On This July 4th 2024, Let’s Remember the Doctors Who Have Helped Patients Declare Their Independence – Wisdom from Michael Millenson

“’A reform,’ wrote a 19th-century British parliamentarian, ‘is a correction of abuses. A revolution is a transfer of power. As we celebrate the American Revolution, catalyzed by men who broke ranks with their peers to overthrow a power structure that seemed immutable, let’s also celebrate those physicians who broke with their peers and declared independence for American patients.” So begins an informative, timely essay on participatory medicine and patient engagement researched and beautifully written by Michael Millenson, whom I am blessed to call both dear friend and professional colleague. Michael’s essay on the
Most Americans Follow an Eating Pattern in Search of Energy, Protein, and Well-Being – With Growing Financial Stress: A Food as Medicine Update
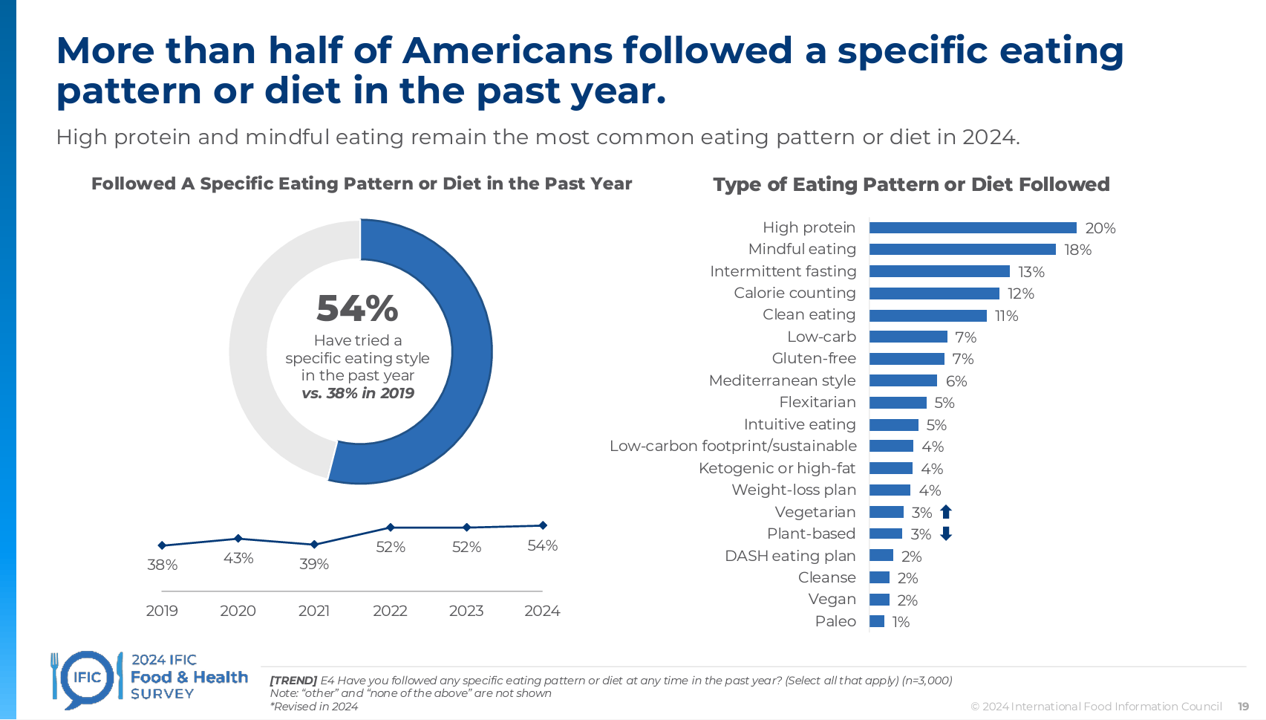
Most Americans follow some kind of eating regime, seeking energy, more protein, and healthy aging, according to the annual 2024 Food & Health Survey published this week by the International Food Information Council (IFIC). But a person’s household finances play a direct role in their ability to balance healthful food purchases and healthy eating, IFIC learned. In this 19th annual fielding of this research, IFIC explored 3,000 U.S. consumers’ perspectives on diet and nutrition, trusted sources for food information, and new insights into peoples’ views on the GLP-1 weight-loss drugs and the growing sense
How to Get Better Care to More People? Address Burnout, Bridge Insights with AI, Embed Sustainability – the Philips Future Health Index 2024

Health care access is a challenge in rural and urban areas, cities and suburbs, and across more demographic groups than you might realize, as we see wait times grow for appointments, primary care shortages, and delays in screening plaguing health systems around the world. In the Future Health Index 2024, Philips’ latest annual report presents a profile of the state of health care focused on how to provide better care for more people. For the report, Philips surveyed a total of 2,800 healthcare leaders consisting of 200 respondents in 14 countries: Australia, Brazil, China,
The Thematic Roadmap for AHIP 2024: What the Health Insurance Conference Will Cover

Health insurance plans make mainstream media news every week, whether coverage deals with the cost of a plan, the cost of out-of-network care, prior authorizations, or cybersecurity and ransomware attacks, among other front-page issues. This week, AHIP (the acronym for the industry association of America’s Health Insurance Plans) is convening in Las Vegas for its largest annual 2024 meeting. We expect at least 2,400 attendees registered for the meeting, and they’ll not just be representing the health insurance industry itself; folks will attend #AHIP2024 from other industry segments including pharmaceuticals, technology, hospitals and health systems, and the investment and financial services
Is There an Easy-Button for AI In Healthcare Team Well-Being? Exploring a New PC with Embedded AI

“The greatest opportunity offered by AI is not reducing errors or workloads, or even curing cancer: it is the opportunity to restore the precious and time-honored connection and trust,” Dr. Eric Topol wrote in his 2019 book, Deep Medicine: How Artificial Intelligence Can Make Healthcare Human Again. In the five years since Dr. Topol looked for AI to bolster the human-touch in health care, we’ve lived, worked, and muddled our way through the COVID-19 pandemic and witnessed the growing epidemic of burnout among clinicians, the front-line of medical care. I recalled Dr. Topol’s assertion on AI’s promise for humanizing health
The ROI on Patient Experience = Loyalty, Trust and Revenue – Listening to Accenture
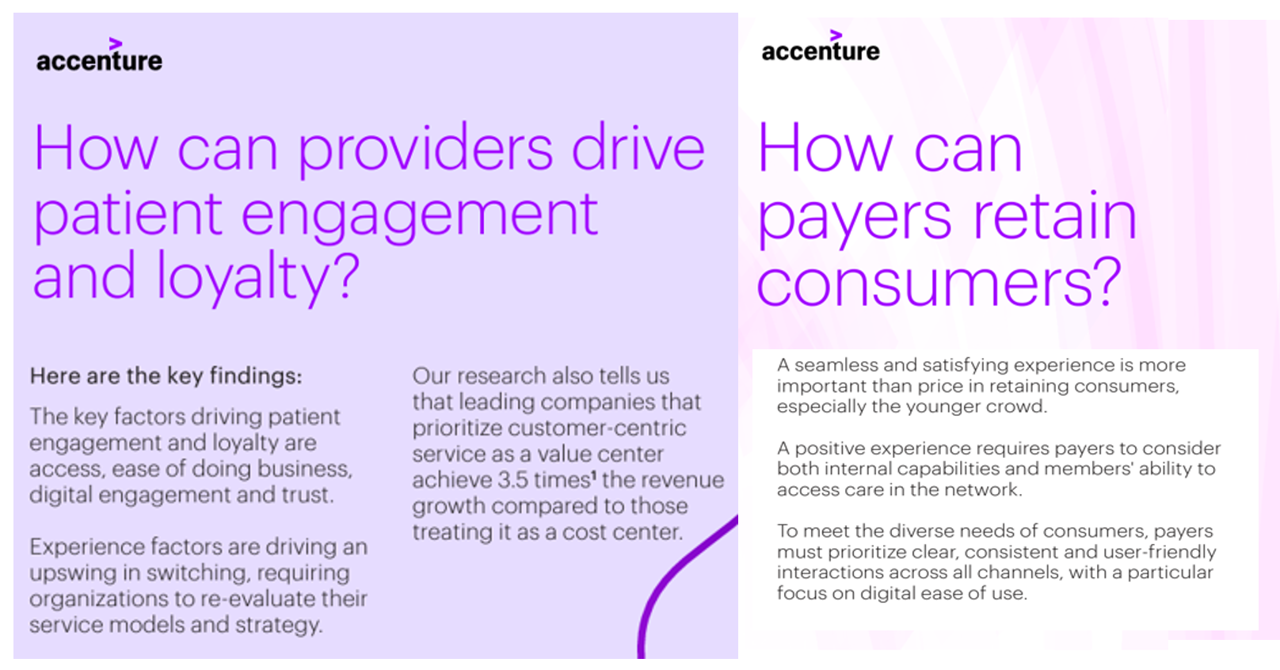
When health care providers and payers make patients’ lives easier, there’s a multiplying factor for loyalty and revenue growth, according to Accenture’s latest look into the value of experience in The Power of Trust: Unlocking patient loyalty in healthcare. Accenture conducted two surveys for this research, assessing nearly 16,000 U.S. adult consumers’ views on healthcare providers and health insurance plans. Several factors underpin patients’ selection of a new health care provider, especially: Access (70%), with a convenient location, quickly available appointments, digital/mobile/social interactions, and virtual care availability; and, The provider being a trusted source
Trust is a Superpower for Public Health – The 2024 Edelman Trust Barometer Through the Health Lens

Less than 50% of people living in 16 countries do not trust government, media, or NGOs to do what is right to address their health needs and concerns, based on the responses from over 15,000 people living in 16 countries whose opinions are captured in the 2024 Edelman Trust Barometer’s Special Report on Trust and Health. Edelman launched the 2024 Trust Barometer earlier this year during the Davos World Economic Forum, and today released this round of research focused on health. Globally (among health citizens in the 16 countries polled in the study), trust for
Healthcare 2030: Are We Consumers, CEOs, Health Citizens, or Castaways? 4 Scenarios On the Future of Health Care and Who We Are – Part 1
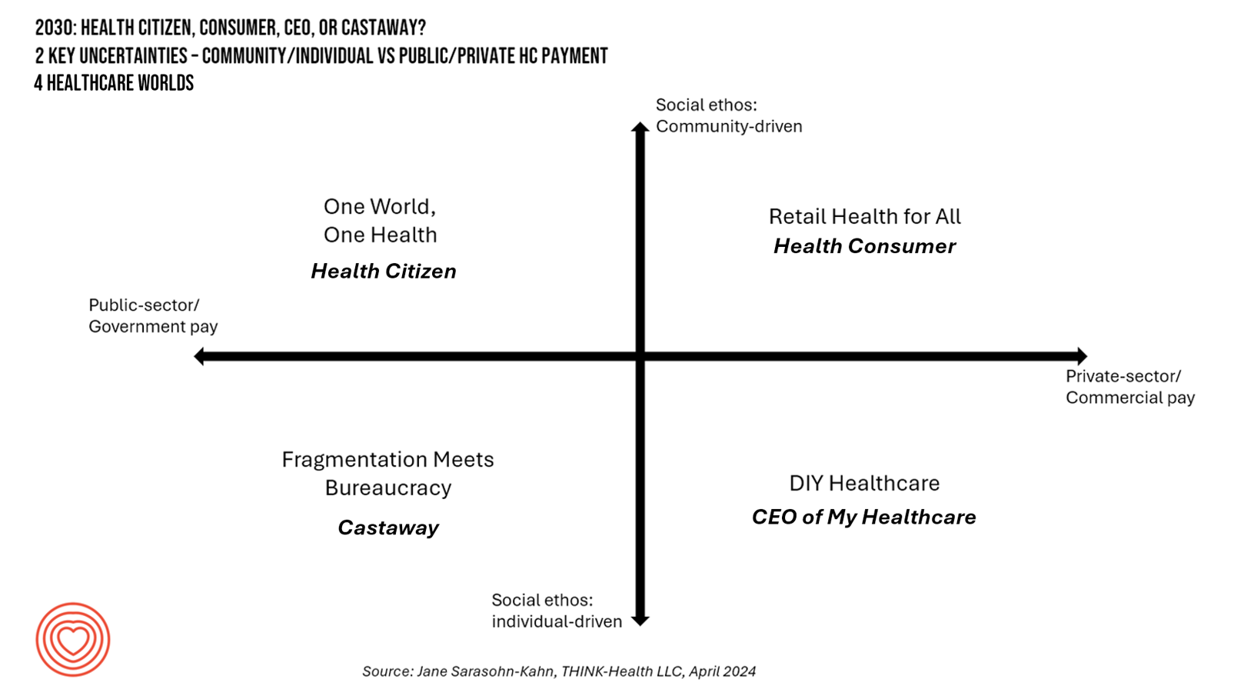
In the past few years, what event or innovation has had the metaphorical impact of hitting you upside the head and disrupted your best-laid plans in health care? A few such forces for me have been the COVID-19 pandemic, the emergence of Chat-GPT, and Russia’s invasion of Ukraine. That’s just three, and to be sure, there are several others that have compelled me to shift my mind-set about what I thought I knew-I-knew for my work with organizations spanning the health care ecosystem. I’m a long-time practitioner of scenario planning, thanks to the early education at the side of Ian
A Vote for Telehealth is a Vote for American Patients’ and Doctors’ Well-Being
Whether you’re a patient or a physician in the U.S., you’re burned out, tapped out, stressed out, timed out. While the 118th U.S. Congress can’t agree on much before the 2024 summer recess, there’s one bipartisan stroke of political pens in Washington, DC, that could provide some satisfaction for both patients and doctors: bring telehealth back to patients and providers permanently. Those pens would do two things to modernize American health care for both patients and doctors: first, Congress would pass the CONNECT for Health Act (HR 4189. S 2016) and second, re-introduce and sign the Telehealth Modernization Act.
While Virtual Care is “Table Stakes” in Health Care, Consumers Are Growing More Protective About Data-Sharing
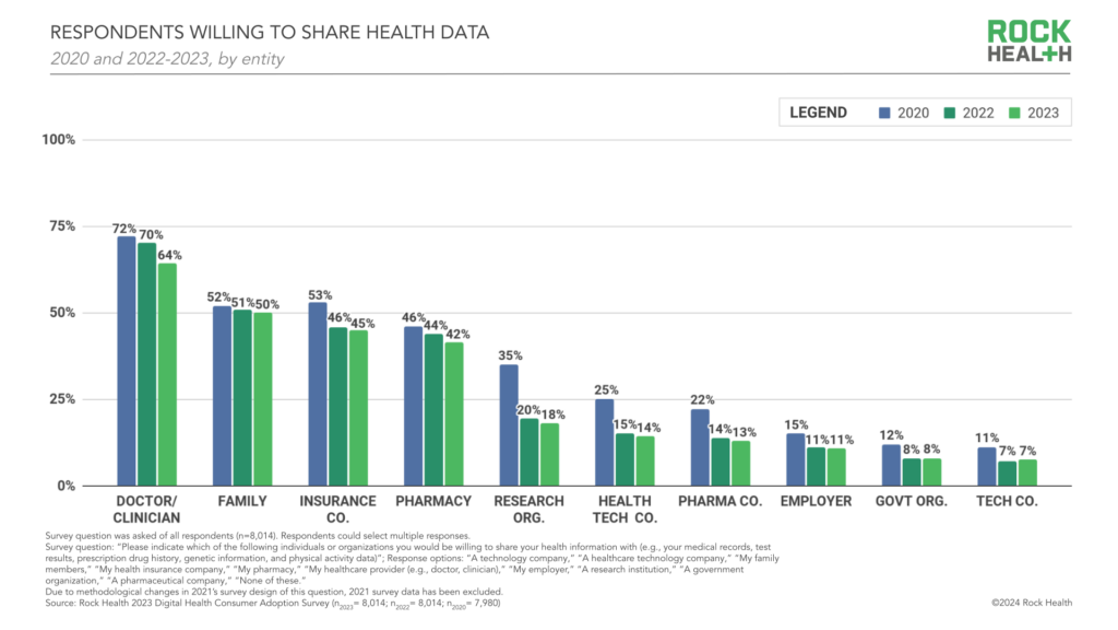
Three in four people in the U.S. have used virtual care, now, “Table-stakes…here to stay for patients and providers. However, that ubiquity comes with its own set of market pressures…shifting from pandemic-responsiveness to market- and consumer- responsiveness,” according to The new era of consumer engagement, Rock Health’s ninth annual Consumer Adoption Survey published 18 March. Convenience and waiting time are the top two reasons for choosing virtual over in-person care, Rock Health found. While virtual care is ubiquitous across the U.S. health care delivery landscape, patients-as-health care consumers are becoming more savvy and discriminating based
AI: Patients Included

