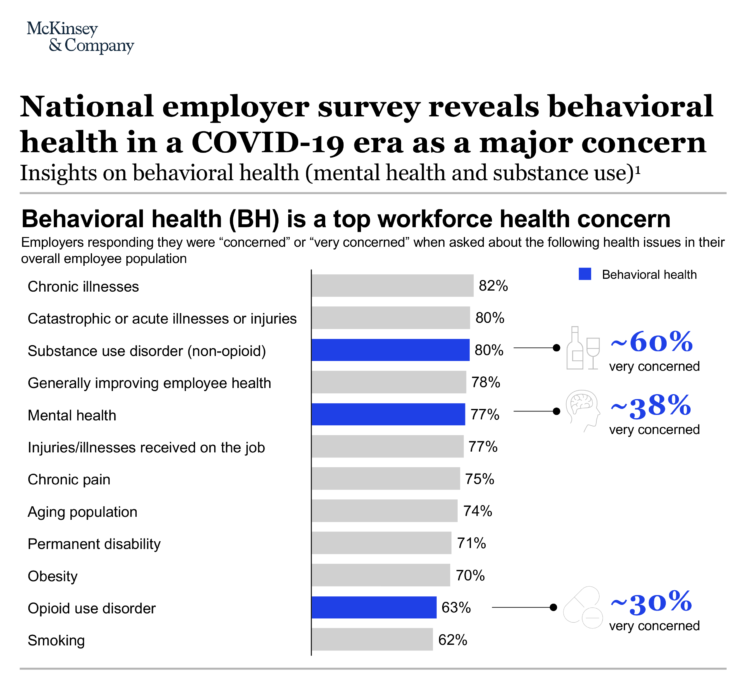
Most U.S. employers worry about workers’ mental health and substance use as employees begin returning to work in the summer of 2020. About 4 in 5 U.S. companies are “very concerned” or “concerned” about employees’ chronic illnesses, acute illnesses, and injuries along with behavioral health issue, based on McKinsey’s annual employer survey which coincided this year with the COVID-19 pandemic. Challenges of opioid use in the workforce remain a concern for two-thirds of U.S. companies, as well. Some 9 in 10 U.S. companies say behavioral health has a negative impact on workforce productivity. In response, 7 in 10 employers are
Saving Money as a Financial Vaccine: BlackRock Finds Consumer Savings Drain and Etsy Sellers Not Saving Much
“Americans are feeling incredible financial pressure as a result of the COVID outbreak,” John Thompson, Chief Program Officer with the Financial Health Network. One in three people in the U.S. has skipped or stopped paying a bill, and over half of Americans have used emergency savings, according to a survey from the BlackRock Emergency Savings Initiative (ESI). BlackRock, the investment firm, allocated $50 million in February 2019 to form the ESI, focused on helping people with lower incomes to bolster savings and financial health. BlackRock partners in the ESI with the Financial Health Network, CommonWealth, the Center for Advanced Hindsight Common
Stress in America – COVID-19 Takes Toll on Finances, Education, Basic Needs and Parenting