“Clinical transformation with AI is easier without patients.” When Dr. Grace Cordovano heard this statement on a panel of physicians convening to share perspectives on the future of AI in health care held in early March 2024, the board-certified patient advocate felt, in her words, “insulted on behalf of the patient communities I know that are working tirelessly to advance AI that works for them.” “The healthcare ecosystem and policy landscape must formally recognize patients as end-users and co-creators of AI,” Cordovano wrote to me in an e-mail exchange. “Patients, their care partners, caregivers, and advocates are already utilizing AI
Physicians Feeling Burnout and Depression Continues in 2024 — The Annual View From Medscape
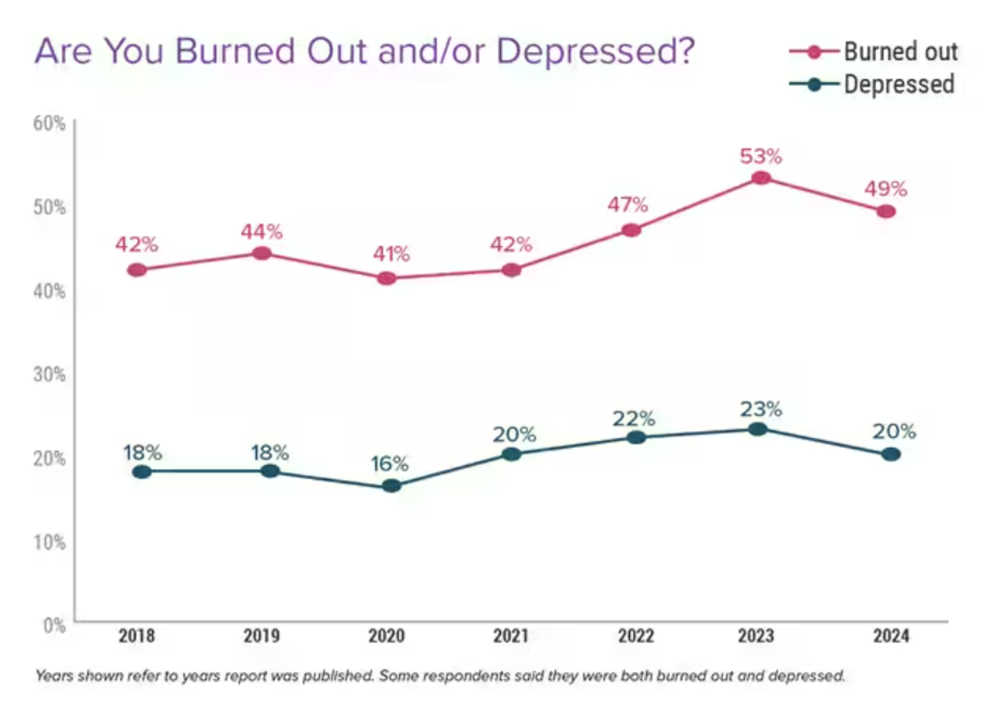
One-half of U.S. physicians report feeling burned out, and 3 in 5 of those doctors say they have felt burned out for over two years, according to the Physician Burnout & Depression Report for 2024 from Medscape. While the study’s press release asserts there may be “progress” given the percent of doctors citing burnout fell by 4 percentage points from 53% of doctors in 2022 to 49% in 2023, it is obvious the U.S. physicians need greater support and less taboo concerning their mental health which impacts both their professional and personal lives.
Nurses Continue to Rank Highest in Ethics and Honesty for Professions in the US — But Peoples’ Opinions for All Jobs, Including Nursing, Have Eroded in Gallup’s Latest Poll
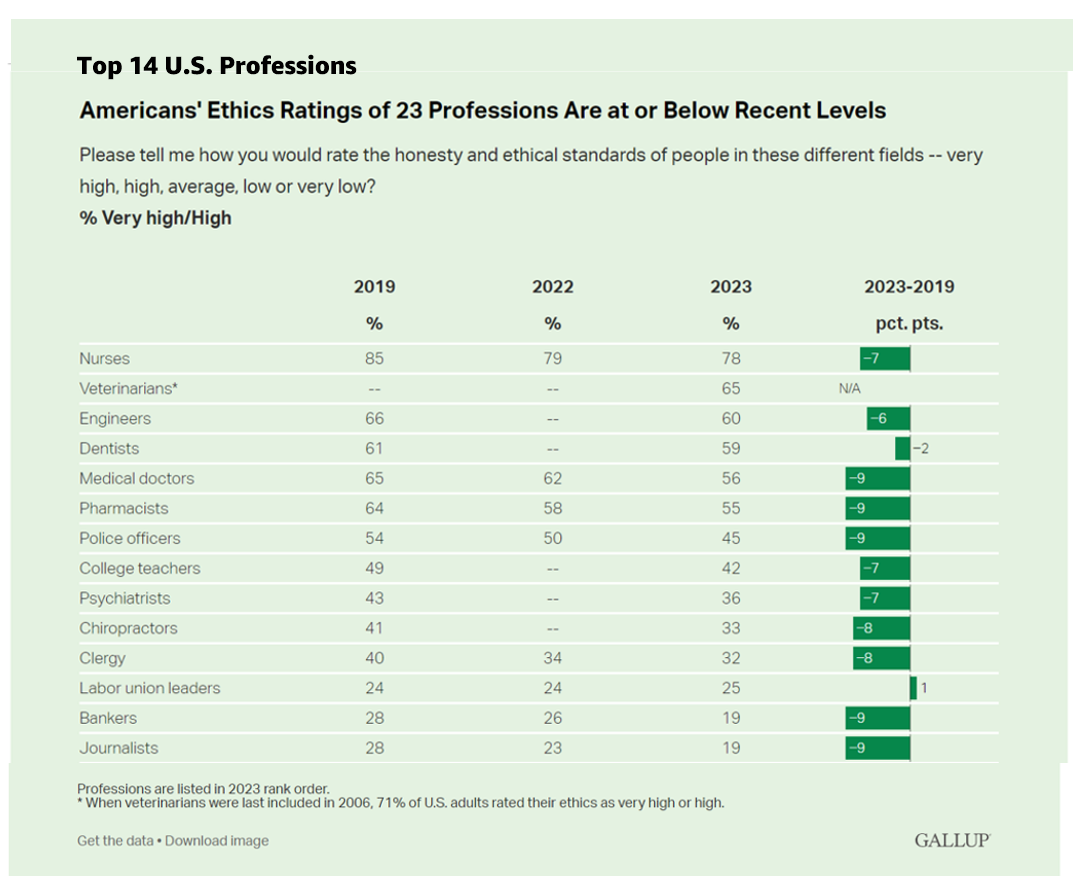
Ratings of honesty and ethics in professions have fallen down in the U.S., we find the Gallup Poll’s annual assessment of rankings for occupations that touch peoples’ lives in America. Each year for over a decade, nurses have ranked highest in this survey, representing the most-trusted profession working in America. However, even nurses’ ethic-equity has dropped in the hearts and minds of Americans over the past four years, falling 7 percentage points from a high of 85% of citizens ranking nurses at the greatest level of honesty and ethics to
Nurses Earn Highest Grade for Care Far Above All Other Health Care Workers — Including Doctors — In Latest Gallup Poll
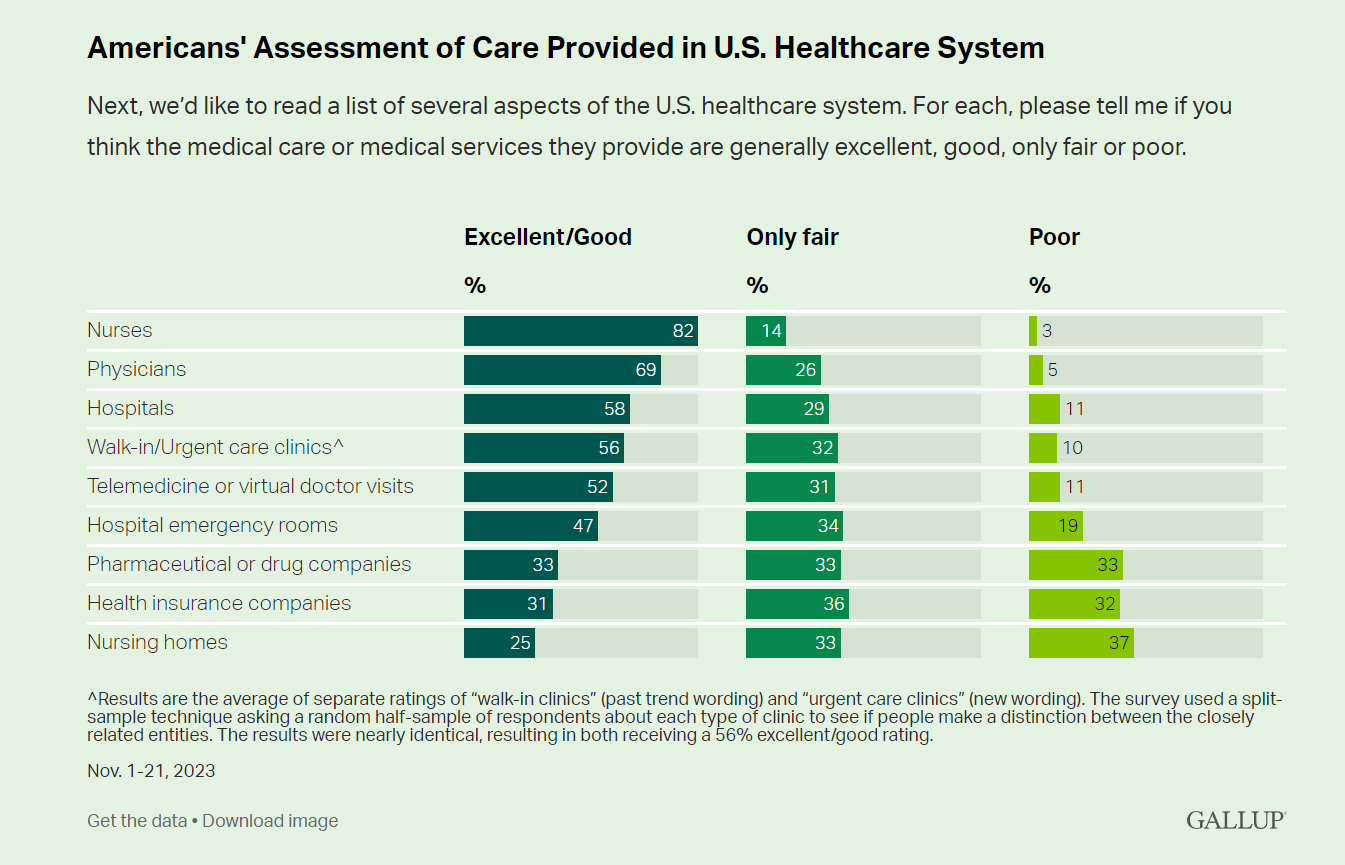
Nurses rank highest among various factors in the U.S. health system in the latest Gallup poll — earning a grade of “excellent” or “good” by American adults surveyed in November 2023. Further substantiation for nurses’ topping this poll of excellent care is that Gallup found historic low confidence in the U.S. health system among Americans earlier this year in a July study. Note that 8 in 10 consumers rate nurses excellent/good compared with 7 in 10 people ranking physicians this way, 6 in 10 for hospitals, 5 in 10 for telemedicine/virtual visits, and
“My Doctor’s Office” Should Accept Wearable Tech Health Data, Most Patients Say

“Do personal health trackers belong in the doctor’s office?” Software Advice wondered. “Yes,” the company’s latest consumer survey found, details of which are discussed in a report published on their website. Unique to this study is the patient sample polled: Software Advice surveyed 876 patients in September 2023 to gauge their perspectives on wearable tech and health. Note that the patient sample was limited to consumers who had seen a health care provider in the past two years and who also owned and used a personal wearable health device such as an Apple Watch or Fitbit. Thus, the responses shared
Cost Trumps Quality of Health Care for Consumers As Their Experience Has Eroded
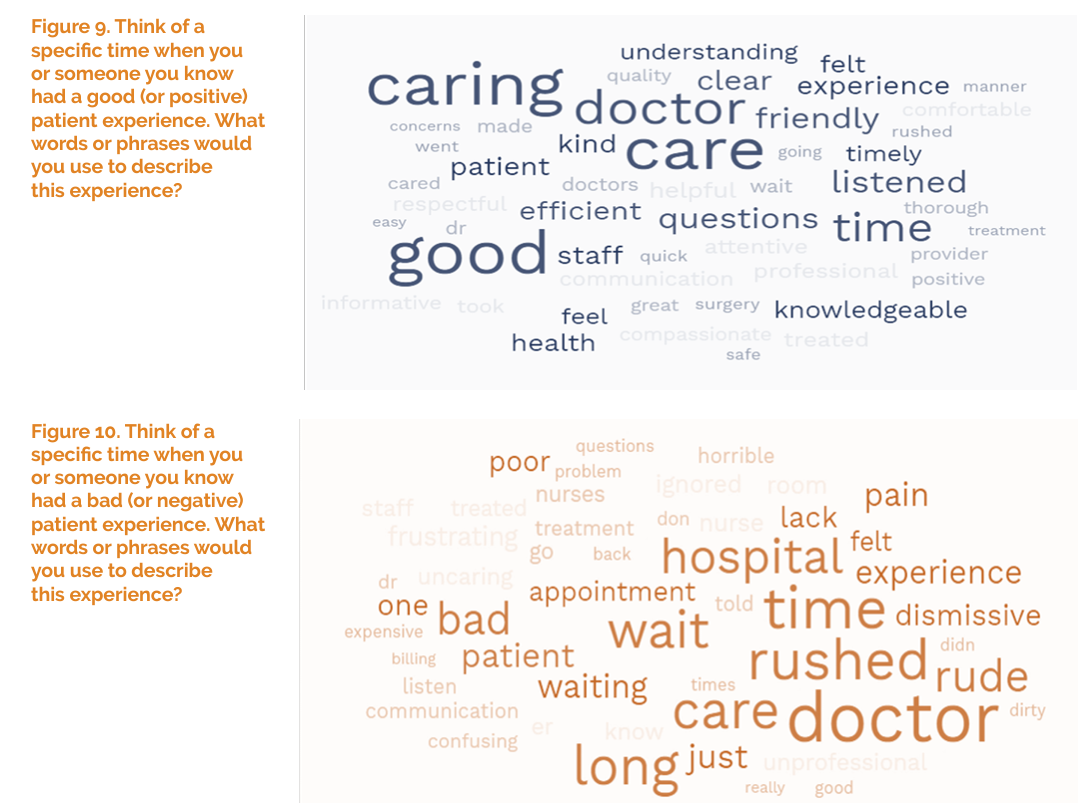
Patients’ perceptions of health care quality and experience have fallen in the three years since 2020, based on a July 2023 update from The Beryl Institute – Ipsos Px Pulse study. Start with health care quality, which 58% of U.S. adult patients ranked as “very good or good” in June 2020. The percent of health consumers evaluating their healthcare quality as very good or good fell to 41% of people in June 2023, an erosion of 17 percentage points, shown in the first chart. Next, consider patients’ ratings on their care experience,
To Avert a GLP-1 Cost Tsunami, Add Lifestyle Interventions: Learning from Virta Health
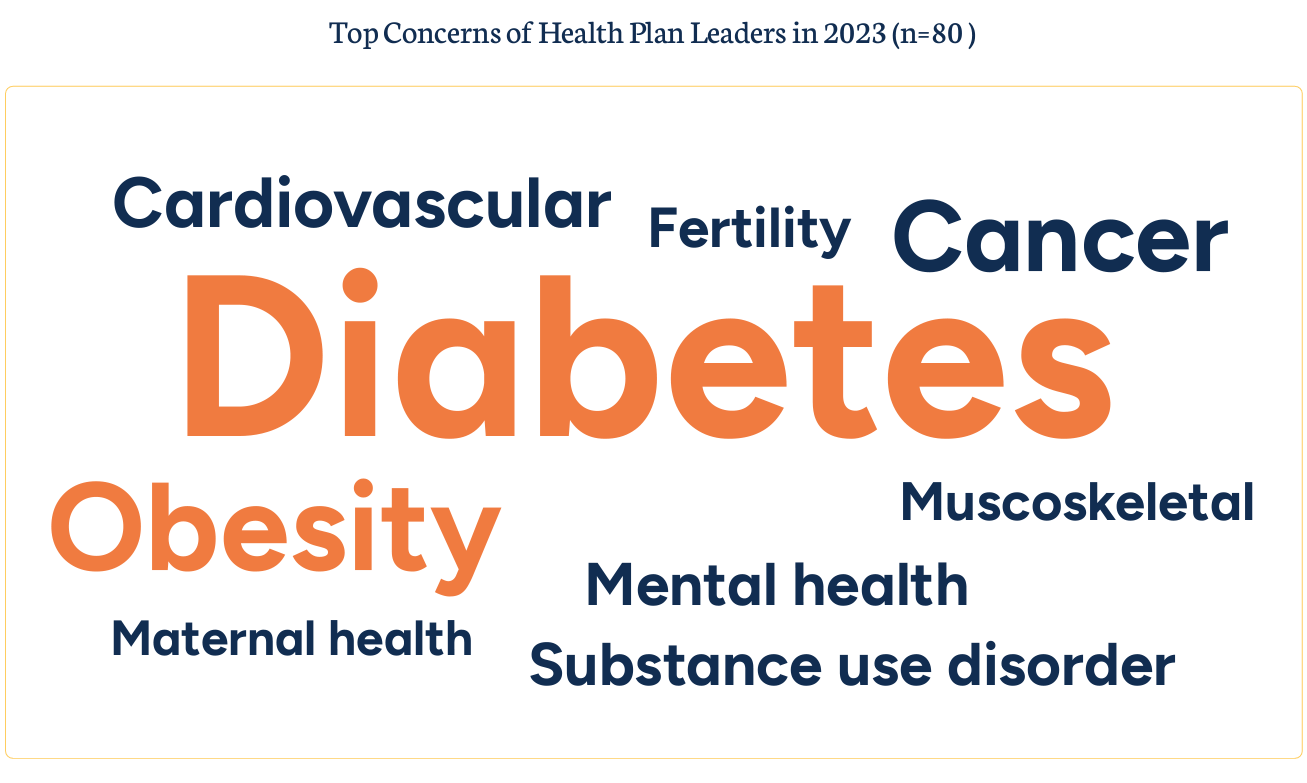
With consumer and prescriber interest in GLP-1 receptor agonist drugs “soaring,” health plan managers have a new source of financial stress and clinical questions on their to-do list. A team of Virta Health leaders held a webinar on 13th July 2023 to explain the results of a study the company just completed assessing health plan execs’ current views on Ozempic and other GLP-1 medicines with a view on both clinical outcomes and cost implications for this growing category of drugs that address diabetes and obesity. Indeed, diabetes and obesity are top health concerns among the
Patients, Nurses and Doctors Blame Health Insurers for Increasing Costs and Barriers to Care
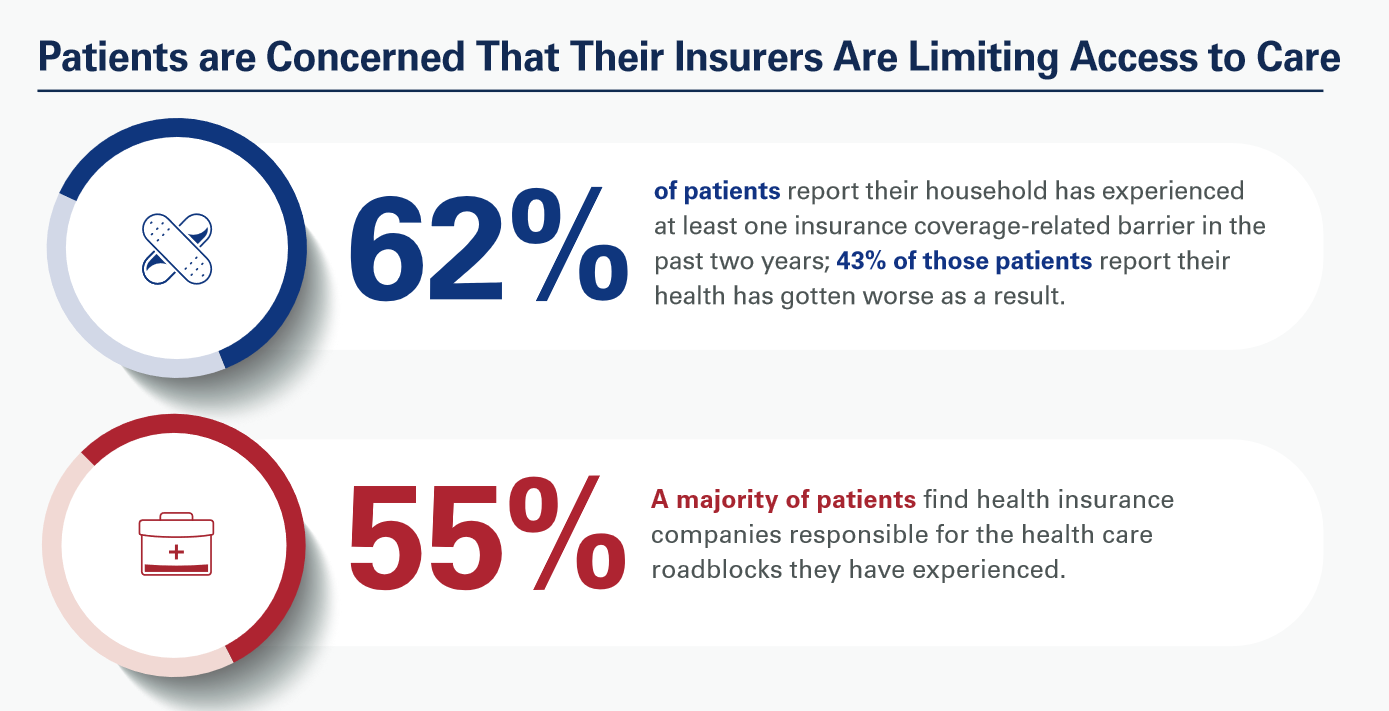
Most patients, nurses and doctors believe that health insurance plans reduce access to health care which contributes to clinician burnout and increases costs, based on three surveys conducted by Morning Consult for the American Hospital Association (AHA). Most patients have experienced at least one health insurance related barrier in the past two years, and 4 in 10 of those people said their health got worse as a result of that care-barrier. “These surveys bear out what we’ve heard for years — certain insurance companies’ policies and practices are reducing health care access and making
Retail Clinics’ Growing Role in Health Care and Prescription Drug Sales
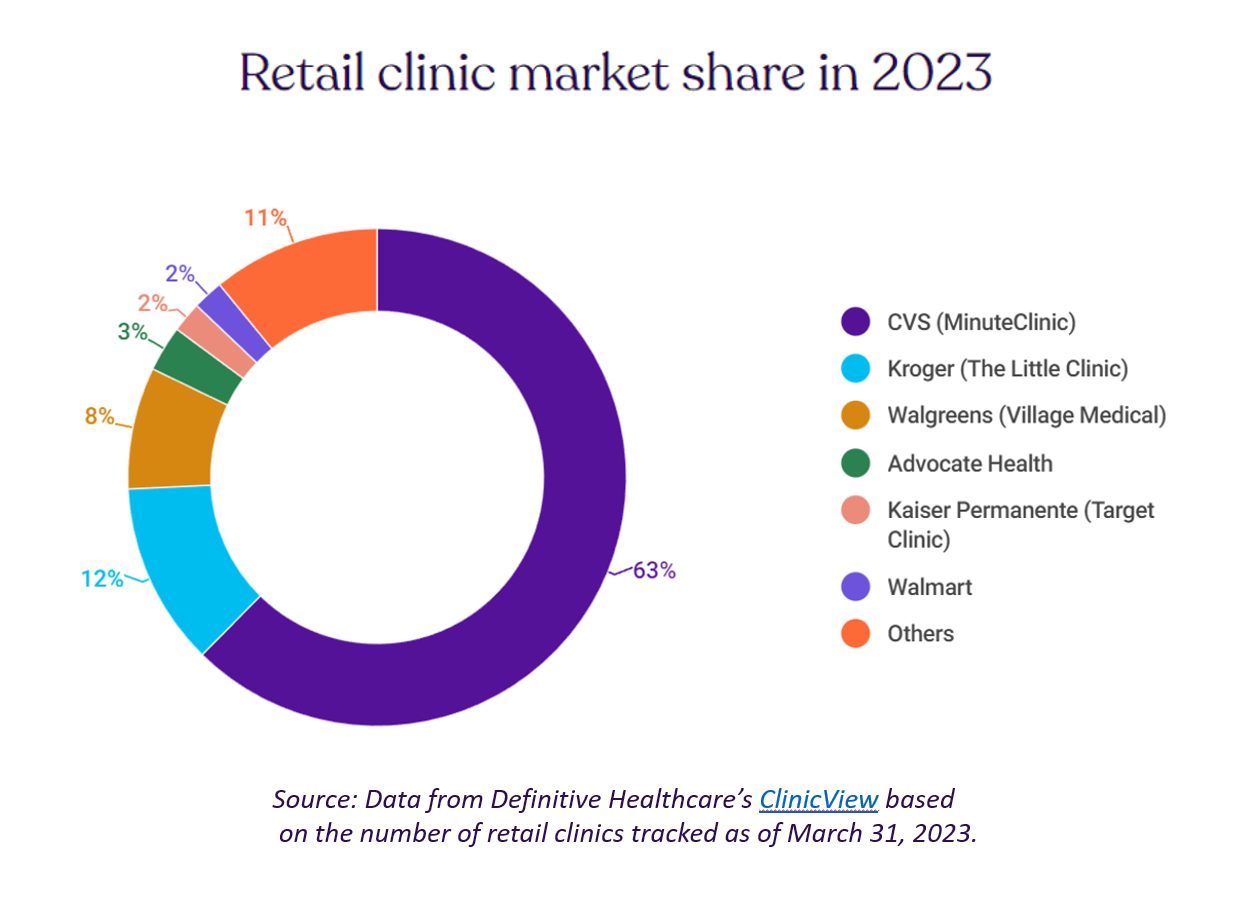
“It seemed like an odd pairing: shampoo and a throat swab,” observes a new report on the growth of retail health from Definitive Healthcare. But retail clinics are no longer, as the paper explains, “an experiment of a few grocery stores….they’re becoming a major force in the U.S. healthcare system,” asserts the thesis of Retailers in healthcare: A catalyst for provider evolution. While the use of emergency departments fell by 1% in the past five years, the use of retail clinics expanded by 70%, Definitive Healthcare calculated. Most retail clinics are owned by
Getting Health Care at a Retail Pharmacy vs a Retail Store: Consumers May Be Favoring the Pharmacist Versus the Retailer
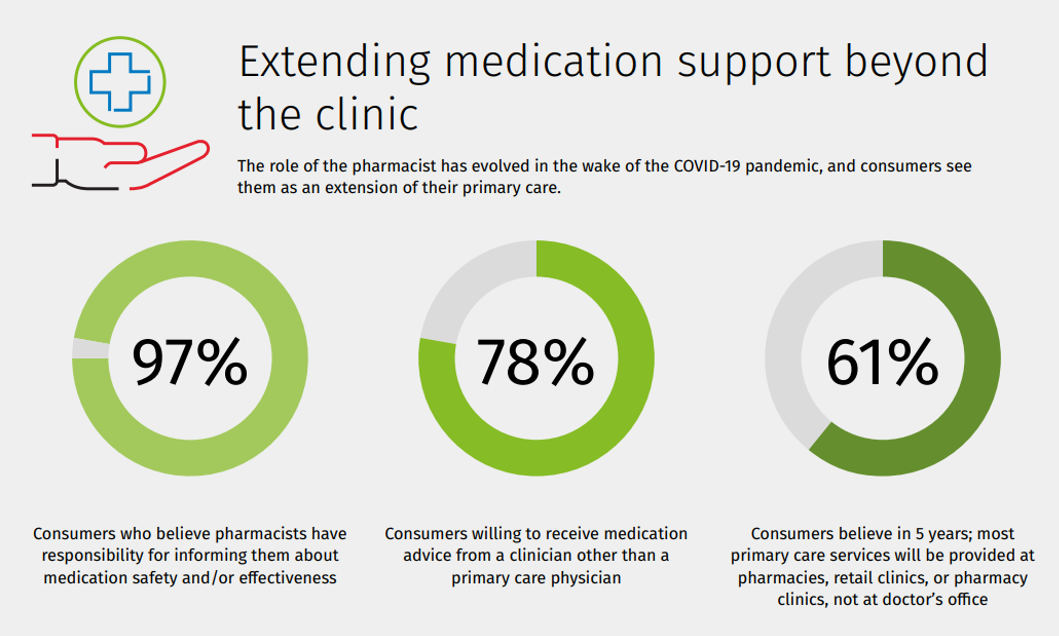
Not all “retail health” sites are created equal, U.S. consumers seem to be saying in a new study from Wolters Kluwer Health, the company’s second Pharmacy Next: Consumer Care and Cost Trends survey. Specifically, consumers have begun to differentiate between health care delivered at a retail pharmacy versus care offered at a retail store — such as Target or Walmart (both named as sites that offer “health clinics in department stores” in the study press release). While 58% of Americans were likely to visit a local pharmacy as a “first step” when faced with a non-emergency medical situation and 79%
Three More Signposts on the Road to Retail Health – Weight Loss Drugs, OTC Birth Control and Fashion-Meets-the-Flu
We continue to track to evolving, expanding landscape of retail health — which we see as the expanding ecosystem of health/care accessible to people-as-health consumers. This week, three intriguing examples are resonating with us: The ever-evolving weight-loss industry FDA favors OTC use for Perrigo’s Opill daily oral contraceptive birth control pill The convergence of fashion and health — specifically, how an over-the-counter medicine converges with clothing that helps us feel better. Let’s start with weight-loss, as several aspects of health/care come together in the consumer’s retail health sandbox. Dr. Eric Topol
“Your care, your way:” Learning from the Philips Future Health Index 2023
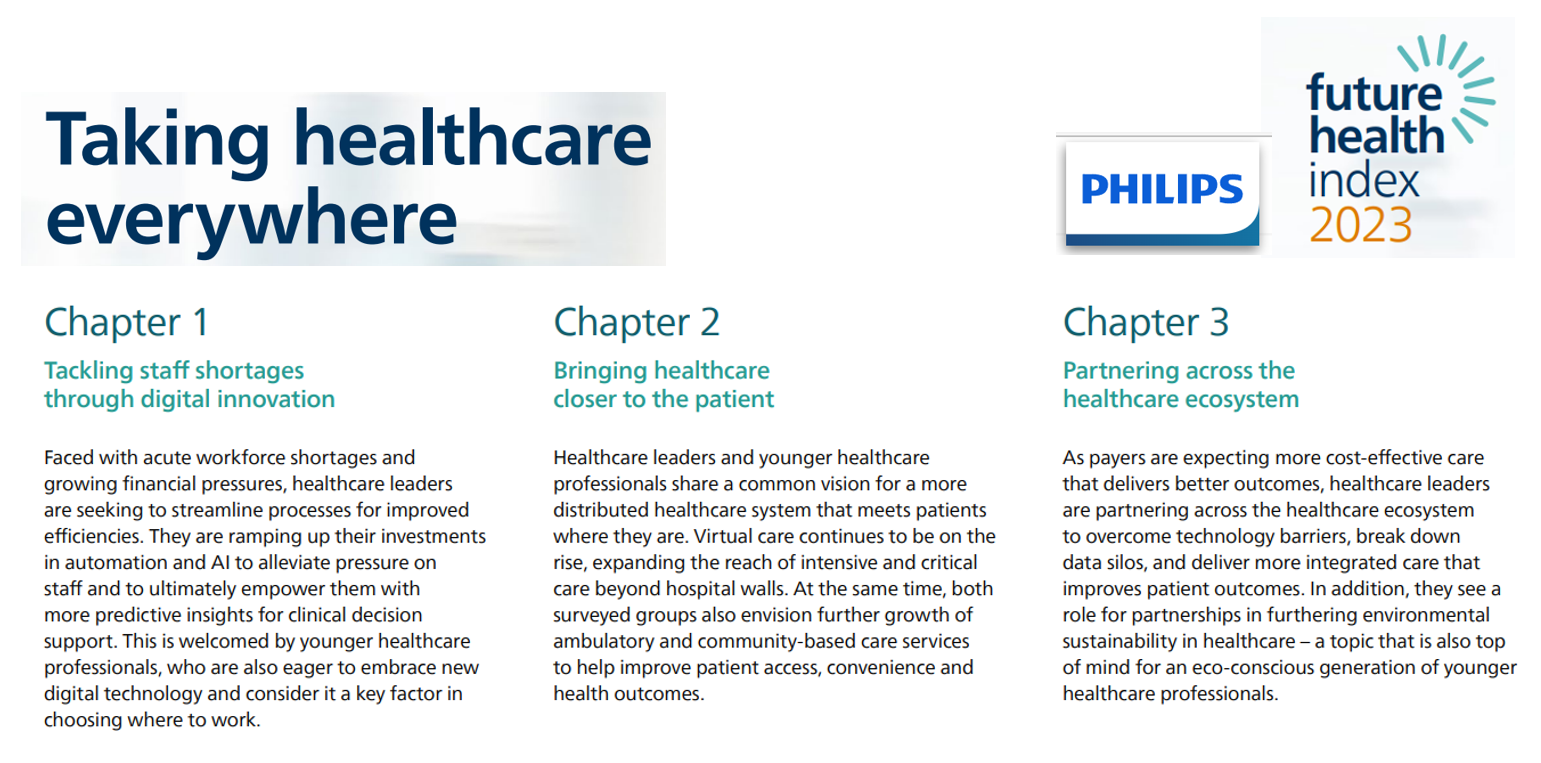
Consider the key drivers of supply and demand in health care, globally, right now: On the medical delivery supply side, the shortage of staff is a limiting factor to continuing to deliver care based on the usual work-flows and payment models. On the demand side, patients are taking on more demanding roles as consumers with high expectations for service, convenience, and safe care delivered closer to home — or at home. This dynamic informs The Future Health Index 2023 report from Philips, launched this week at HIMSS 2023. This is the eighth annual global FHI report, with detailed country-specific analyses to
Medscape Diagnoses Worsening Burnout and Depression Among U.S. Physicians
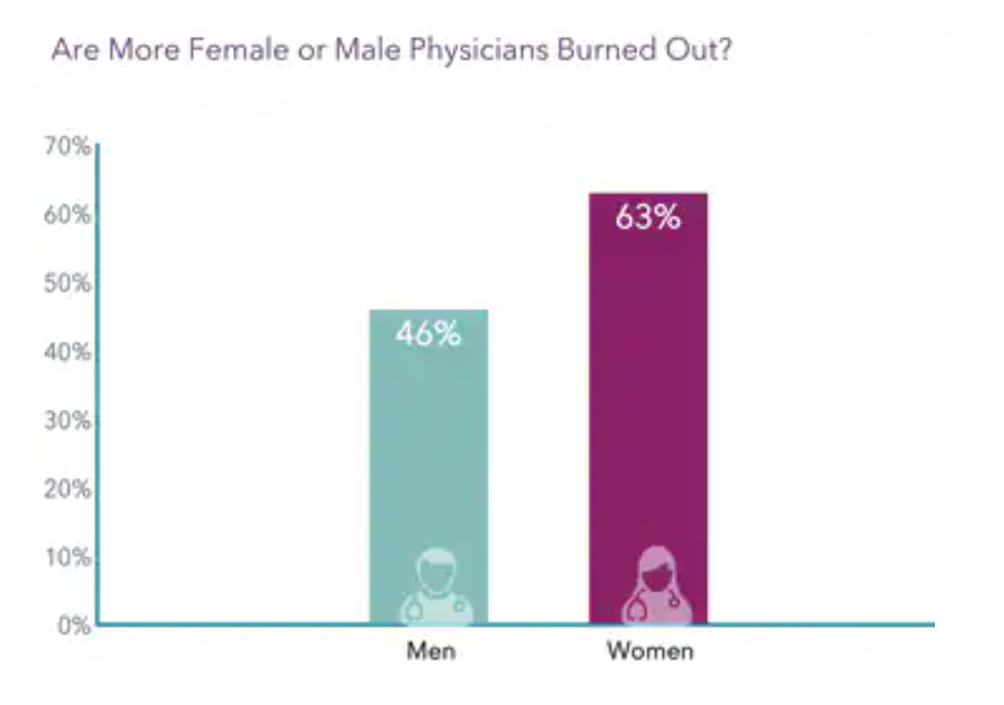
In the organization’s annual study into physicians’ wellbeing, Medscape has diagnosed worsening burnout and depression among America’s doctors. Over one-half of U.S. physicians say they are burned out or depressed, the chart from the U.S. Physician Burnout & Depression Report for 2023 calls out. “I cry but not one cares,” is one of the represented color comments provided by one of the physicians included in the survey of 9,175 physicians polled online between June and October 2022. The study covered 29 specialties, finding most burned out physicians worked in emergency medicine (65% saying
While Nurses and Doctors Still Rank Highest in Trust, Gallup Finds Trust-Erosion by Party ID
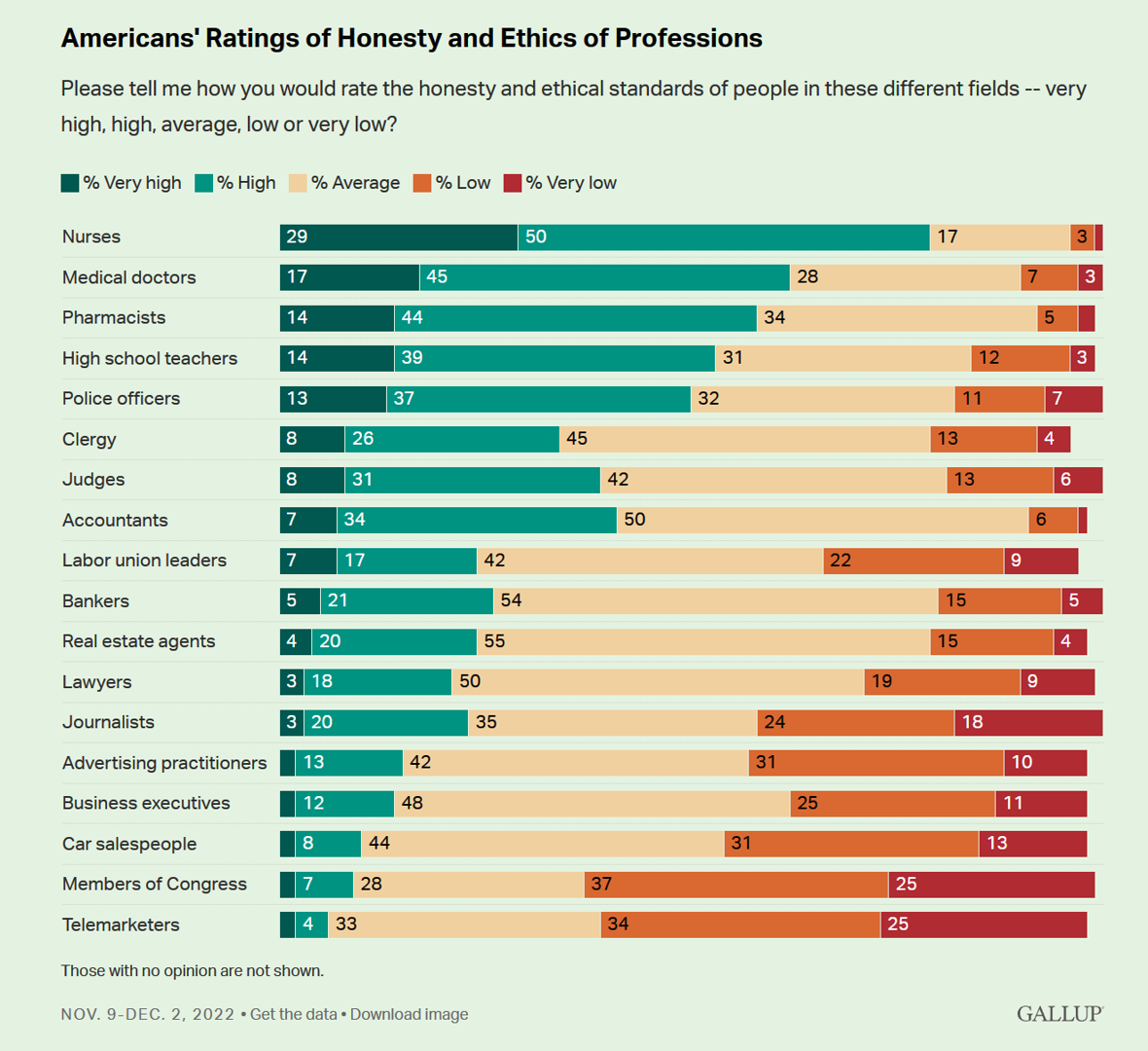
In the annual 2023 Gallup poll on honesty and ethics in professions in the U.S., the good news for the human capital of health care is that nurses, physicians and pharmacists continue to lead Americans’ ratings across professions in first, second, and third place respectively. The bummer is that that trust equity has eroded in the past year — especially among health citizens who identify as Republican voters. Start with the upside, which is the perennial Gallup finding that health care’s front-line workers are the most-trusted professions in the U.S. And
When Household Economics Blur with Health, Technology and Trust – Health Populi’s 2023 TrendCast