“The COVID-19 pandemic has altered every aspect of American life, from health and work to education and exercise,” the new Stress in America 2020 study from the American Psychological Association begins. The APA summarizes the impact of these mass changes on the nation: “The negative mental health effects of the coronavirus may be as serious as the physical health implications,” with COVID-19 stressors hitting all health citizens in the U.S. in different ways. Beyond the risk of contracting the virus, the Great Lockdown of the U.S. economy has stressed the U.S. worker and the national economy, with 7 in 10
What $6,553 Buys You in America: A Luxury Watch, a Year at Valdosta State, or a PPO for One – the 2020 Milliman Medical Index
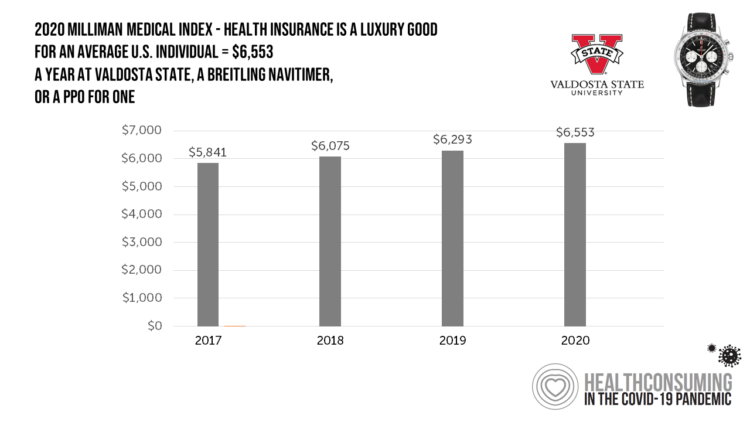
Imagine this: you find yourself with $6,553 in your pocket and you can pick one of the following: A new 2020 Breitling Navitimer watch; A year’s in-state tuition at Valdosta State University; or, A PPO for an average individual. Welcome to the annual Milliman Medical Index (MMI), which gauges the yearly price of an employer-sponsored preferred-provider organization (PPO) health insurance plan for a hypothetical American family and an N of 1 employee. That is a 4.1% increase from the 2019 estimate, about twice the rate of U.S. gross domestic product growth, Milliman points out in its report. Milliman bases
COVID-19’s Consumer Health Care Behaviors: Telehealth, Trauma, and Trust, via PwC
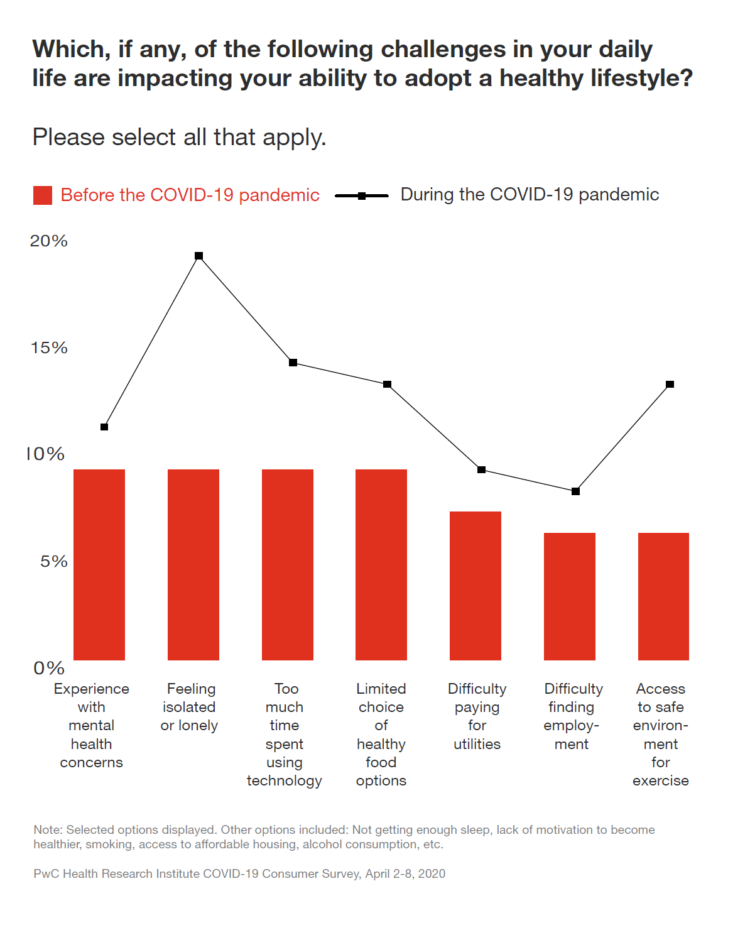
In a matter of several weeks, people living in the U.S. have endured massive personal social, emotional, physical and fiscal disruption due to the COVID-19 pandemic. State mandates to shelter at home, the adoption of wearing face masks and covers in public, and re-making dining tables and dens into home-working spaces for kids in school or parents telecommuting, American homes have morphed into petri dishes of people undergoing dramatic changes in a very short time. A new report from PwC looks at peoples’ changes in health behaviors in the first two months of the pandemic, asking whether these changes will
The Coronavirus Impact on American Life, Part 1 – Life Disrupted, and Money Concerns
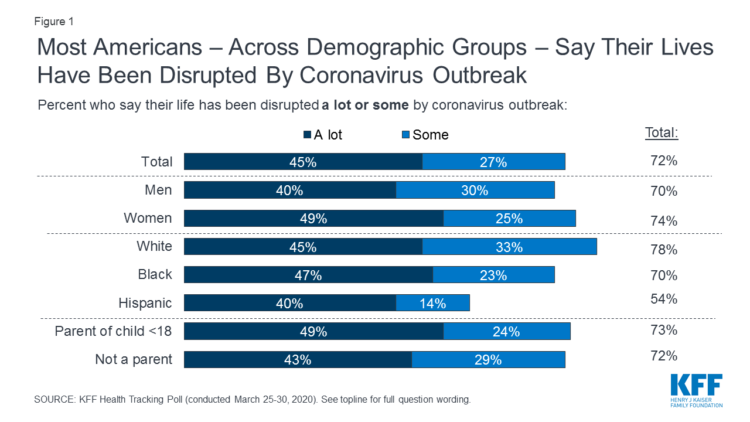
Nearly 3 in 4 Americans see their lives disrupted by the coronavirus pandemic, according to the early April Kaiser Family Foundation Health Tracking Poll. This feeling holds true across most demographic factors: among both parents and people without children; men and women alike; white folks as well as people of color (although fewer people identifying as Hispanic, still a majority). There are partisan differences, however, in terms of who perceives a life-disruption due to COVID-19: 76% of Democrats believe this, 72% of Independents, and 70% of Republicans. Interestingly, only 30% of Republicans felt this way in March 2020, more than
Estimates of COVID-19 Medical Costs in the US: $20K for inpatient stay, $1300 OOP costs
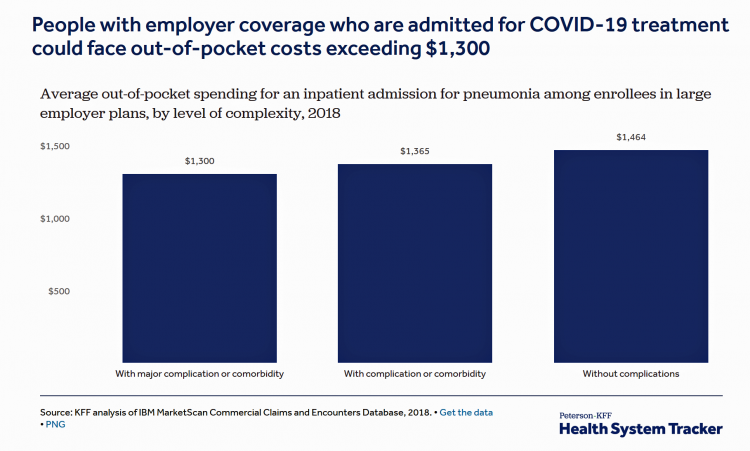
In the midst of growing inpatient admissions and test results for COVID-19, Congress is working as I write this post to finalize a round of legislation to help Americans with the costs-of-living and (hopefully) health care in a national, mandated, clarifying way. Right now in the real world, real patients are already being treated for COVID-19 in American hospitals. Patients are facing health care costs that may result in multi-thousand dollar bills at discharge (or death) that will decimate households’ financial health, particularly among people who don’t have health insurance coverage, covered by skinny or under-benefited plans, and/or lack banked
The High Cost-of-Thriving and the Evolving Social Contract for Health Care
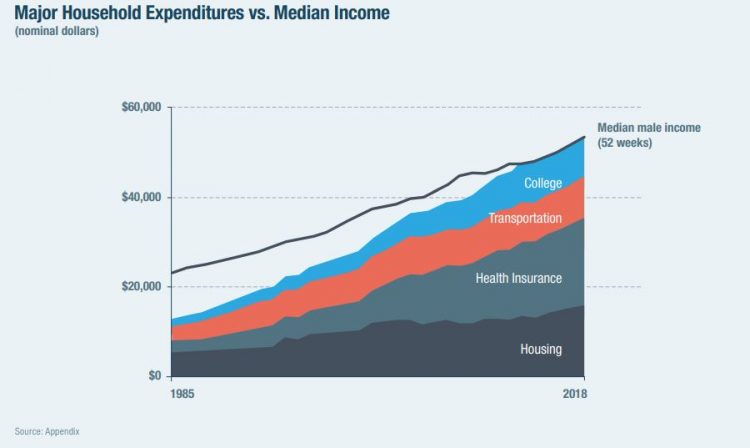
Millions of Americans have to work 53 weeks to cover a year’s worth of household expenses. Most Americans haven’t saved much for their retirement. Furthermore, the bullish macroeconomic outlook for the U.S. in early 2020 hasn’t translated into individual American’s optimism for their own family budgets. (Sidebar and caveat: yesterday was the fourth day in a row of the U.S. financial markets losing as much as 10% of market cap, so the global economic outlook is being revised downward by the likes of Goldman Sachs, Vanguard, and Morningstar, among other financial market prognosticators. MarketWatch called this week the worst market
Most Workers and their Employers Want to Receive Digital Healthcare On-Demand
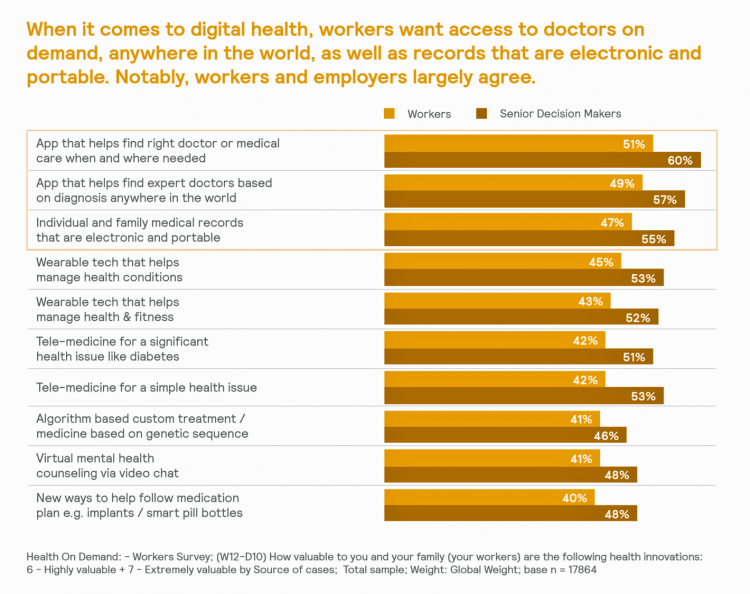
Most employers and their workers see the benefits of digital health in helping make health care more accessible and lower-cost, according to survey research published in Health on Demand from Mercer Marsh Benefits. Interestingly, more workers living in developing countries are keener on going digital for health than people working in wealthier nations. Mercer’s study was global, analyzing companies and their employees in both mature and growth economies around the world. In total, Mercer interviewed 16,564 workers and 1,300 senior decision makers in companies. The U.S. sample size was 2,051 employees and 100 decision makers. There’s a treasure trove of insights
Come Together – A Health Policy Prescription from the Bipartisan Policy Center
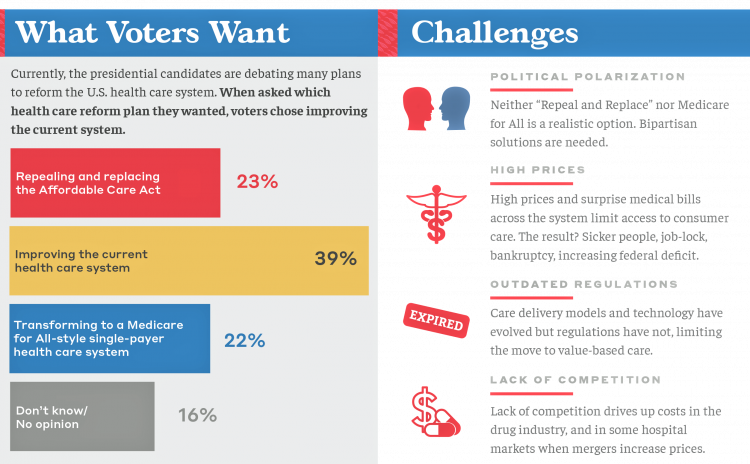
Among all Americans, the most popular approach for improving the health care in the U.S. isn’t repealing or replacing the Affordable Care Act or moving to a Medicare-for-All government-provided plan. It would be to improve the current health care system, according to the Bipartisan Policy Center’s research reported in a Bipartisan Rx for America’s Health Care. The BPC is a truly bipartisan organization, co-founded by Former Democratic Senate Majority Leaders Tom Daschle and George Mitchell, and Former Republican Senate Majority Leaders Howard Baker and Bob Dole. While this political week in America has revealed deep chasms between the Dems and
What’s Causing Fewer Primary Care Visits in the US?
Americans who have commercial health insurance (say, through an employer or union) are rarely thought to face barriers to receiving health care — in particular, primary care, that front line provider and on-ramp to the health care system. But in a new study published in the Annals of Internal Medicine, commercially-insured adults were found to have visited primary care providers (PCPs) less often, and 1 in 2 had no PCP visits in one year. In Declining Use of Primary Care Among Commercially Insured Adults in the United States, 2008-2016, the researchers analyzed data from a national sample of adult health
Income Inequality is Fostering Mis-Trust, the Edelman 2020 Trust Barometer Observes
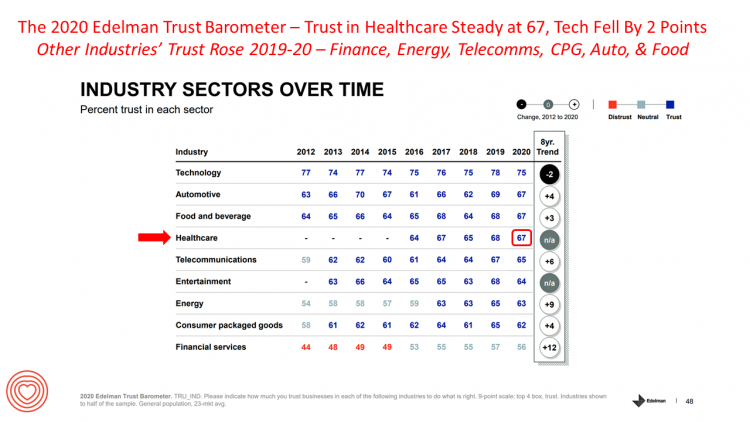
Economic development has historically built trust among nations’ citizens. But in developed, wealthier parts of the world, like the U.S., “a record number of countries are experiencing an all-time high ‘mass-class’ trust divide,” according to the 2020 Edelman Trust Barometer. For 20 years, Edelman has released its annual Trust Barometer every year at the World Economic Forum in Davos, recognizing the importance of trust in the global economy and society. Last year, it was the employer who was the most-trusted touch-point in citizens’ lives the world over, I discussed in Health Populi one year ago. This year, even our employers can’t
In 2020, PwC Expects Consumers to Grow DIY Healthcare Muscles As Medical Prices Increase