People are sick of being sick, the New York Times tells us. “Which virus is it?” the title of the article updating the winter 2022-23 sick-season asked. Entering 2023, U.S. health citizens face physical, financial, and mental health challenges of a syndemic, inflation, and stress – all of which will shape peoples’ demand side for health care and digital technology, and a supply side of providers challenged by tech-enabled organizations with design and data chops. Start with pandemic ennui The universal state of well-being among us mere humans is pandemic ennui: call it languishing (as opposed to flourishing), burnout, or
The Tik Tok’ing of Medical Mis-Information: Doctors’ and Patients’ Roles in Curating Healthy Advice
Doctors in the U.S. believe that the medical mis-information problem is worsening, learned in survey research from Merck Manuals. Doctors and patients, both, have roles to play in addressing medical misinformation online. Less than half of consumers, 44%, said that that there is more medical mis-information online than previously. That’s less than half of the percentage of doctors saying so — 98%, virtually all U.S. physicians, citing the problem. There were several disconnects noted in the Merck Manuals study showing starkly different perceptions of health information online between doctors and patients:
In Search of Clinical Effectiveness, But “Investment Exuberance?” Not So Much. Insights From FINN Partners and Galen Growth at HLTH 2022

While venture funding for digital health technology declined globally by 35% in the first three quarters of 2022 compared with 2021, this marks a “return to normal” based on the assessment in the Global State of Digital Health Report from FINN Partners and Galen Growth, published today and launched during the HLTH 2022 conference. The report analyzes data from over 12,000 digital health ventures tracked by Galen Growth’s HealthTech Alpha platform. The first chart illustrates the change in venture funding by therapeutic area, showing downturns in four of the five areas called
Thinking Value-Based Health Care at HLTH 2022 – A Call-to-Action
The cost of health insurance for a worker who buys into a health plan at work in 2022 reached $22,463 for their family. The average monthly mortgage payment was $1,759 in mid-2022. “When housing and health both rank as basic needs in Maslow’s hierarchy, what’s a health system to do?” I ask in an essay published today on Crossover Health’s website titled Value-Based Care: Driving a Social Contract of Trust and Health. The answer: embrace value-based care. Warren Buffett wrote Berkshire Hathaway shareholders in 2008, asserting that, “Price is what you pay. Value
Telehealth-As-Healthcare Is a Mainstream Expectation Among Consumers, J.D. Power Finds
Telehealth has increased access to mental health services, I’ve highlighted this Mental Illness Awareness Week here in Health Populi. But telehealth has also emerged as a preferred channel for routine health care services, we learn from J.D. Power’s 2022 Telehealth Satisfaction Study. Among people who had used virtual care in the past year, telehealth-as-healthcare is now part of mainstream Americans’ expectations as a normal part of their medical care. That’s because 9 in 10 users of telehealth in the U.S. would use virtual care to receive medical services in the future, J.D. Power found in
The Retail Health Battle Royale, Day 5 – Consumer Demands For a Health/Care Ecosystem (and What We Can Learn from Costco’s $1.50 Hot Dog)

In another factor to add into the retail health landscape, Dollar General (DG) the 80-year old retailer known for selling low-priced fast-moving consumer goods in peoples’ neighborhoods appointed a healthcare advisory panel this week. DG has been exploring its health-and-wellness offerings and has enlisted four physicians to advise the company’s strategy. One of the advisors, Dr. Von Nguyen, is the Clinical Lead of Public and Population Health at Google….tying back to yesterday’s post on Tech Giants in Healthcare. Just about one year ago, DG appointed the company’s first Chief Medical Officer, which I covered here in
The Retail Health Battle Royale in the U.S. – A Week-Long Brainstorm, Day 3 of 5 – Apple as “Intelligent Health Guardian”
Apple wants to be your “intelligent guardian for health,” based on a 60-page paper shepherded by Jeff Williams, the company’s Chief Operating Officer. Published last week, the paper is one of the big signals trumpeted this U.S. summer marked by the BA.5 omicron subvariant of SARS-CoV-2, inflation pressures on our household budgets, social/political tensions, and hot-hot weather. I’m folding the report into my coverage this week on the Retail Health Battle Royale today, Day 3 of my week-long series updating us on the health/care ecosystem. For the previous two days’ posts, see… Day 1
Healthcare access, racial disparities, guns and climate – U.S. doctors are worried about some big social issues
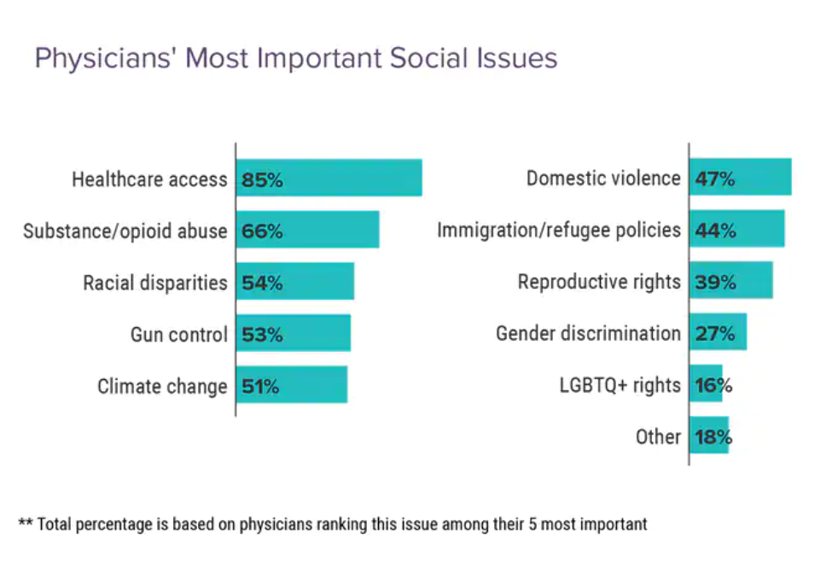
Doctors heads and hearts are jammed with concerns beyond curing patients’ medical conditions: U.S. physicians are worried about big social issues, according to a Medscape survey report, Physicians’ Views on Today’s Divisive Social Issues 2022. Topping physicians’ list of their top-five most important social issues, far above all others ranked healthcare access. Underneath that top-line statistic, it’s important to note that: 52% of doctors are “very concerned” about healthcare access, 28% are “concerned,” and 13% are “somewhat concerned.” Medscape underscores that in 2020, 31 million U.S. residents had no health insurance coverage, and
Health is Our Most Important Relationship: Inconvenient Truths from MRM/McCann Truth Central

We’ve hit a great “healthcare trust” recession around the world, translating into lower multiple points of medical ‘facts’ and pseudoscience, lower adherence to therapeutic regimens, and clinician burnout that has compromised medicine as the team sport it ideally should be. And that’s just one of five inconvenient truths unearthed in The Truth About Our Relationships with Health, the first in a series of papers that MRM is developing to, in their words, “look at the truths pr7eventing us from achieving a better relationship with our own health and with those along our health journey.” This report from MRM analyzes research
Primary Care in the U.S. – Still a Weak Backbone for the Health of Health Citizens
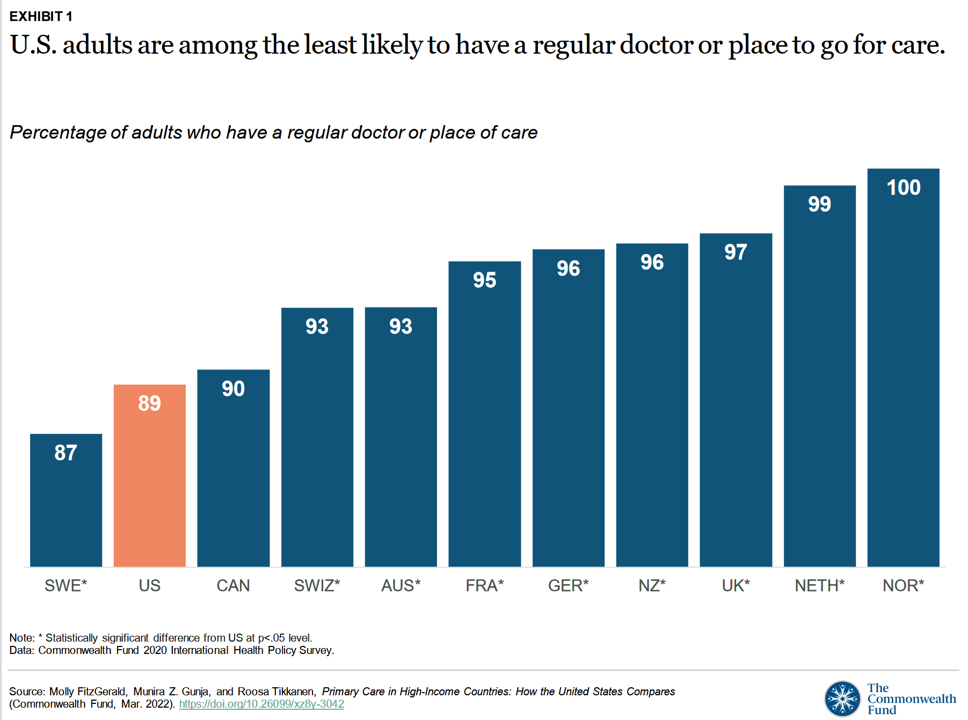
Compared with health citizens living in other wealthy countries, people living in the U.S. are still among the least likely to have a regular doctor or place to go for care. Thus, millions of Americans continue to lack access to primary care compared with peers in other nations, according to a report from The Commonwealth Fund. The Commonwealth Fund has tracked primary care access for many years, and over time has found the United States to lack the kind of primary care “backbone” that many wealthy nations have — whose health citizens also enjoy much better health outcomes that relate
Diagnosis: Stress, Anxiety and Anger – the 2022 Medscape Physician Burnout & Depression Report
As physicians deal on the frontlines in Year 3 of the COVID-19 pandemic, they’re stressed, anxious, and angry concludes the Medscape 2022 Physician Burnout & Depression Report. This year, the tagline focuses on stress, anxiety and anger. [Over the past couple of years, the study has used the word “suicide” in the title of the report, FYI]. Those reporting burnout are more likely women physicians than males (56% vs. 41%), work in the ER or critical care departments, and deal with too many bureaucratic tasks like charting and paperwork. For this annual look into the state of U.S. physicians mindsets
Nurses Continue to Rule in Honesty and Ethics in U.S. Professions – Healthcare Professions Still Top Gallup’s Annual Poll
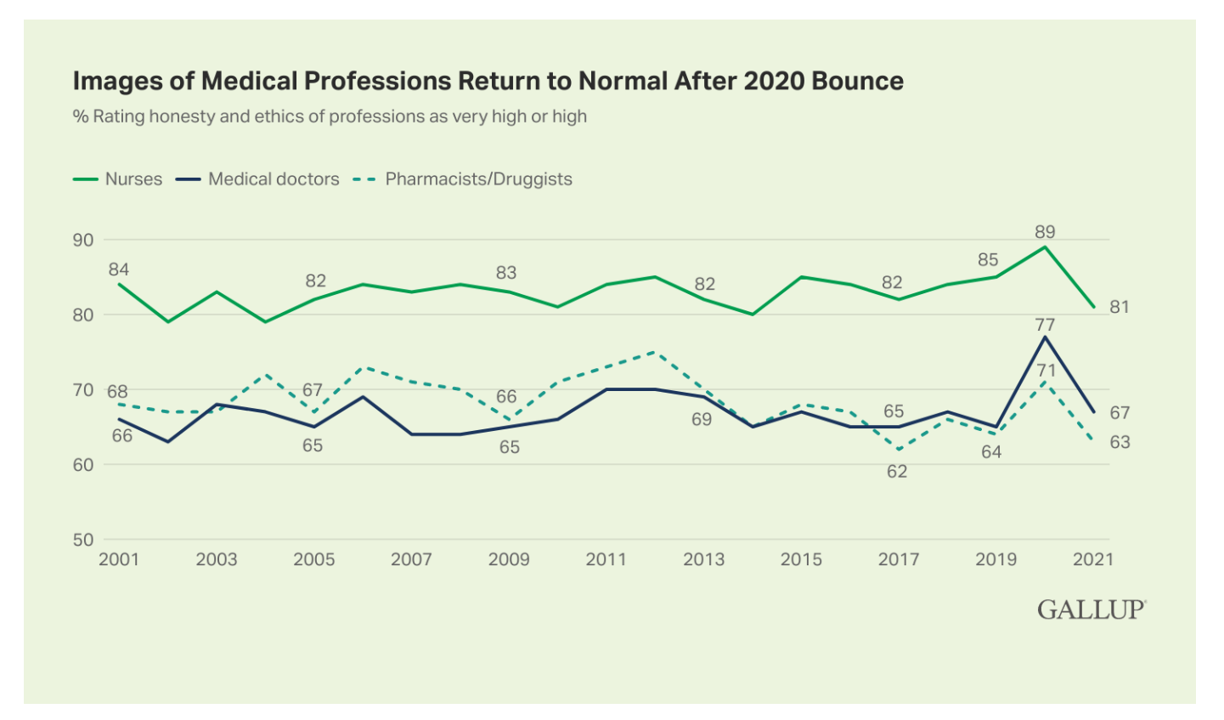
Three health care professions rank in the top four of the most honest and ethical rankings in Gallup’s annual poll on honesty and ethics in professions. And nurses are at the top of the list for the 20th year in a row. Grade-school teachers ranked third place between physicians and pharmacists, shown in the big chart of job types from most ethical to least. Perennially, the bottom-ranked posts are a mix of politicians (Members of Congress and lobbyists, state office holders), car salespeople, and the Mad Men and Women of advertising. Media professionals in TV and newspapers also polled relatively
Designing Digital Health for Public Health Preparedness and Equity: the Consumer Tech Association Doubles Down
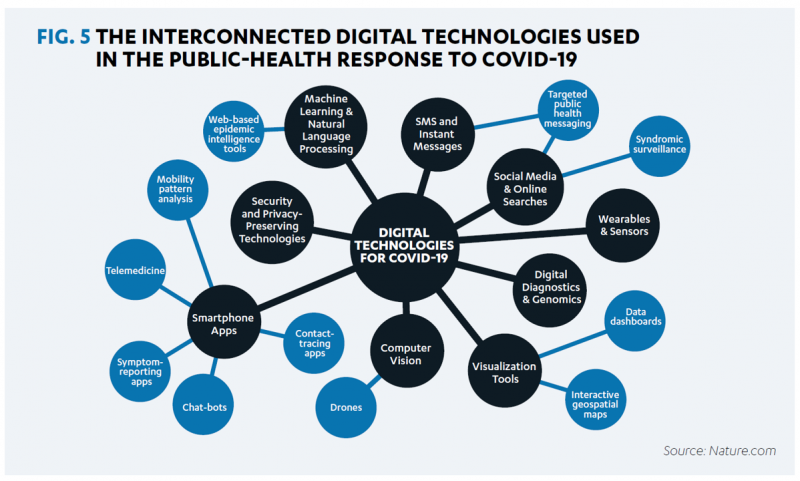
A coalition of health care providers, health plans, technology innovators, NGOs, and medical societies has come together as the Public Health Tech Initiative (PHTI), endorsed by the Consumer Technology Association (CTA) with the goal of advancing the use of trustworthy digital health to proactively meet the challenge of future public health emergencies….like pandemics. At the same time, CTA has published a paper on Advancing Health Equity Through Technology which complements and reinforces the PHTI announcement and objective. The paper that details the PHTI program, Using Heath Technology to Response to Public Health Emergencies, identifies the two focus areas: Digital health
Why CrossFit and 23andMe Are Moving from Health to Primary Care

As we see the medical and acute care sector moving toward health and wellness, there’s a sort of equal and opposite reaction moving from the other end of the continuum of health/care: that is, wellness and fitness companies blurring into health care. Let’s start with the news about CrossFit and 23andMe, then synthesize some key market forces that will help us anticipate more ecosystem change for 2022 and beyond. CrossFit announced the company’s launch of CrossFit Precision Care, described as primary care that provides personalized, data-driven services for “lifelong health,” according to the press release for the program. The service
Clinician Burnout in the Age of COVID
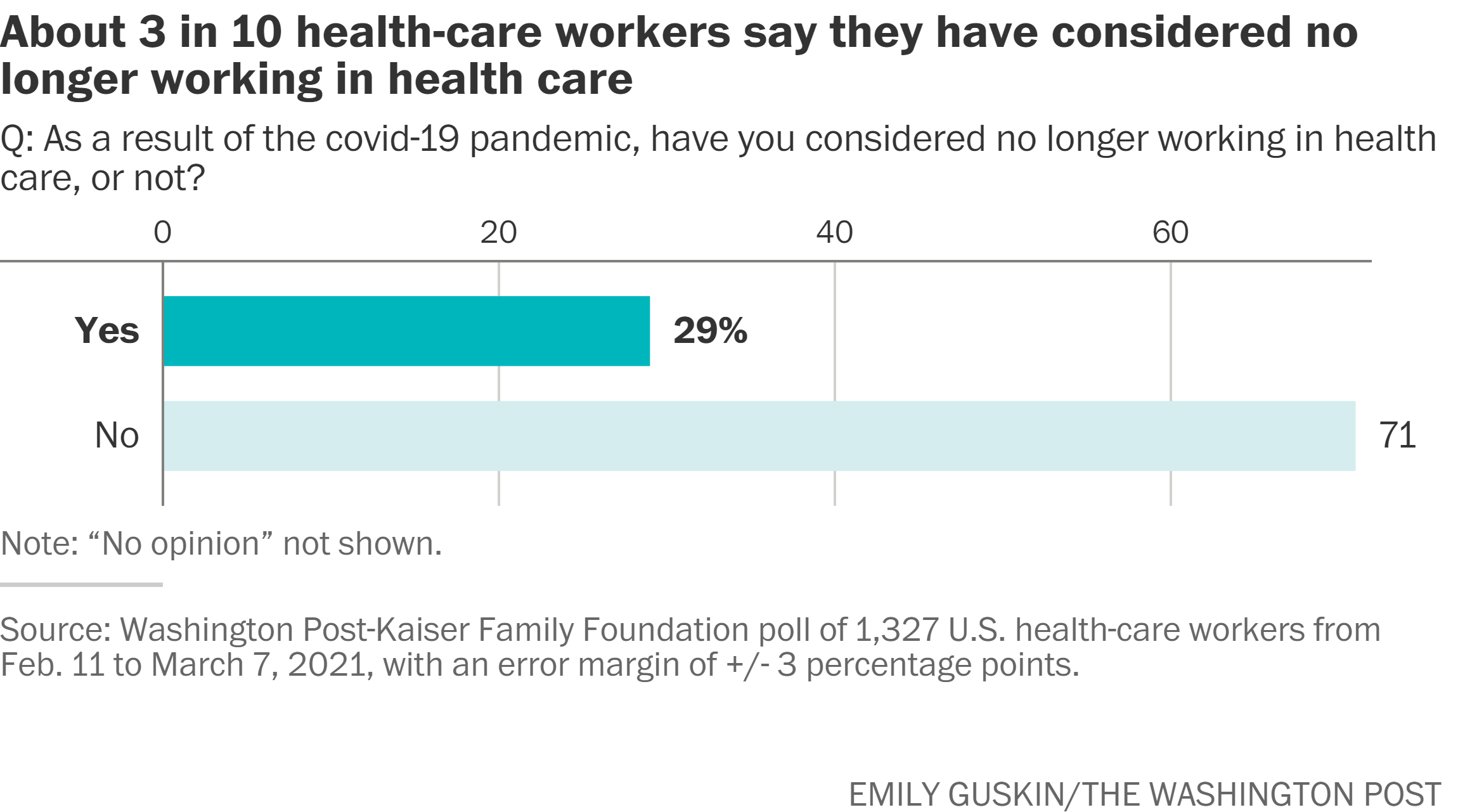
My latest essay for Medecision’s Liberation site digs into the sobering statistics on clinical burnout across the medical professions. From doctors to nurses, physician assistants and other licensed allied health human capital, our health care providers are in a world of hurt. This was initiated with the emergence of the COVID-19 pandemic. But the public health crisis, Delta variant, and lack of universal precautions adopted by U.S. health citizens have exacerbated an already-challenging scenario for individual clinicians and the organizations with whom they work and collaborate. But there’s an even bigger picture, and that’s the risk clinician burnout in its
Genentech’s Look Into the Mirror of Health Inequities

In 2020, Genentech launched its first study into health inequities. The company spelled out their rationale to undertake this research very clearly: “Through our work pursuing groundbreaking science and developing medicines for people with life-threatening diseases, we consistently witness an underrepresentation of non-white patients in clinical research. We have understood inequities and disproportionate enrollment in clinical trials existed, but nowhere could we find if patients of color had been directly asked: ‘why?’ So, we undertook a landmark study to elevate the perspectives of these medically disenfranchised individuals and reveal how this long-standing inequity impacts their relationships with the healthcare system
A Negative Outlook for US Hospital Margins Through 2021
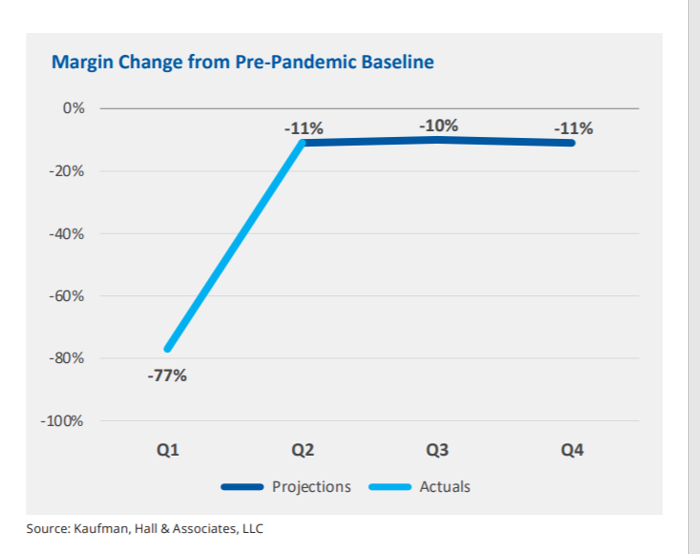
In the fourth quarter of 2021, U.S. hospital margins will still be lower than before the COVID-19 pandemic, Kaufman, Hall & Associates project in their latest read on hospital finances. Kaufman Hall has been monitoring hospitals’ financial health in the coronavirus era since March 2020, month-by-month. This new report looks into the Financial Effects of COVID-19: Hospital Outlook for the Remainder of 2021. This report was conducted on behalf of the American Hospital Association (AHA), who succinctly summarized the forecast saying, “COVID-19 [is] expected to drive continued hospital losses throughout 2021.” That projection is further couched in the concern that
Nurses and Aides Are Beloved and Deserve Higher Pay; and a Spotlight on the Filipinx Frontline
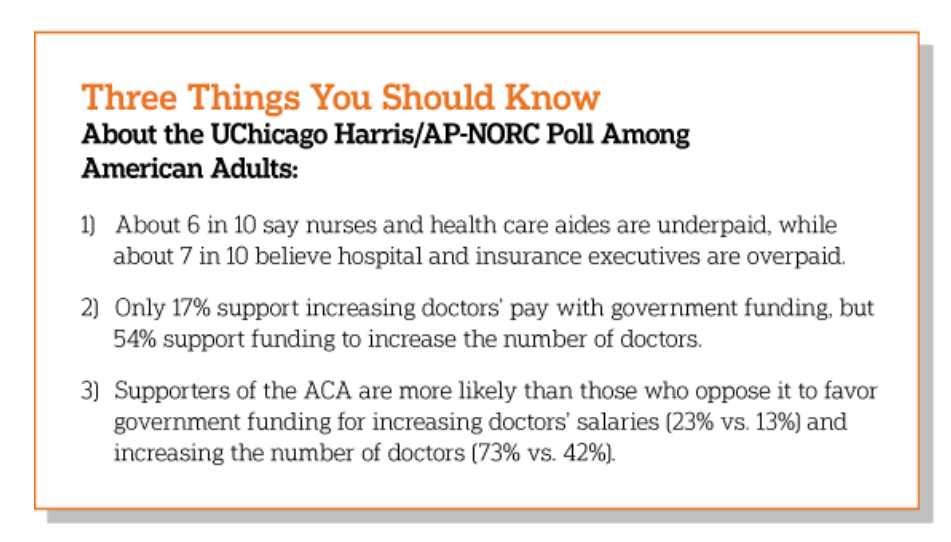
A majority of Democrats, Independents, and Republicans agree that nurses are underpaid. Most Americans across political parties also believe that hospital executives are overpaid, according to a poll from The Associated Press-NORC Center for Public Affairs Research. The survey analysis is aptly titled, Most Americans Agree That Nurses and Aides Are Underpaid, While Few Support Using Federal Dollars to Increase Pay for Doctors, . Insurance executives are also overpaid, according to 73% of Americans — an even higher percent of people than the 68% saying hospital execs make too much money. In addition to nurses being underpaid, 6 in 10
Pondering Prescription Drugs: Pricing Rx and Going Direct-to-Consumer
There is one health care public policy issue that unites U.S. voters across political party: that is the consumer-facing costs of prescription drugs. With the price of medicines in politicians’ and health citizens’ cross-hairs, the pharmaceutical and biotech industries have responded in many ways to the Rx pricing critiques from consumers (via, for example, Consumer Reports/Consumers Union and AARP), hospitals (through the American Hospital Association), and insurance companies (from AHIP, America’s Health Insurance Plans). The latest poll from the University of Chicago/Harris Public Policy and the Associate Press-NORC Center for Public Affairs Research quantifies the issue cross-party, finding that 74%
Our Pandemic Lessons: Listening to Michael Dowling – a #HIMSS21 Wrap-Up

“We don’t un-learn,” Dr. Amy Abernethy asserted as she shared her pandemic perspectives on a panel with 2 other former U.S. health policy and regulatory leaders. The three spoke about navigating compliance (think: regulations and reimbursement) in an uncertain world. An uncertain world is our workplace in the health/care ecosystem, globally, in this moment. So to give us some comfort in our collective foxhole, my last post for this week of immersion in #HIMSS21 is based on the keynote speech of Michael Dowling, CEO of Northwell Health. Dowling keynoted on the theme of “Leading for the Future,” sharing his lessons
Doctors’ Offices Morph into Bill Collectors As Patients Face Growing Out-Of-Pocket Costs
In the U.S., patients have assumed the role of health care payors with growing co-payments, coinsurance amounts, and deductibles pushing peoples’ out-of-pocket costs up. This has raised the importance of price transparency, which is based on the hypothesis that if patients had access to personally-relevant price/cost information from doctors and hospitals for medical services, and pharmacies and PBMs for prescription drugs, the patient would behave as a consumer and shop around. That hypothesis has not been well proven-out: even though more health care “sellers” on the supply side have begun to post price information for services, patients still haven’t donned
Healthy Living Trends Inspired by COVID-19: Retailers, Food, and Consumers’ Growing Self-Care Muscles
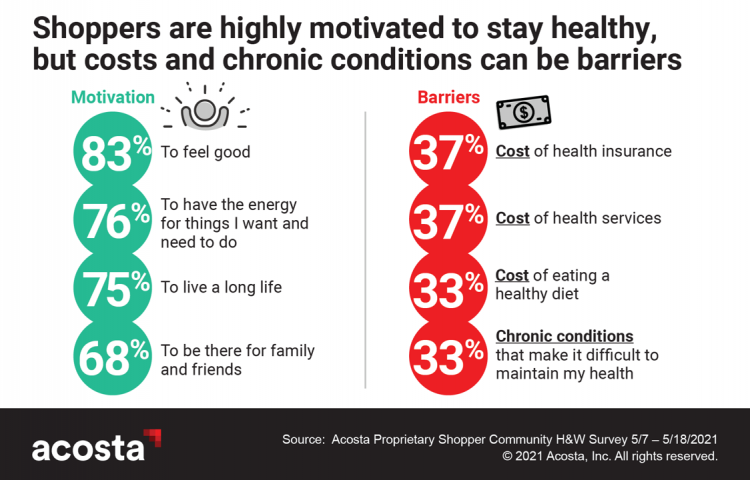
“Self-care” took on new meaning and personal work-flows for people living in and through the coronavirus pandemic in the U.S. Acosta, the retail market research pro’s, updated our understanding consumers evolving as COVID-19 Has Elevated the Health and Wellness Trends of the Recent Years, results of a survey conducted among in May 2021. In the U.S., consumers’ take on self-care has most to do with healthy eating and nutrition (for 1 in 2 people), getting regular medical checkups (for 42%), taking exercise, relaxing, using vitamins and supplements, and getting good sleep. Healthy relationships are an integral part of self-care for
Aging Populations of Consumers and Physicians Underpin the Future Doctor Shortage
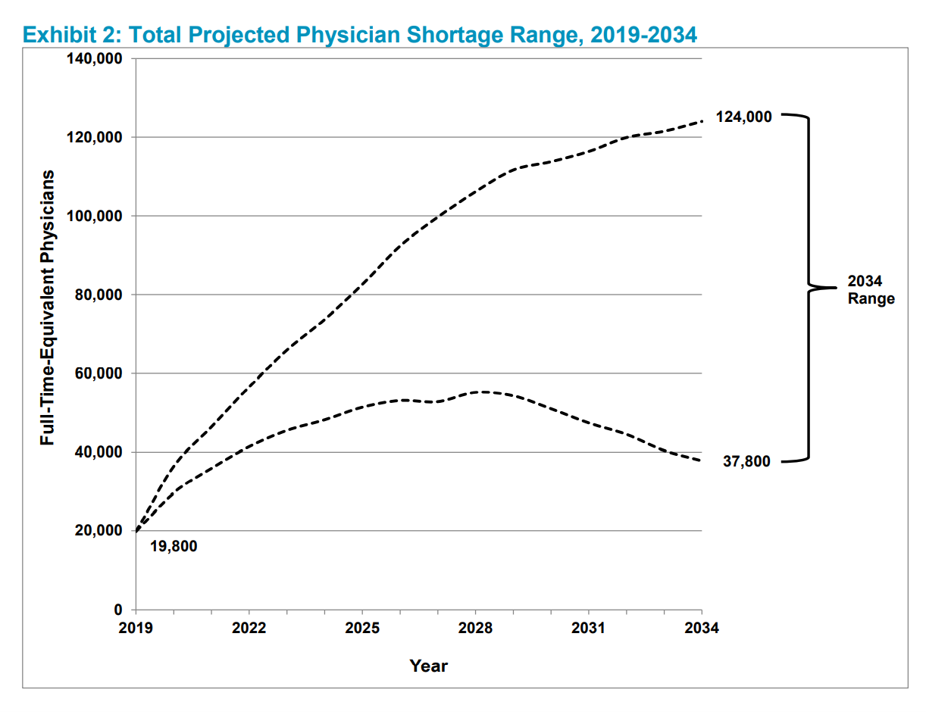
The U.S. will be short as many as 124,000 physicians in 2034, according to The Complexities of Physician Supply and Demand Projections From 2019 to 2034 from the Association of American Medical Colleges (AAMC). Published 11th June 2021, the report was prepared by IHS Markit Ltd. and updates AAMC’s six previous annual reports on physician workforce projections. In this year’s projections, AAMC considers the long-term implications of the COVID-19 pandemic on physician supply, new to this report. Another timely feature in the 2021 study is the Health Care Utilization Equity Scenario which provides a baseline looking at inequities in access
Post-Pandemic, U.S. Healthcare is Entering a “Provide More Care For Less” Era – Pondering PwC’s 2022 Forecast