The new year will see a “looming tsunami” of high prices in healthcare, regulation trumping health reform, more business deals reshaping the health/care industry landscape, and patients growing do-it-yourself care muscles, according to Top health industry issues of 2020: Will digital start to show an ROI from the PwC Health Research Institute. I’ve looked forward to reviewing this annual report for the past few years, and always learn something new from PwC’s team of researchers who reach out to experts spanning the industry. In this 14th year of the publication, PwC polled executives from payers, providers, and pharma/life science organizations. Internally,
The Patient As Payor: Workers Covered by Employer Health Insurance Spend 11.5% of Household Incomes on Premiums and Deductibles
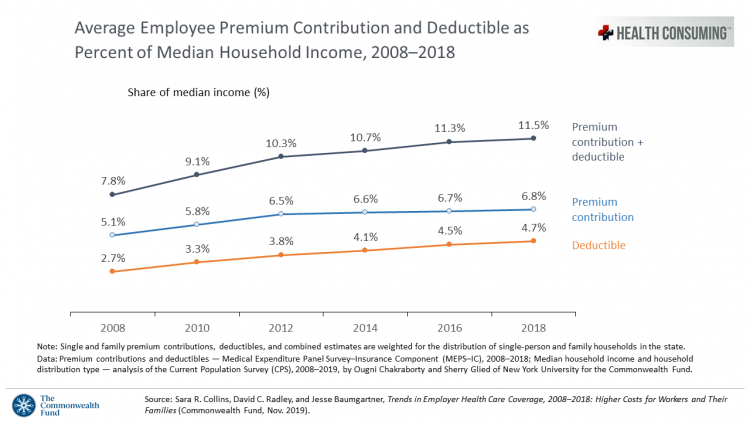
Workers covered by health insurance through their companies spend 11.5% of their household income on health insurance premiums and deductibles based on The Commonwealth Fund’s latest report on employee health care costs, Trends in Employer Health Coverage, 2008-2018: Higher Costs for Workers and Their Families. The topline of this study is that average annual growth in employer premiums rose faster between 2016 and 2017, by about 5% for both single and family plans. The bottom line for families is that workers’ premium payments grew faster than median incomes did over the ten years 2008 to 2018. Average deductibles also outpaced
A Tale of Two Americas as Told by the 2019 OECD Report on Health