In the COVID-19 pandemic, health care spending in the U.S. increased by a relatively low 6.0% in 2020. This year, medical cost trend will rise by 7.0%, expected to decline a bit in 2022 according to the annual study from PwC Health Research Institute, Medical Cost Trend: Behind the Numbers 2022. What’s “behind these numbers” are factors that will increase medical spending (the “inflators” in PwC speak) and the “deflators” that lower costs. Looking around the future corner, the inflators are expected to be: A COVID-19 “hangover,” leading to increased health care services utilization Preparations for the next pandemic, and
Telehealth Bolsters Patient Satisfaction (J.D. Power), and Providers Are Working to Catch Up (BDO)
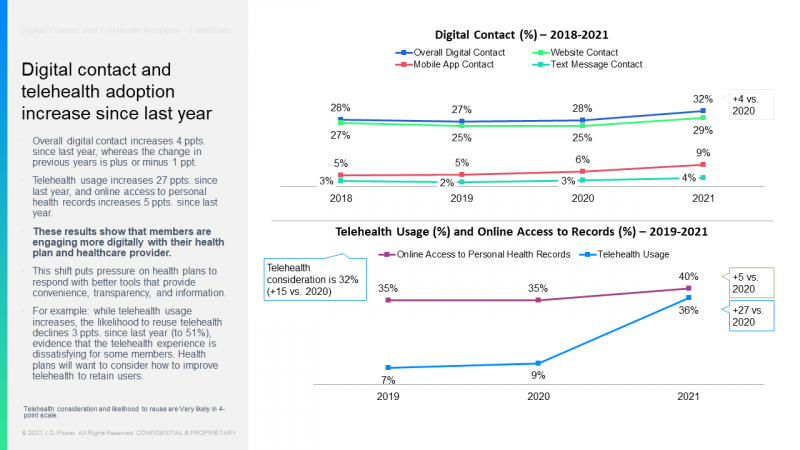
Two studies published in May 2021 illustrate the value and importance of telehealth to patients in 2020, and a disconnect among many C-level executives working in hospitals, academic medical centers, and other care provider organizations. Together, the two reports from J.D. Power and BDO illustrate some mis-alignment between the demand and supply side of telehealth. On the consumer demand side, patients’ growing use of telehealth in the COVID-19 pandemic along with more frequent digital contacts with health plans bolstered member satisfaction, discovered by the J.D. Power 2021 U.S. Commercial Member Health Plan Study. J.D. Power has conducted the U.S. Commercial
Healthcare, Heal Thyself! How the Industry Can and Should Play the Trust Card
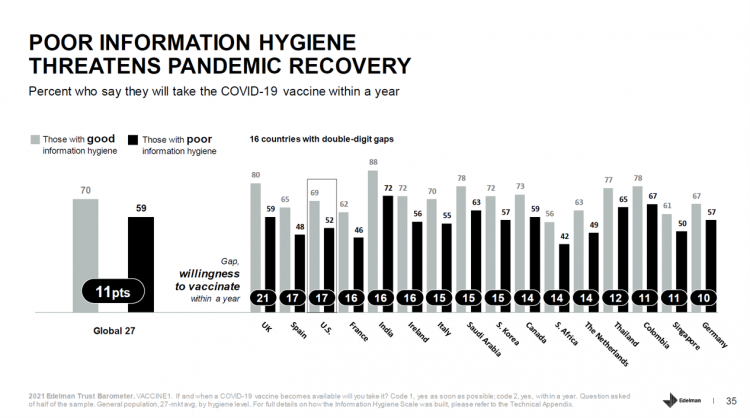
The emergence of the COVID-19 vaccine “infodemic” has slowed the ability for nations around the world to emerge out of the public health crisis. Growing cynicism among some health citizens facing the politicization of public health tactics like vaccines and facial masks is what we’re talking about. At the root is peoples’ lack of trust across a range of information providers, including government, media, business, and even peers. The 2021 Edelman Trust Barometer spotlighted the infodemic and eroding trust in the U.S. in the voices of public health, the public sector, and media. This is a global challenge as well,
The ROI on Virtual Care – Thinking About Value and Future Prospects With the AMA
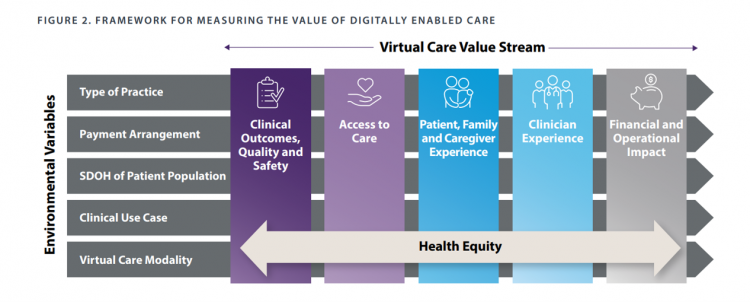
When a new technology or product starts to get used in a market, it follows a diffusion curve whose slope depends on the pace of adoption in that market. For telehealth, that S-curve has had a very long and fairly flat front-end of the “S” followed by a hockey stick trajectory in March and April 2020 as the COVID-19 pandemic was an exogenous shock to in-person health care delivery. The first chart from the CDC illustrates that dramatic growth in the use of telehealth ratcheting up since the first case of COVID-19 was diagnosed in the U.S. Virtual care has
Nurses Hacking for Health and Compassionomics

The hearts and minds of nurses are fertile and inspirational sources and engines for health care innovation. This past weekend, and for the second time, I had the privilege and opportunity to be a panelist for the perennial hackathon meet-up of Nurse Hack 4 Health, sponsored by Microsoft, Johnson & Johnson, Sonsiel, and DevUp. This round, the hackathon attracted hundreds of nurses from at least 20 countries and 30 U.S. states. Even a few students attended, a growing trend as academia recognizes the shortage of workers trained to solve thorny problems of the world. In health care, right here, right
Spending on Medicines In and Post-COVID Say a Lot About Patients and Larger Healthcare Trends – an IQVIA Update
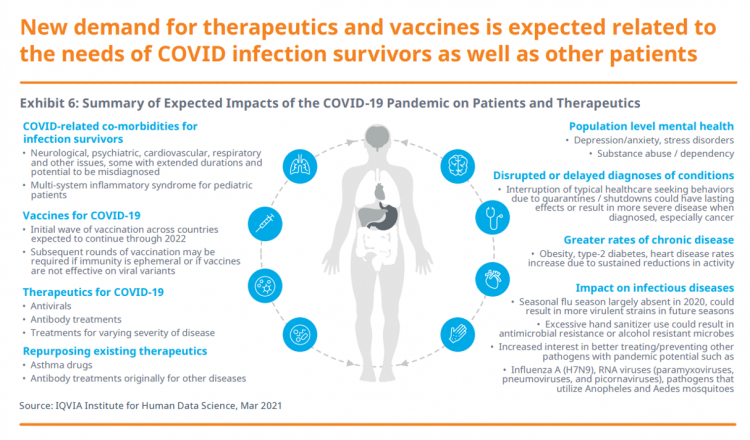
Spending on medicines, globally, will rebound this year and rise above pre-pandemic levels through 2025. Between 2021 and 2025, the annual growth global growth rate for prescription drugs spending is expected to range from 3% to 6%, a $1.6 trillion bill for the worlds’s total Rx medicines market. That relatively low single-digit growth rate is tempered by savings from biosimilars and the loss of brand exclusivity (that is, more generics coming to market). On the faster-growth side, we can expect two big therapeutic areas to drive spending upward: oncology and immunology, projected to expand by 9% to 12% each year
The Pandemic’s Death Rate in the U.S.: High Per Capita Income, High Mortality
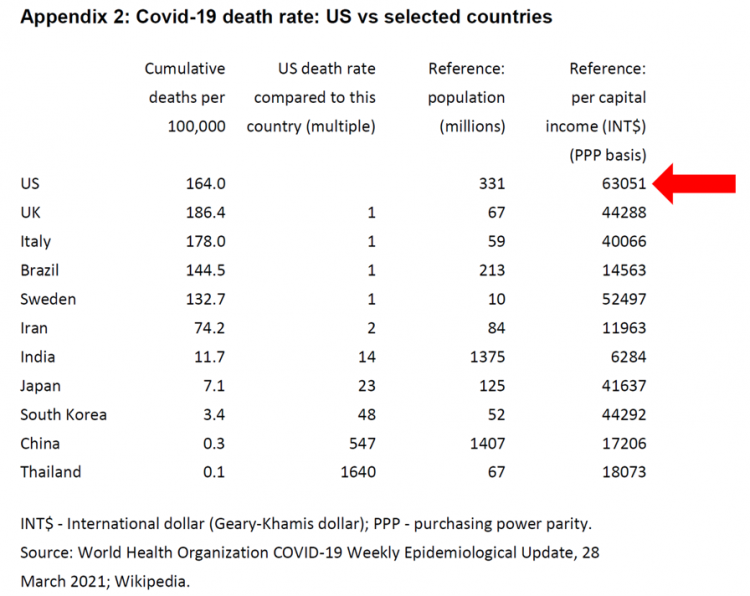
The United States has among the highest per capita incomes in the world. The U.S. also has sustained among the highest death rates per 100,000 people due to COVID-19, based on epidemiological data from the World Health Organization’s March 28, 2021, update. Higher incomes won’t prevent a person from death-by-coronavirus, but risks for the social determinants of health — exacerbated by income inequality — will and do. I have the good fortune of access to a study group paper shared by Paul Sheard, Research Fellow at the Mossaver-Rahmani Center for Business and Government at the Harvard Kennedy School. In reviewing
Emerging with A Stronger Healthcare System Post-COVID: NAM’s Lessons Learned
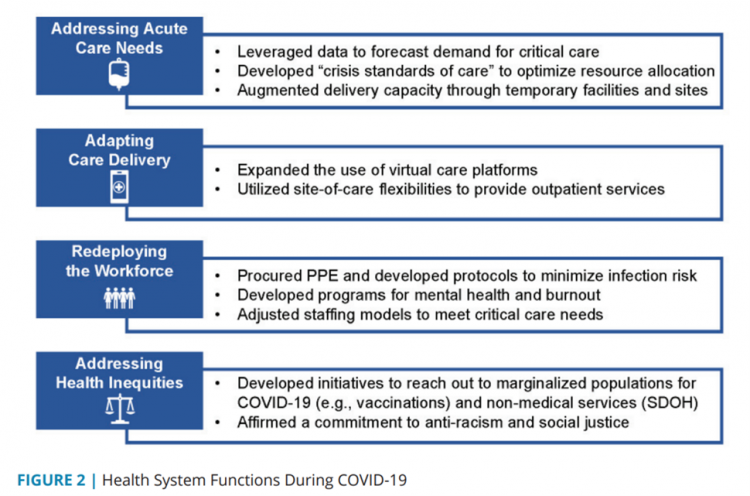
The coronavirus pandemic exposed weaknesses in the U.S. health care system that existed before the public health crisis. What lessons can be learned from the COVID-19 stress-test to build American health care back better? The National Academy of Medicine is publishing nine reports addressing health stakeholder segments impacted and re-shaped by COVID-19 — for public health, quality and safety, health care payers, clinicians, research, patients-families-communities, health product manufacturers, digital health, and care systems. The report on health care systems and providers was released this week: COVID-19 Impact Assessment: Lessons Learned and Compelling Needs was authored by experts on the front-line
The Continued Erosion of Trust in the Age of COVID
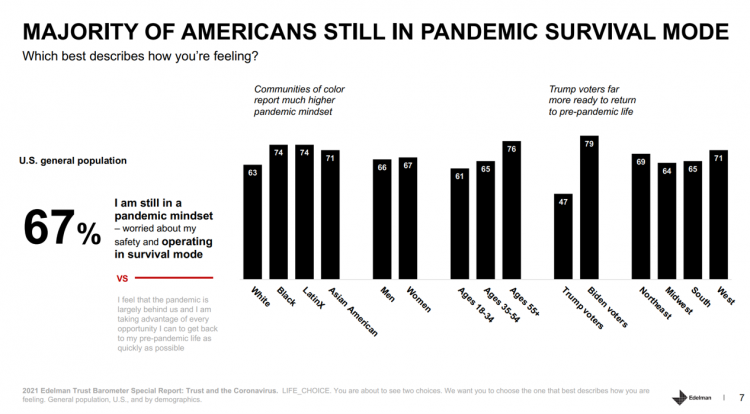
A year into the COVID-19 pandemic, most Americans are still in “survival mode,” according to an update of the 2021 Edelman Trust Barometer, Trust and the Coronavirus in the U.S. Updating the company’s annual Trust Barometer, Edelman conducted a new round of interviews in the U.S. among 2,500 people in early March. [For context, you can read my take on the 2021 Edelman Trust Barometer published during the World Economic Forum in January 2021 here in Health Populi]. The first chart shows that two in three people in the U.S. are still in a pandemic mindset, worried about safety and
Three in Four People Avoiding Health Care in the Pandemic Have Had Chronic Conditions
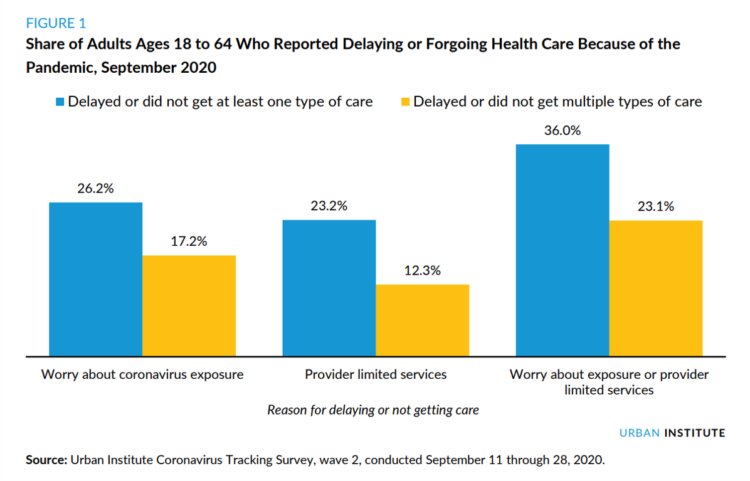
By the autumn of 2020, U.S. physicians grew concerned that patients who were avoiding visits to doctor’s offices were missing care for chronic conditions, discussed in in Delayed and Forgone Health Care for Nonelderly Adults during the COVID-19 Pandemic from the Urban Institute. More than three-fourths of people who delayed or forewent care had at least one chronic health condition. The pandemic may have led to excess deaths from diabetes, dementia, hypertension, heart disease, and stroke, as well as record drug overdoses in the 12 months ending in May 2020. In their JAMA editorial on these data, Dr. Bauchner and
Call It Deferring Services or Self-Rationing, U.S. Consumers Are Still Avoiding Medical Care
Patients in the U.S. have been self-rationing medical care for many years, well before any of us knew what “PPE” meant or how to spell “coronavirus.” Nearly a decade ago, I cited the Kaiser Family Foundation Health Security Watch of May 2012 here in Health Populi. The first chart here shows that one in four U.S. adults had problems paying medical bills, largely delaying care due to cost for a visit or for prescription drugs. Fast-forward to 2020, a few months into the pandemic in the U.S.: PwC found consumers were delaying treatment for chronic conditions. In October 2020, The American Cancer
Dr. Burnout – The 2021 Medscape Physician Burnout & Suicide Report
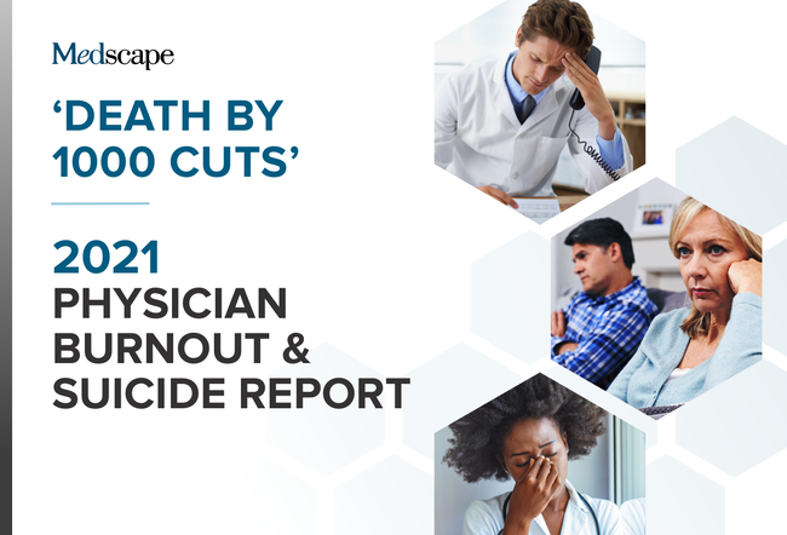
Physicians in the U.S. are experiencing “death by 1,000 cuts,” according to the 2021 Medscape Physician Burnout & Suicide Report. Medscape polled 12,339 physicians representing over 29 specialties between late August and early November 2020 to gauge their feelings about work and life in the midst of the coronavirus pandemic. Medscape researched its first Physician Lifestyle Report in 2012. That research focused on physician “happiness” and work-life satisfaction. In 2013, the issue of burnout was called out on the cover of the report, shown here with the question, “does burnout affect lifestyle?” In 2015, the Physician Lifestyle Report was titled,
Our Homes Are Health Delivery Platforms – The New Home Health/Care at CES 2021