It was the best of times, It was the worst of times, It was the age of wisdom, it was the age of foolishness, It was the epoch of belief, it was the epoch of incredulity, … starts Dickens’ Tale of Two Cities. That’s what came to my mind when reading the latest global health report from the OECD, Health at a Glance 2019, which compares the United States to other nations’ health care outcomes, risk factors, access metrics, and spending. Some trends are consistent across the wealthiest countries of the world, many sobering, such as: Life expectancy rates fell in 19 of the
Thinking About Health Care One Year From the 2020 Presidential Election

Today is 4th November 2019, exactly one year to the day that Americans can express their political will and cast their vote for President of the United States. Health care will be a key issue driving people to their local polling places, so it’s an opportune moment to take the temperature on U.S. voters’ perspectives on healthcare reform. This post looks at three current polls to gauge how Americans are feeling about health care reform 365 days before the 2020 election, and one day before tomorrow’s 2019 municipal and state elections. Today’s Financial Times features a poll that found two-thirds
Health Consumer Behaviors in the U.S. Stall, Alegeus Finds in the 2019 Index
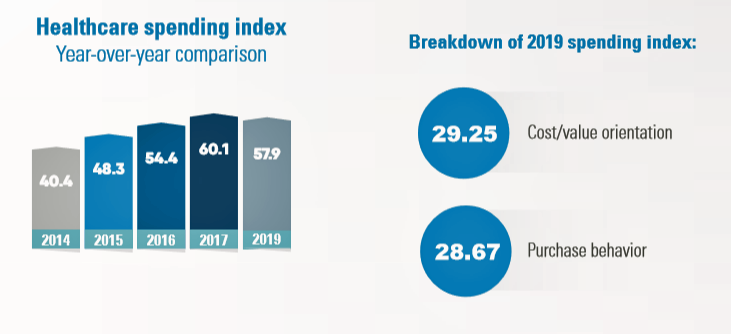
In the U.S., the theory of and rationale behind consumer-directed health has been that if you give a patient more financial skin-in-the-game — that is, to compel people to spend more out-of-pocket on health care — you will motivate that patient to don the hat of a consumer — to mindfully research, shop around, and purchase health care in a rational way, benefit from lower-cost and high-quality healthcare services. For years, Alegeus found that patients were indeed growing those consumer health muscles to save and shop for health care. In 2019, it appears that patients have backslid, according to the
Wasted: $1 of Every $4 Spent on Health Care In America
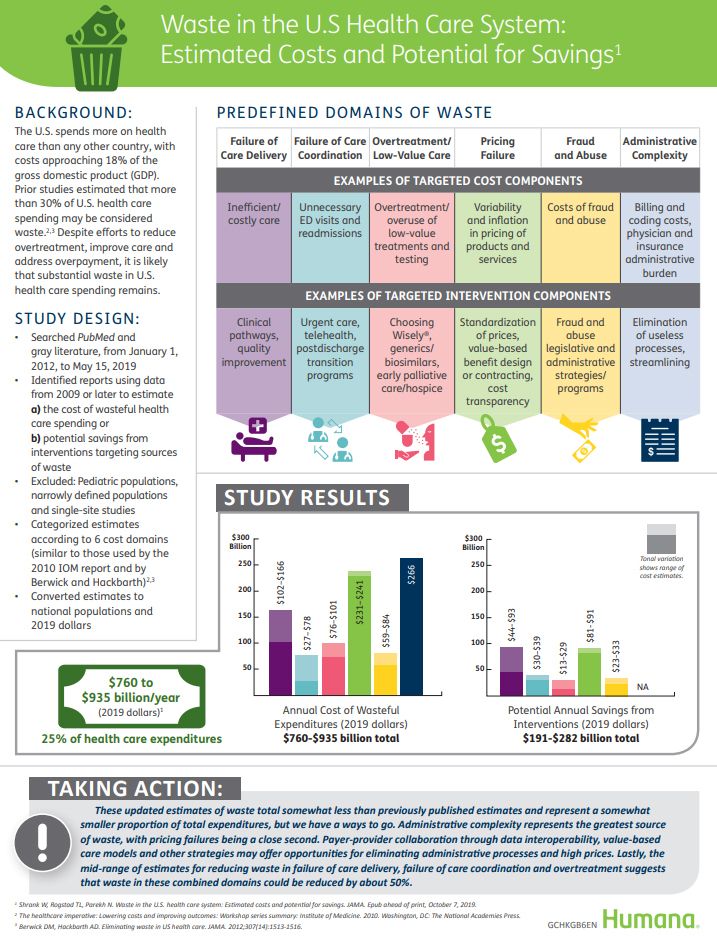
A study in JAMA published this week analyzed research reports that have measured waste in the U.S. health care system, calculating that 25% of medical spending in America is wasted. If spending is gauged at $3.8 trillion, waste amounts to nearly $1 trillion. If spending is 18% of the American gross domestic product (GDP), then some 4.5% of the U.S. economy is wasted spending by the health care system and its stakeholders. In “Waste in the US Health Care System,” a team from Humana and the Univrsity of Pittsburgh recalibrated the previous finding of 30% of wasted spending to the 25%,
Health @ Retail – Prelude to GMDC SelfCare Summit with Updates from Hims & Hers, GoodRx, Sam’s Club and Amazon Care
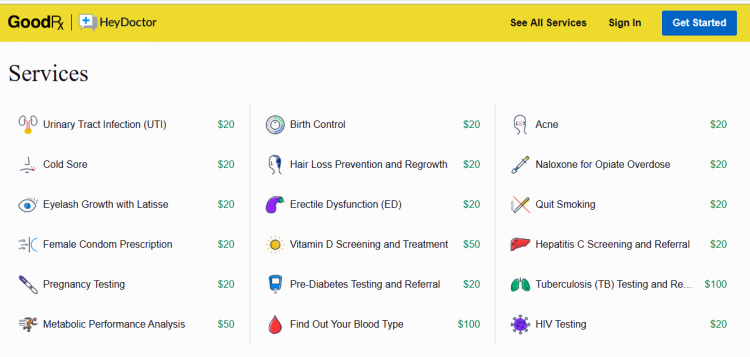
“We knew millions of people weren’t getting the care they needed — they were either too embarrassed to seek help or felt stuck in a system that was confusing and intimidating. Digital health has the potential to radically change the way people approach their wellness and, since launching in 2017, we’ve outpaced even our own expectations, delivering more than 1 million Hims & Hers products to our customers. In collaboration with highly-qualified doctors and healthcare providers, we’ve built a digital health platform that is changing the way people talk about and receive the care they need.” That’s a verbatim paragraph
“It’s the Deductible, Stupid” – Health Premiums Reach $20,576 in 2019 for a Family
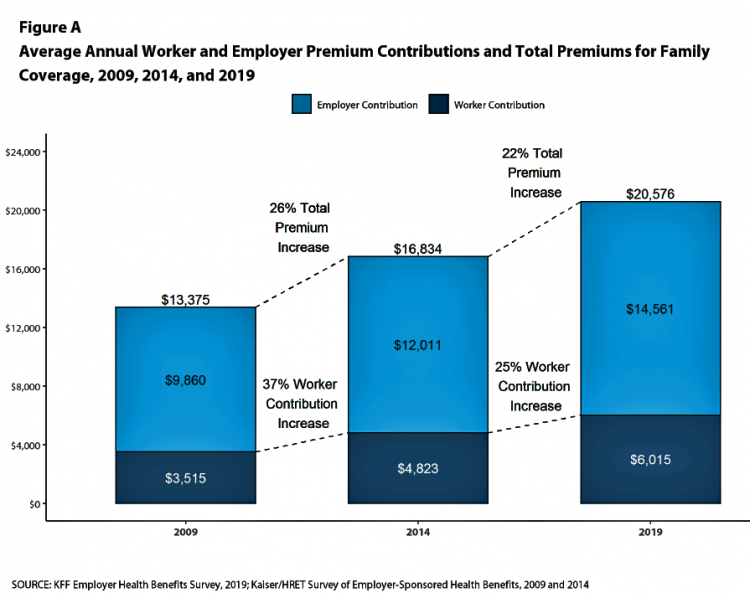
Here’s the latest arithmetic on American workers’ financial trade-off of wages for health care insurance coverage: in the ten years since 2009, family premiums have risen 54% and workers’ contribution to health care spending grew 71%. Wages? They rose 26%, and general price inflation by 20%, according to the Kaiser Family Foundation survey on employer-sponsored benefits for 2019 released yesterday. Survey details for this 21st annual encyclopedia on employer-sponsored health care are published in Health Affairs October 2019 issue in a paper titled, Health Benefits in 2019: Premiums Inch Higher, Employers Respond to Federal Policy. Because this
Worrying About Paying for Health Care Is the Norm in America

Among stresses facing people at least 50 years of age, health care costs rank top of mind compared with other issues like long-term care, health insurance, Social Security, taxes, and being read to retire. Worries about health care costs are particularly stressful among future retirees, 8 of 10 of whom share this top concern along with 7 in 10 recent retirees and 6 in 10 people retired for at least a decade. Health care stress cuts in two ways: most people are worried about paying for health care, as well as experienced an unanticipated decline in their health, according to
The New Employer Wellness Lens Includes Mental Health, Telehealth and Women’s Health
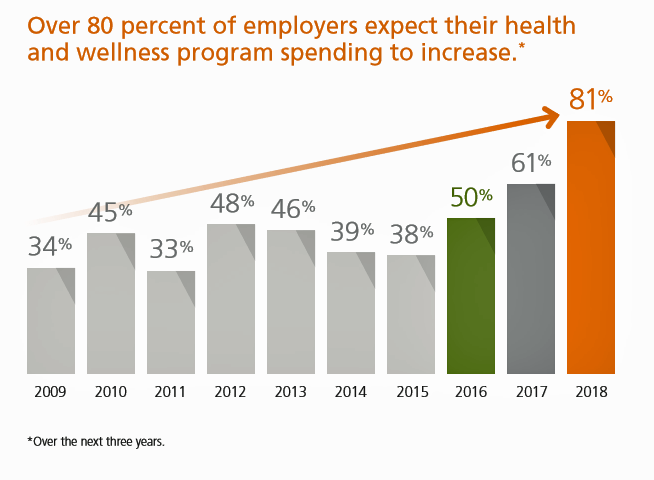
U.S. employers are tightening their focus on mental and behavioral health, addressing workers’ chronic conditions, emphasizing women’s health, and allocating more resources to digital and telehealth investments, we learn from Optum’s Ten Years of Health and Well-Being at Work: Learning from our past and reimagining the future. Four in five medium, large and jumbo companies expect their spending on health and wellness programs will increase over the next three years. That spending will have a strong focus on behavioral health services: 9 in 10 employers are concerned with the level of access workers have to mental health services. Companies will
Getting More Personal, Virtual and Excellent – the 2020 NBGH Employer Report
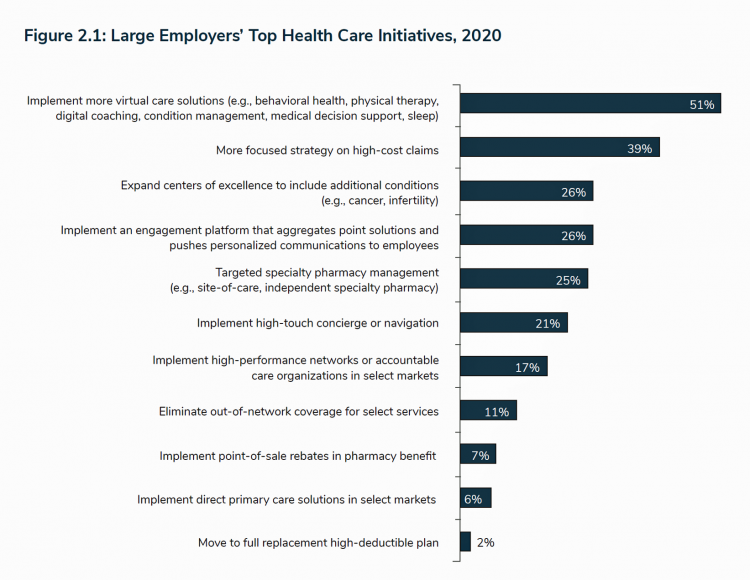
In 2020, large employers will be “doubling down” efforts to control health care costs. Key strategies will include deploying more telehealth and virtual health care services, Centers of Excellence for high-cost conditions, and getting more personal in communicating and engaging through platforms. This is the annual forecast for 2020 brought to us by the National Business Group of Health (NBGH), the Large Employers’ Health Care Strategy and Plan Design Survey. The 42-page report is packed with strategic and tactical data looking at the 2020 tea leaves for large employers, representing over 15 million covered lives. Nearly 150 companies were surveyed
Talking “HealthConsuming” on the MM&M Podcast