The coronavirus pandemic disrupted and re-shaped the annual CES across so many respects — the meeting of thousands making up the global consumer tech community “met” virtually, both keynote and education sessions were pre-recorded, and the lovely serendipity of learning and meeting new concepts and contacts wasn’t so straightforward. But for those of us working with and innovating solutions for health and health care, #CES2021 was baked with health goodness, in and beyond “digital health” categories. In my consumer-facing health care work, I’ve adopted the mantra that our homes are our health hubs. Reflecting on my many conversations during CES
Will 2021 Be the Year of Sicker Americans? Pondering Late 2020 Data from IQVIA
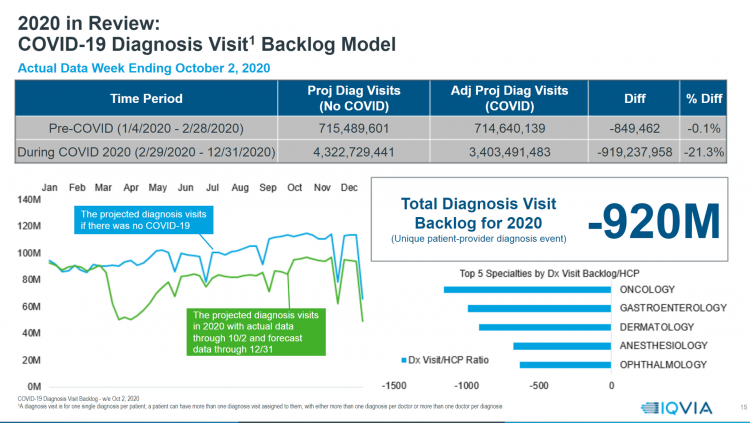
Yesterday, IQVIA presented their end-of-year data based on medical claims in the U.S. health care system tracking the ups, downs, and ups of the coronavirus in America. IQVIA has been tracking COVID-19 medical trends globally from early 2020. The plotline of patient encounters for vaccines, prescribed medicines, foregone procedures and diagnostic visits to doctors begs the question: in 2021, will Americans be “sicker,” discovering later-stage cancer diagnoses, higher levels of pain due to delayed hip procedures, and eroded quality of life due to leaky guts? Here are a few snapshots that paint a picture for greater morbidity and potentially more “excess
Will We See A Field of Dreams for the COVID-19 Vaccine in the U.S.?
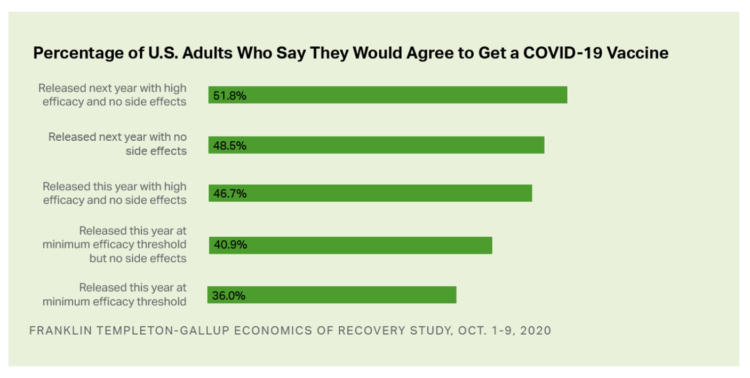
“If you build it, he will come,” the voice of James Earl Jones echoes in our minds when we recall the plotline of the film, Field of Dreams. A quick summary if you don’t know the movie: the “it” was a baseball field to be built in a rural cornfield. The “he” was a baseball player, ultimately joined by a dream-team of ball players who would convene on that dreamy field to play an amazing game. Today, the day after Pfizer announced a 90% benefit for its coronavirus vaccine, bolstering Wall Street returns on 9th November 2020, two new consumer
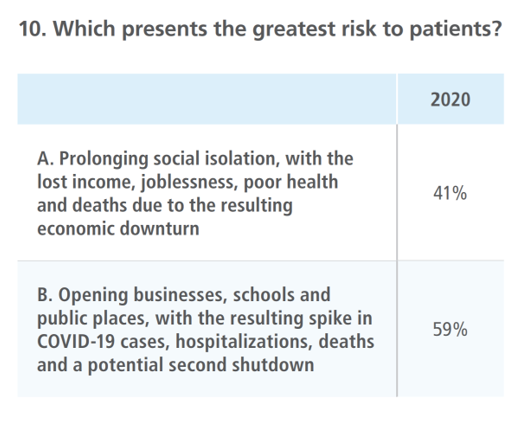
Voting for Health in 2020

In the 2018 mid-term elections, U.S. voters were driven to polls with health care on their minds. The key issues for health care voters were costs (for care and prescription drugs) and access (read: protecting pre-existing conditions and expanding Medicaid). Issue #2 for 2018 voters was the economy. In 2020, as voting commences in-person tomorrow on 3rd November, U.S. voters have lives and livelihoods on their minds. It’s the pandemic – our physical lives looming largest in the polls – coupled with our fiscal and financial lives. Health is translating across all definitions for U.S. voters in November 2020: for
Health Care Providers Are More Politically Engaged in the 2020 Elections
Until 2016, physicians’ voting rates in U.S. elections had not changed since the late 1970s. Then in 2018, two years into President Donald Trump’s four-year term, the mid-term elections drove U.S. voters to the election polls…including health care providers. Based on the volume and intensity of medical professional societies’ editorials on the 2020 Presidential Election, we may be in an inflection-curve moment for greater clinician engagement in politics as doctors and nurses take claim of their health citizenship. A good current example of this is an essay published in the AMA’s website asserting, “Why it’s okay for doctors to ask
Healthcare Costs, Access to Data, and Partnering With Providers: Patients’ Top User Experience Factors
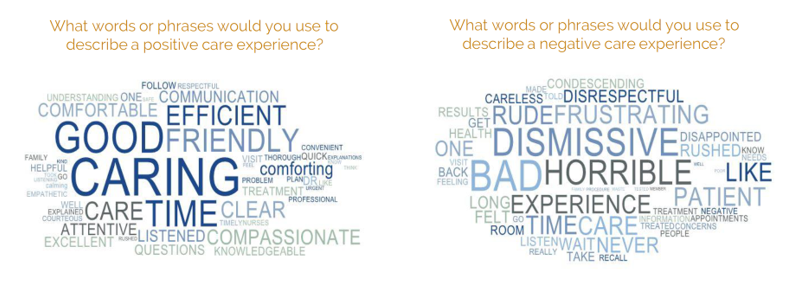
As patients returned to in-person, brick-and-mortar health care settings after the first wave of COVID-19 pandemic, they re-enter the health care system with heightened consumer expectations, according to the Beryl Institute – Ipsos Px Pulse report, Consumer Perspectives on Patient Experience in the U.S. Ipsos conducted the survey research among 1,028 U.S. adults between 23 September and 5 October 2020 — giving consumers many months of living in the context of the coronavirus. This report is a must-read for people involved with patient and consumer health engagement in the U.S. and covers a range of issues. My focus in this
Redefining PPE As Primary Care, Public Health, and Health Equity – The Community PPE Index
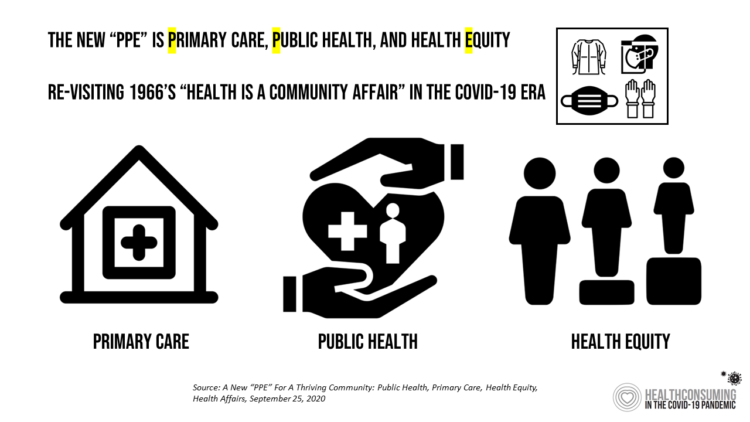
In May 2020, the Oxford English Dictionary (OED) re-visited the acronym, “PPE.” As OED evolves the definition of PPE, the wordsmiths could borrow from OSHA’s website, noting that PPE, “is equipment worn to minimize exposure to hazards that cause serious workplace injuries and illnesses. These injuries and illnesses may result from contact with chemical, radiological, physical, electrical, mechanical, or other workplace hazards. Personal protective equipment may include items such as gloves, safety glasses and shoes, earplugs or muffs, hard hats, respirators, or coveralls, vests and full body suits.” Perhaps Definition 3 in the OED could be updated by a blog
Digital Health Gaps in the Pandemic Through the Eyes of Younger Physicians

One universal experience health systems around the globe have witnessed in the first months of the coronavirus pandemic has been the dramatic pivot to telehealth and virtual care platforms. The latest report from Philips Future Health Index series attests to that, and to clinicians’ general recognition that telehealth has been crucial in the early phase of the crisis. However, younger doctors’ experience with telehealth has led to them being more bullish on the value of the modality than older physicians, Philips learned. Philips conducted 500 interviews with doctors in China, France, Germany, Singapore, and the United States to assess their
Telehealth Use Among Older Americans: Growing Interest, Remaining Concerns
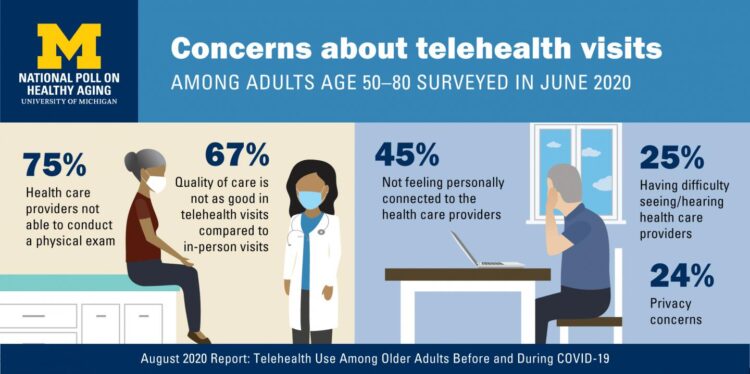
In the Fear of Going Out Era spawned by the COVID-19 pandemic, many patients were loath to go to the doctor’s office for medical care, and even less keen on entering a hospital clinic’s doors. This drove health consumers to virtual care platforms in the first months of the public health crisis — including lots of older people who had never used telemedicine or even a mobile health app. In the August 2020 National Poll on Heathy Aging, the University of Michigan research team found a 26% increase in telehealth visits from 2019 to 2020, March to June 2020 year-over-year.
Physicians Practicing in the Age of COVID-19: Lower Incomes, More Telehealth
In the midst of the coronavirus pandemic, two certainties emerge in the lives of physicians: they are generating less revenue, and they have adopted more virtual care in practices. The Physicians Foundation surveyed 3,513 physicians in July 2020 on their perspectives on COVID-19 and how the pandemic has impacted practices and patients. This study is part one of three conducted by the Foundation this year, subtitled the “COVID-19 Impact Edition” of the 2020 Survey of America’s Physicians which the Foundation conducts each year. Merritt Hawkins conducted the study on behalf of the Foundation, shifting the focus to the pandemic. This
Growing Evidence for eConsults – the Asynchronous, Clinician-to-Clinician Platform for Telehealth
Health care providers stood up virtual health care services with lightning speed as the coronavirus pandemic emerged in the U.S. Telehealth and its various flavors enabled both patients and providers to manage the risk of contracting the virus, especially at a time when little was known about the nature of transmission, treatment and prevention — except for washing hands, covering one’s face, and isolating when showing symptoms. In Electronic Consultations (eConsults): A Triple Win for Patients, Clinicians, and Payers, the Milbank Memorial Fund explores the evidence supporting the growth of asynchronous electronic consultation encounters between patients and clinicians. Note that
How COVID-19 Has Re-Shaped Health Care Delivery So Far
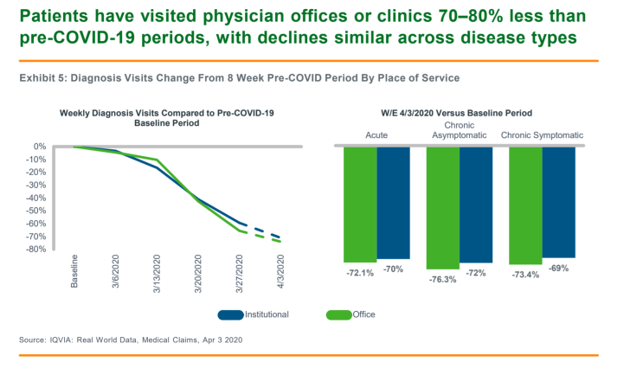
COVID-19 is re-shaping health care in America across many dimensions. In Shifts in Healthcare Demand, Delivery and Care During the COVID-19 Era, IQVIA presents a multi-faceted profile of the early impacts of the pandemic on U.S. health care. In the report, published in April 2020, IQVIA mined the company’s many data bases that track real-time data, including medical claims, flu data, sales data, oncology medical and pharmacy claims, formularies, among other sources. Top-line, IQVIA spotted the following key shifts in U.S. health care since the start of the coronavirus pandemic: Patients’ use of health services Impacts on medicine use, influenced
Honor Your Doctor – It’s National Doctors Day Today (and EveryDay)
Today, March 30, is National Doctors Day. We honor doctors annually on this day. But every day, we must honor physicians for bolstering the health and wellness of our fellow Americans, our beloved families and friends, and our selves. The Coronavirus Pandemic reminds us of the precious and scarce resource that is our national supply of physicians in America — numbering about 750,000 active clinicians in the U.S. according to the U.S. Bureau of Labor Statistics. Even before the COVID-19 crisis, physicians in America had been feeling increasingly burned out and depressed. The 2020 WebMD survey on the state of
Physicians Lean In to Digital Health, Especially Telehealth and Remote Monitoring
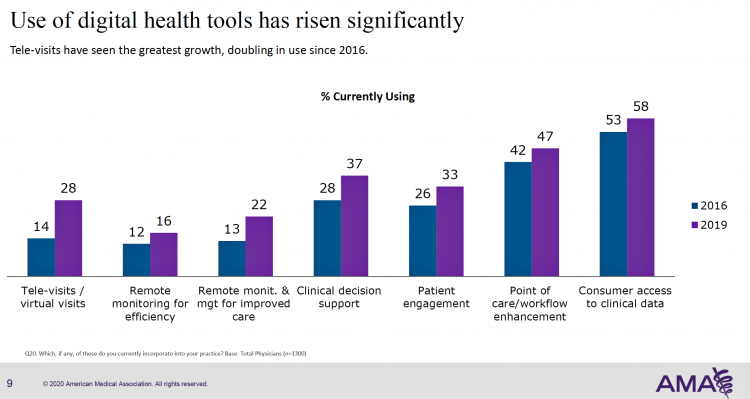
More U.S. doctors are using digital health tools in patient care, with quickening adoption of telehealth and remote monitoring technology, according to a study from the American Medical Association (AMA). This survey, conducted in 2019 among 1,359 U.S. physicians, follows up AMA’s research conducted in 2016 and largely reflects the original questionnaire to be able to understand real changes among doctors’ use of tech in practice. As part of this rigorous study design, AMA used particular definitions for the seven tools the study gauged: remote monitoring for efficiency, remote monitoring and management for improved care, clinical decision support, patient engagement,
What’s Causing Fewer Primary Care Visits in the US?
Americans who have commercial health insurance (say, through an employer or union) are rarely thought to face barriers to receiving health care — in particular, primary care, that front line provider and on-ramp to the health care system. But in a new study published in the Annals of Internal Medicine, commercially-insured adults were found to have visited primary care providers (PCPs) less often, and 1 in 2 had no PCP visits in one year. In Declining Use of Primary Care Among Commercially Insured Adults in the United States, 2008-2016, the researchers analyzed data from a national sample of adult health
Physicians in America – Too Many Burned Out, Depressed, and Not Getting Support
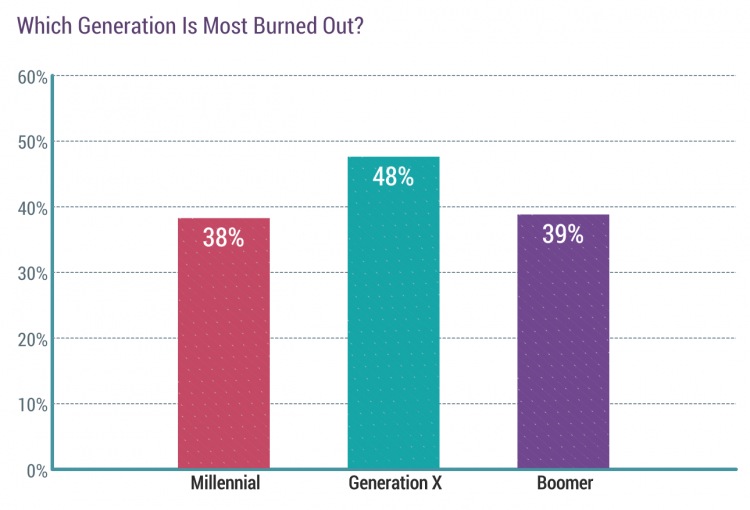
Some one in three physicians is burned out, according to the Medscape’s National Physician Burnout & Suicide Report. The subtitle, “The Generational Divide,” tells a bit part of the subtext of this annual report that’s always jarring and impactful for both its raw numbers and implications for both patient care and the larger health care system in America. Nearly 1 in 2 physicians in Generation X, those people born between 1965 and 1979, feel burned out compared with roughly 4 in 10 doctors who are Millennials or Boomers. Furthermore, many more women than men physicians feel burned out: 48% of
Home Is Where the Health Is, CareMore Health (And Most People) Believe
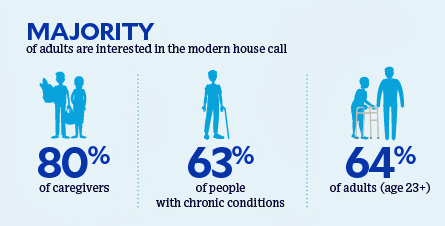
Most people dealing with chronic conditions, and those who care for them, believe that “home is where the health is,” according to a survey about the “21st century house call” from CareMore Health. To gain peoples’ perspectives on health care at home and chronic disease management, CareMore Health and Aspire Health commissioned a survey among 2,009 U.S. adults 23 years of age and over in September and October 2019. The survey sample included people dealing with chronic disease themselves, as well as caregivers attending to people with chronic illnesses. The definition of that “modern house call” is largely based on the
Dr. Roboto? Stanford Medicine Foresees Digital Doctors “Maturing”
Physicians are evolving as digital doctors, embracing the growing role of data generated in electronic health records as well as through their patients using wearable technologies and mobile health apps downloaded in ubiquitous smartphones, described in The Rise of the Data-Driven Physician, a 2020 Health Trends Report from Stanford Medicine Stanford Medicine interviewed 523 physicians and 210 medical students and residents in September and October 2019 to assess clinicians’ perspectives on digital health topics for this study. The study title citing the “data-driven physician” is based on the key survey finding that doctors are preparing to embrace data, from both traditional
Nurses Continue to Reign #1 in Honesty and Ethics; Healthcare Pro’s 4 of Top 5 in Annual Gallup Poll
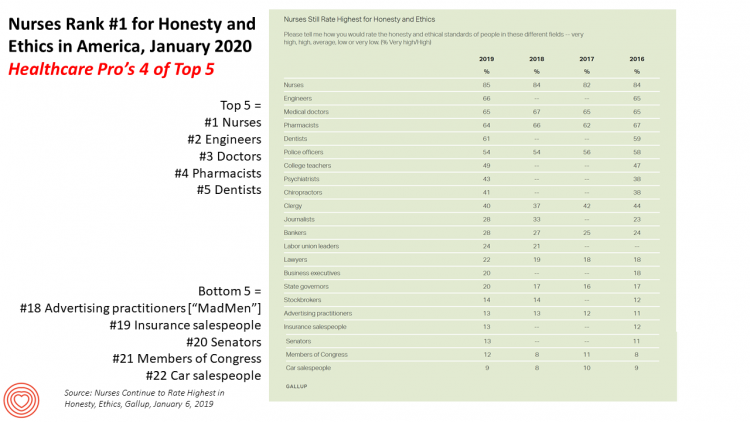
The topline of this year’s annual Gallup Poll into honesty and ethics of professions finds nurses sustaining their reign as the top trusted profession in America. But it’s also important to point out that four of the top five most ethical professions are people working on the front lines of health care: doctors (#3), pharmacists (#4) and dentists (#5). Engineers rank second this year after nurses, edging ahead of doctors and pharmacists who typically have ranked 2nd and 3rd each year in the past decade. One of these years, pharmacists’ reputation fell as the profession was associated with being a
Medicare Members Are Health Consumers, Too – Our AHIP Talk About Aging, Digital Immigrants, and Personalizing Health/Care
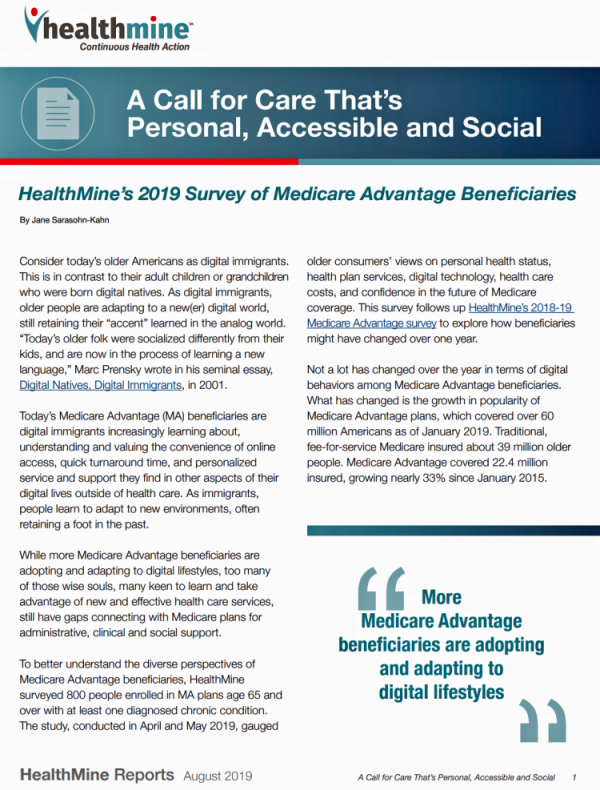
As Boomers age, they’re adopting mobile and smart technology platforms that enable people to communicate with loved ones, manage retirement investment portfolios, ask Alexa to play Frank Sinatra’s greatest hits, and manage prescription refills from the local grocery store pharmacy. Last week, the Giant Eagle grocery chain was the first pharmacy retailer to offer a new medication management skill via Alexa. That program has the potential to change our Medicare members manage meds at home to ensure better adherence, supporting better health outcomes and personal feelings of efficacy and control. [As an aside, consumers really value pharmacies embedded in grocery
Hospitals Suffer Decline in Consumer Satisfaction