Marc Iskowitz, Executive Editor of MM&M, warmly welcomed me to the Haymarket Media soundproof studio in New York City yesterday. We’d been trying to schedule meeting up to do a live podcast since February, and we finally got our mutual acts together on 6th August 2019. Here’s a link to the 30-minute conversation, where Marc combed through the over 500 endnotes from HealthConsuming‘s appendix to explore the patient as the new health care payor, the Amazon prime-ing of people, and prospects for social determinants of health to bolster medicines “beyond the pill.” https://www.pscp.tv/MMMnews/1eaJbvgovBYJX Thanks for listening — and if you
Milliman Finds PPO for Family of 4 in 2019 Will Cost $28,386
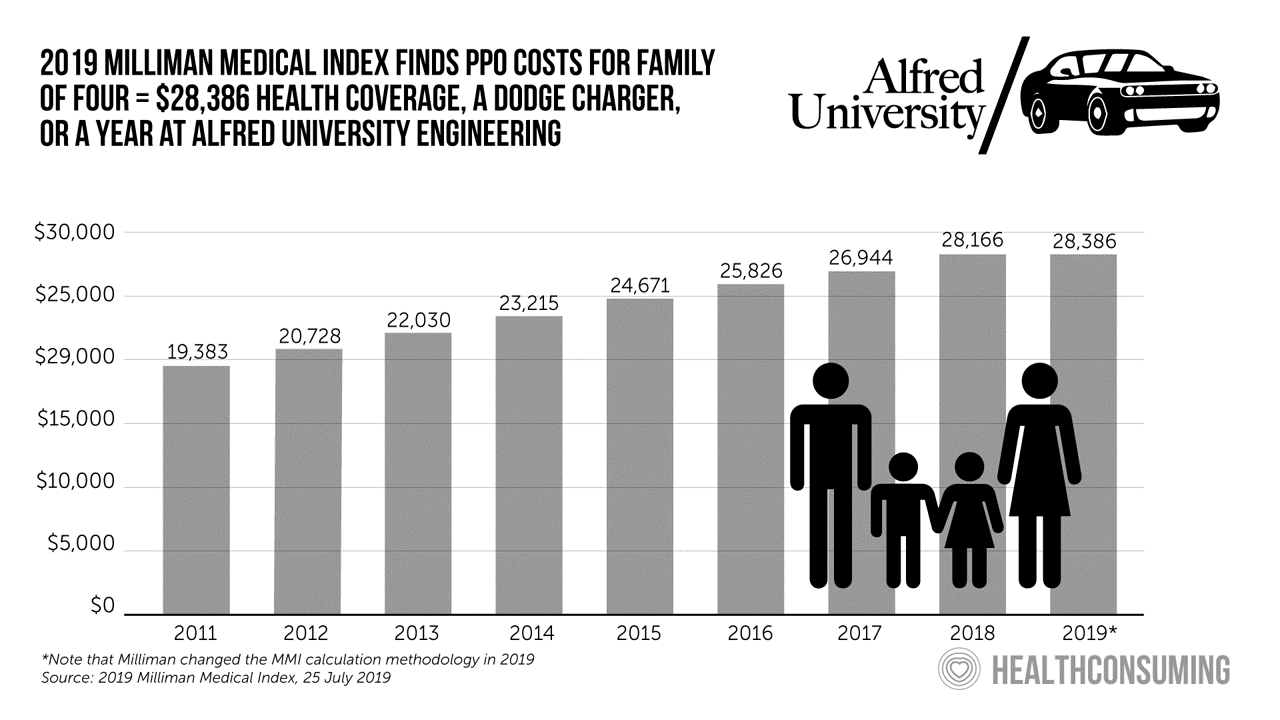
This year, an employer-sponsored PPO for a family of four in the U.S. will cost $28,386, a 3.6% increase over 2018, according to the 2019 Milliman Medical Index (MMI). Based on my annual read of this year’s Index, the PPO costs roughly the same as a new Dodge Charger or a year attending the engineering school at Alfred University. The Milliman MMI team has updated the methodology for the Index; the chart shown here is my own, recognizing that the calculations and assumptions beneath the 2019 data point differ from previous years. The key points of the report are that:
Finances Are the Top Cause of Stress, and HSAs Aren’t Helping So Much…Yet

If you heed the mass media headlines and President Trump’s tweets, the U.S. has achieved “the best economy” ever in mid-July 2019. But if you’re working full time in that economy, you tend to feel much less positive about your personal prospects and fiscal fitness. Nearly nine in 10 working Americans believe that medical costs will rise in the next few years as they pondering potential changes to the Affordable Care Act. The bottom line is that one-half of working people are more concerned about how they will save for future health care expenses. That’s the over-arching theme in PwC’s
Healthcare Costs Inspire Employer Activism and Employee Dissatisfaction – What PwC Found Behind the Numbers
In the U.S. each year between 2006 and 2016, employees’ healthcare cost sharing grew 4.5%. In that decade, Americans’ median wages rose 1.8% a year, PwC notes in their annual report, Medical cost trend: Behind the numbers 2020 from the firm’s Health Research Institute. Medical cost trend is the projected percent growth in healthcare costs over a year based on an equivalent benefit package from one year to the next. As the first chart shows, trend will grow 6% from 2019 to 2020. This is an increase of 0.3 percentage points up from 5.7% for 2019, which was flat from
How Consumers Look At Social Determinants of Health for Cancer, Diabetes and Mental Health

Enlightened health/care industry and public policy stakeholders have begun to embrace and address social determinants of health. These are the inputs that bolster health beyond health care services: they include economic stability like job security and income level (and equity), education, and access to healthy food, food security, safe neighborhoods, social support, clean environments (water and air), and in my own update on SDoH factors, access to broadband connectivity. As physician leaders in the AMA, technology advocates from AMIA, and numerous health plans focus efforts on strengthening social determinants, what do people – consumers, patients, caregivers — think about these
The 3 A’s That Millennials Want From Healthcare: Affordability, Accessibility, Availability

With lower expectations of and satisfaction with health care, Millennials in America seek three things: available, accessible, and affordable services, research from the Transamerica Center for Health Studies has found. Far and away the top reason for not obtaining health insurance in 2018 was that it was simply too expensive, cited by 60% of Millennials. Following that, 26% of Millennials noted that paying the tax penalty plus personal medical expenses were, together, less expensive than available health options. While Millennials were least likely to visit a doctor’s office in the past year, they had the most likelihood of making a
A Dose of Optimism Is a Prescription for Financial Health, Says Frost Bank

People define their personal health and well-being broadly, well beyond physical health. Mental wellness, physical appearance, social connections, and financial wellness all add into our self-health definitions. Mind Over Money is a consumer study conducted by Frost Bank, working with FleischmanHillard, connecting the dots between optimism and financial health. The top-line of the study is that people who are optimists have roughly two-thirds fewer days of financial stress per year than pessimists. Put another way, pessimists stress about finances 62% of the year, shown in the first chart from the study. This translates into 62% of optimists having better financial
In the Modern Workplace, Workers Favor More Money, New Kinds of Benefits, and Purpose
Today, April 2nd, is National Employee Benefits Day. Who knew? To mark the occasion, I’m mining an important new report from MetLife, Thriving in the New Work-Life World, the company’s 17th annual U.S. employee benefit trends study with new data for 2019. For the research, MetLife interviewed 2,500 benefits decision makers and influencers of companies with at least two employees. 20% of the firms employed over 10,000 workers; 20%, 50 and fewer staff. Companies polled represented a broad range of industries: 11% in health care and social assistance, 10% in education, 9% manufacturing, 8% each retail and information technology, 7%
The Evolution of Self-Care for Consumers – Learning and Sharing at CHPA
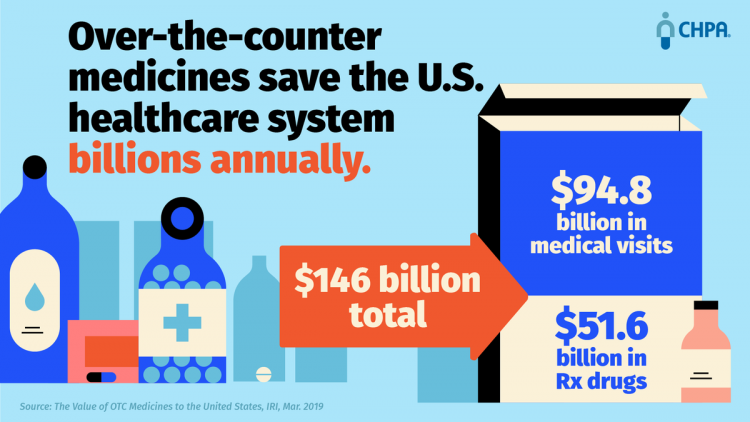
Self-care in health goes back thousands of years. Reading from Hippocrates’ Corpus about food and clean air’s role in health sounds contemporary today. And even in our most cynical moments, we can all hearken back to our grandmothers’ kitchen table wisdom for dealing with skin issues, the flu, and broken hearts. The annual conference of the Consumer Healthcare Products Association (CHPA) convened this week, and I was grateful to attend and speak on the evolving retail health landscape yesterday. Gary Downing, CEO of Clarion Brands and Chairman of the CHPA Board, kicked off the first day with a nostalgic look
Loving Wegmans and Amazon, Hating on the US Government: the Axios Harris Poll 100 in 2019

Americans love grocery stores, responsible retailers, technology and Amazon, Axios and Harris Poll found in this year’s top 100 visible company poll. The bottom five of the 100 include a big bank that ripped off consumers, a bankrupt retailer, a Big Tobacco company, and two organizations led by President Trump: The Trump Organization (#98) and the U.S. Government (#100). The summary points to five key findings in the report: The U.S. Government is the worst “company” in America according to “The Citizens of America,” in the words of Axios and Harris Poll. Americans have acquired “prime” tastes and expectations through
National Health Spending Will Reach Nearly 20% of U.S. GDP By 2027
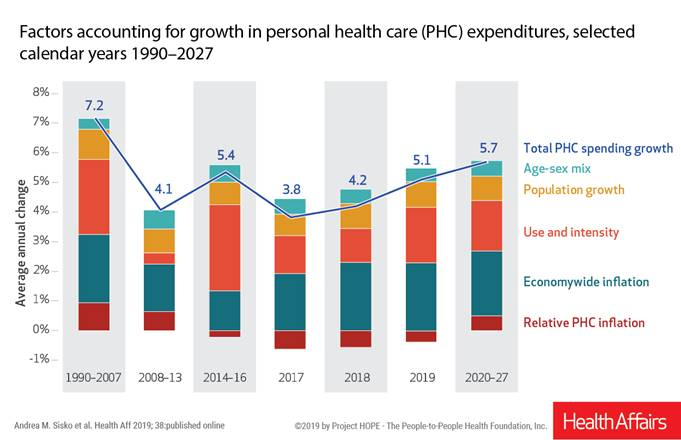
National health spending in the U.S. is expected to grow by 5.7% every year from 2020 to 2027, the actuaries at the Centers for Medicare and Medicaid Services forecast in their report, National Health Expenditure Projections, 2018-2927: Economic And Demographic Trends Drive Spending And Enrollment Growth, published yesterday by Health Affairs. For context, note that general price inflation in the U.S. was 1.6% for the 12 months ending January 2019 according to the U.S. Bureau of Labor Statistics. This growth rate for health care costs exceeds every period measured since the high of 7.2% recorded in 1990-2007. The bar chart illustrates the
“Telehealth is a digital distribution channel for health care” – catching up with Roy Schoenberg, President and CEO of American Well

Ten years ago, two brothers, physicians both, started up a telemedicine company called American Well. They launched their service first in Hawaii, where long distances and remote island living challenged the supply and demand sides of health care providers and patients alike. A decade later, I sat down for a “what’s new?” chat with Roy Schoenberg, American Well President and CEO. In full transparency, I enjoy and appreciate the opportunity to meet with Roy (or very occasionally Ido, the co-founding brother-other-half) every year at HIMSS and sometimes at CES. In our face-to-face brainstorm this week, we covered a wide range
Telehealth and Virtual Care Are Melting Into “Just” Health Care at HIMSS19

Just as we experienced “e-business” departments blurring into ecommerce and everyday business processes, so is “telehealth” morphing into, simply, health care delivery as one of many channels and platforms. Telehealth and virtual care are key education topics and exhibitor presences at HIMSS19. Several factors underpin the adoption of telehealth in 2019: Consumers’ demand for accessible, lower-cost health care services as people face greater financial responsibility for paying the medical bill (via high-deductible health plans and greater out-of-pocket costs for co-payments) Some consumers’ lacking or losing health insurance as ACA coverage eroded in the past two years, resulting in these patients
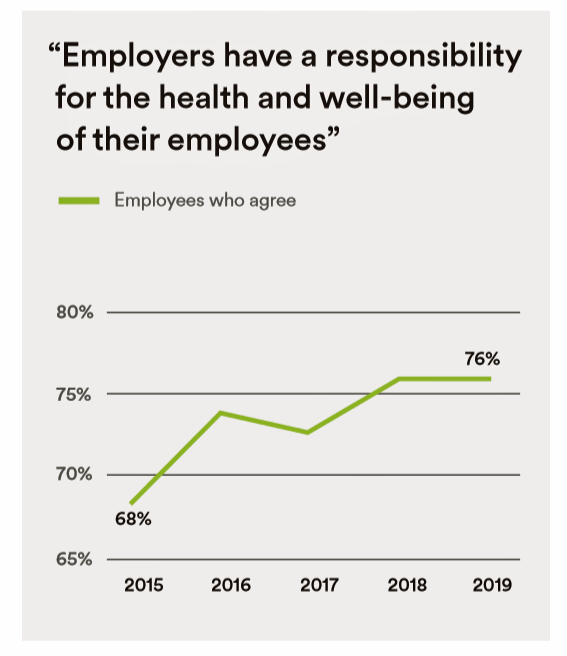
Trust in 2019 Via Edelman: The Plotline for Women and Healthcare
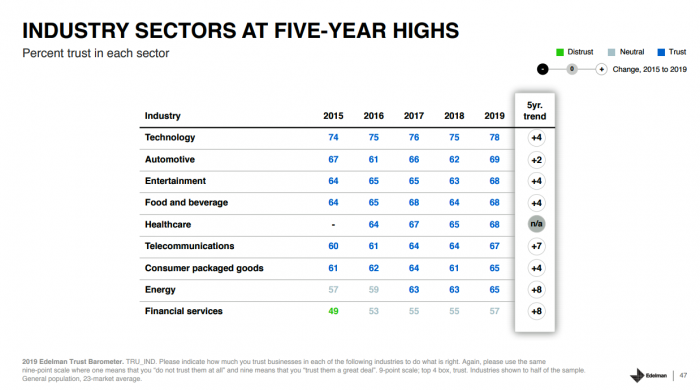
Fewer than one-half of consumers trust in government and media. Three-quarters trust employers, who in 2019 are the top-trusted institution according to the 2019 Edelman Trust Barometer released last week in Davos at the World Economic Forum. Consumers in the U.S. over-index for trust in employers, with 80% of people saying they have a strong relationship with “my employer,” compared with 73% of Britons, 66% of the French, and 59% of people in Japan. What’s underneath this is employers being trusted to provide certainty: most workers look to their employer to be a trustworthy source of information about social issues and
In U.S. Health Care, It’s Still the Prices, Stupid – But Transparency and Consumer Behavior Aren’t Working As Planned
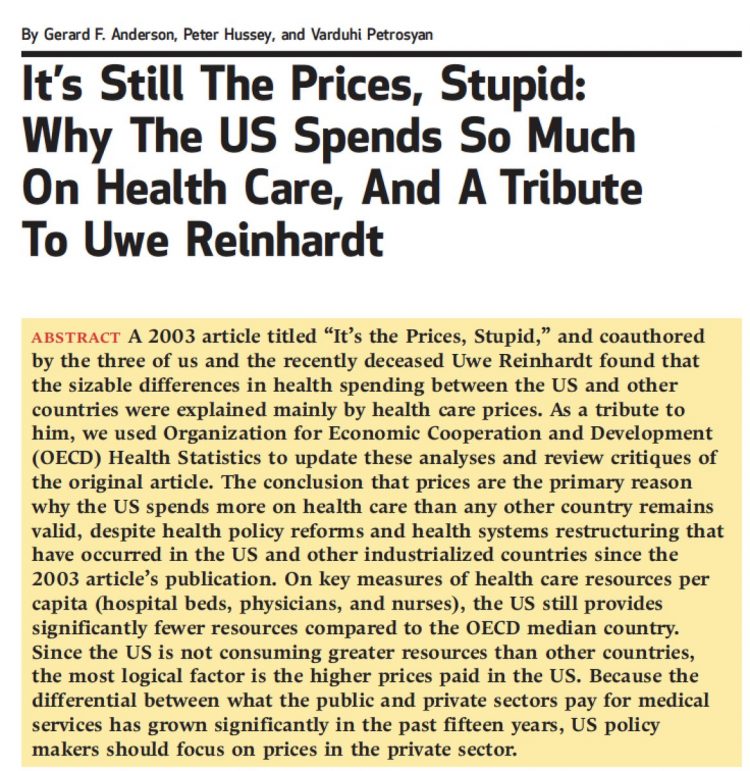
I’m glad to be getting back to health economic issues after spending the last couple of weeks firmly focused on consumers, digital health technologies and CES 2019. There’s a lot for me to address concerning health care costs based on news and research published over the past couple of weeks. We’ll start with the centerpiece that will provide the overall context for this post: that’s the ongoing research of Gerard Anderson and colleagues under the title, It’s Still The Prices, Stupid: Why The US Spends So Much On Health Care, And A Tribute To Uwe Reinhardt. It is bittersweet to
Costs, Consumerism, Cyber and Care, Everywhere – The 2019 Health Populi TrendCast

Today is Boxing Day and St. Stephens Day for people who celebrate Christmas, so I share this post as a holiday gift with well-wishes for you and those you love. The tea leaves have been brewing here at THINK-Health as we prepared our 2019 forecast at the convergence of consumers, health, and technology. Here’s our trend-weaving of 4 C’s for 2019: costs, consumerism, cyber and care, everywhere… Health care costs will continue to be a mainstream pocketbook issue for patients and caregivers, with consequences for payors, suppliers and ultimately, policymakers. Legislators inside the DC Beltway will be challenged by the




 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...