While customer satisfaction with health insurance plans slightly increased between 2018 and 2019, patient satisfaction with hospitals fell in all three settings where care is delivered — inpatient, outpatient, and the emergency room, according to the 2018-2019 ACSI Finance, Insurance and Health Care Report. ACSI polls about 300,000 U.S. consumers each year to gauge satisfaction with over 400 companies in 46 industries. For historic trends, you can check out my coverage of the 2014 version of this study here in Health Populi. The 2019 ACSI report bundles finance/banks, insurance (property/casualty, life and health) and hospitals together in one document. Health
Social Determinants of Health – My Early Childhood Education and Recent Learnings, Shared at the HealthXL Global Gathering
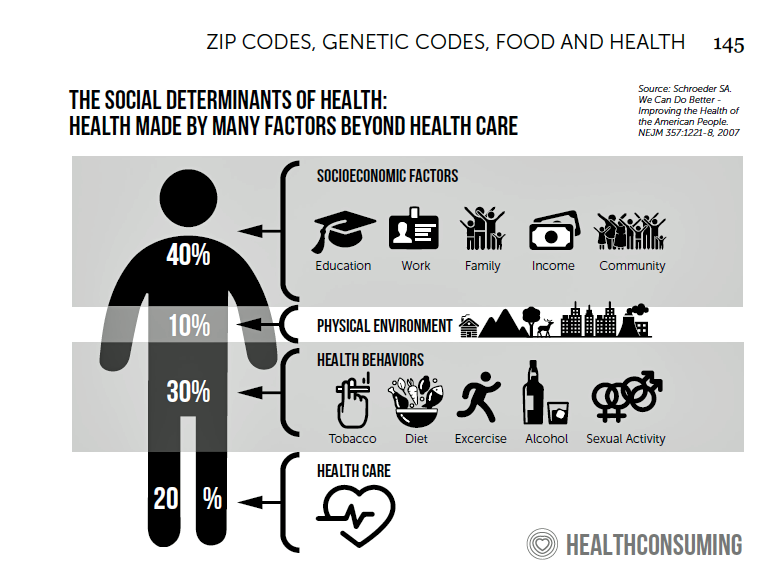
My cousin Arlene got married in Detroit at the classic Book Cadillac Hotel on July 23, 1967, a Sunday afternoon wedding. When Daddy drove us back out to our suburban home about 30 minutes from the fancy hotel, the car radio was tuned to WWJ Newsradio 950, all news all the time. As soon as Daddy switched on the radio, we were shocked by the news of a riot breaking out in the city, fires and looting and gunshots and chaos in the Motor City. Two days later, my father, who did business with Mom-and-Pop retail store owners in the
Will Consumers Cross the Cost-and-Trust Chasm Between Prescription Drugs and Hospitals?
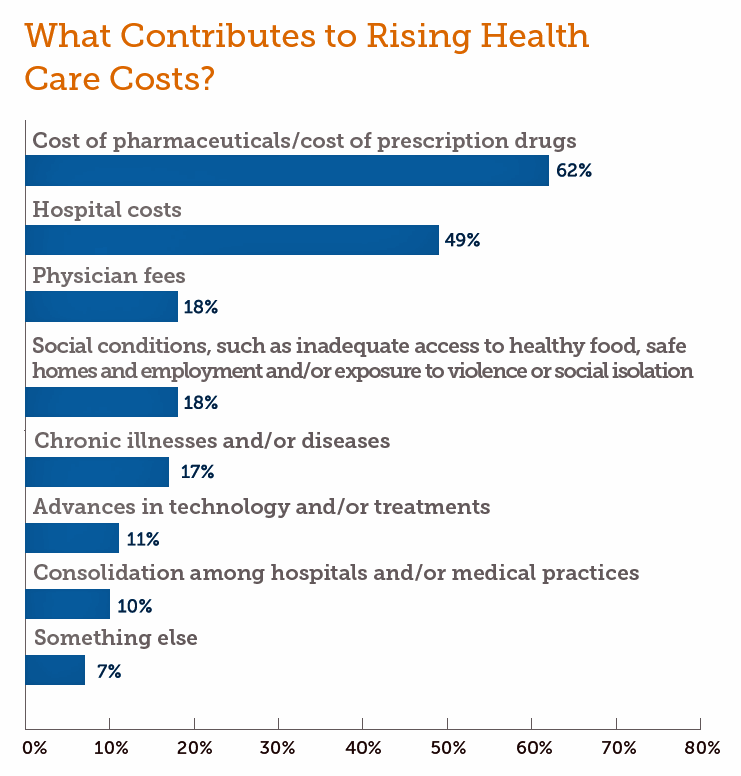
People in the U.S. rank prescription drugs, lab tests, emergency room visits, dental and vision care, preventive services, chronic disease management and mental health care as the “most essential” health care services, according to the 2019 Survey of America’s Patients conducted by The Physicians Foundation. When asked what factors contribute to rising health care costs in America, most consumers cite the cost of prescription drugs. Taken together, these two data points demonstrate the potent political import of prescription drug prices as the U.S. approaches the 2020 Presidential election. The Physicians Foundation surveyed 2,001 U.S. adults between 27 and 75 years
Making Health Care Better, from the N of 1 to the Public’s Health – Trend-Weaving Medecision Liberation 2019
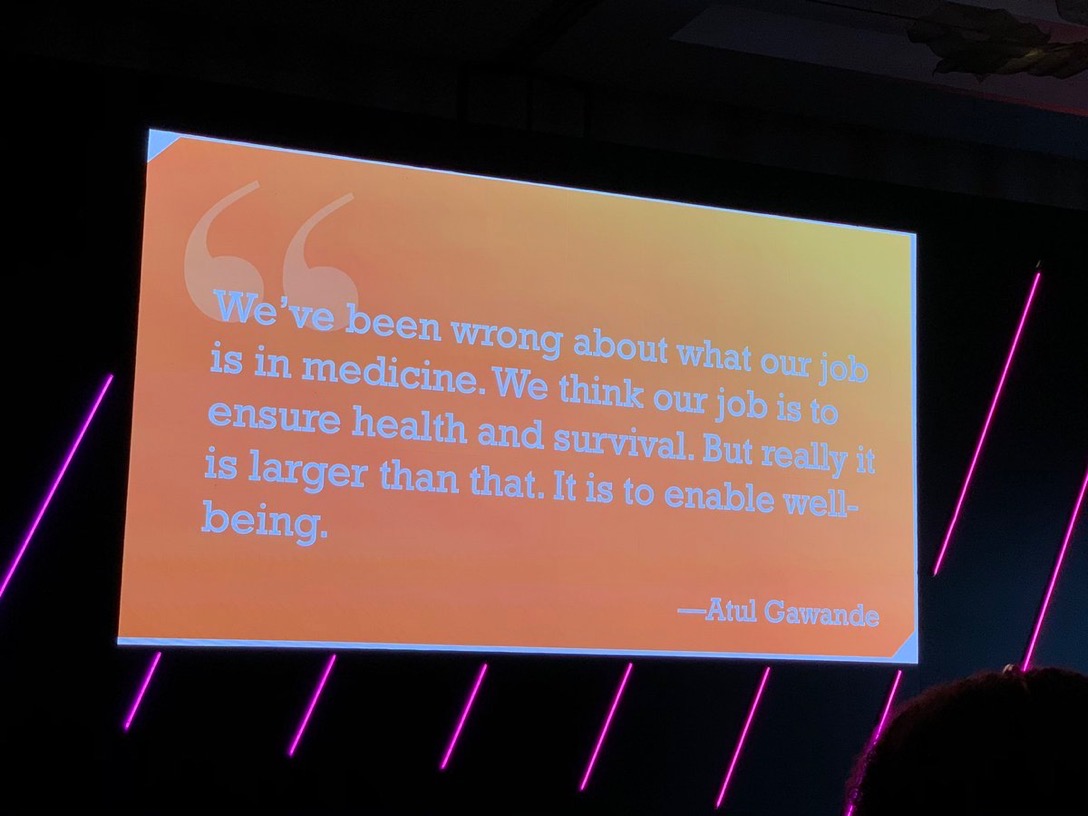
Health and our health information are deeply personal. Changing health care and inspiring positive health behaviors is hard to do. But we must and we will, a group of inspiring and inspired people who work across the health/care ecosystem affirmed this week in Dallas at the conference of Medecision Liberation 2019. I was engaged at this conference to wear several hats — as a keynote speaker, a sort of “emcee,” and, finally, to trend-weave the many talks and discussions happening throughout the meeting. This post is my synthesis of the summary I delivered live at the end of the conference,
Prelude to Health 2.0 2019: Thinking Consumers At the Center of Digital Health Transformation

“Digital transformation” is the corporate strategy flavor of the moment across industries, and the health are sector isn’t immune from the trend. As this 13th year of the annual Health 2.0 Conference kicks off this week, I’m focused on finding digital health innovations that engage people — consumers, caregivers, patients, health citizens all. This year’s conference will convene thought leaders across a range of themes, and as is the Health 2.0 modus operandi, live demo’s of new-new things. As Health 2.0 kicks off today in pre-conference sessions, there is useful context described in a new report from the American Hospital
Health Consumers Expect Healthcare to be Digital (and Secure), Philips Future Health Index Finds

Health care system financing, delivery, and workflows widely vary across nations around the world. Philips surveyed health care professionals and consumers living in 15 countries, from North America to Asia, and found that these health systems share one over-arching objective: to provide quality care with improved experiences for both patients and healthcare professionals. Being Philips, what underpins that quality and experience is technology; Philips explored telehealth, AI, digital health records (DHRs), and other digital health tools that can engage patients. Philips published results from this global study in The Future Health Index 2019, themed “Transforming healthcare experiences, exploring the impact
Milliman Finds PPO for Family of 4 in 2019 Will Cost $28,386
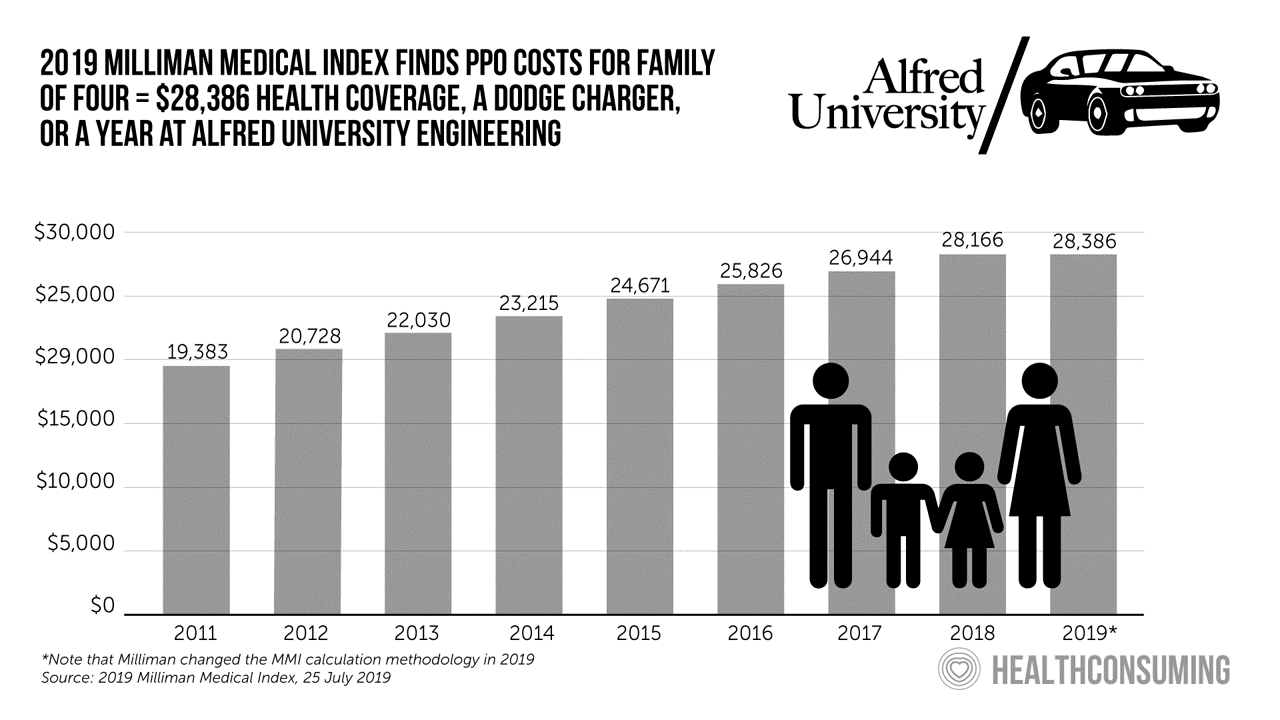
This year, an employer-sponsored PPO for a family of four in the U.S. will cost $28,386, a 3.6% increase over 2018, according to the 2019 Milliman Medical Index (MMI). Based on my annual read of this year’s Index, the PPO costs roughly the same as a new Dodge Charger or a year attending the engineering school at Alfred University. The Milliman MMI team has updated the methodology for the Index; the chart shown here is my own, recognizing that the calculations and assumptions beneath the 2019 data point differ from previous years. The key points of the report are that:
Finances Are the Top Cause of Stress, and HSAs Aren’t Helping So Much…Yet

If you heed the mass media headlines and President Trump’s tweets, the U.S. has achieved “the best economy” ever in mid-July 2019. But if you’re working full time in that economy, you tend to feel much less positive about your personal prospects and fiscal fitness. Nearly nine in 10 working Americans believe that medical costs will rise in the next few years as they pondering potential changes to the Affordable Care Act. The bottom line is that one-half of working people are more concerned about how they will save for future health care expenses. That’s the over-arching theme in PwC’s
Health Care and Consumers in 2030: A Profile from KPMG

A “one layered delivery network through which patients can move seamlessly as they age and their needs evolve” will be the new health care platform to meet patients’ demands by 2030, according to a forecast from KPMG’s Healthcare and Life Sciences Institute. In Healthcare 2030: The consumer at the center, the KPMG team explores the demographic shifts and market drivers that will challenge the health care industry in the current U.S. delivery and financing system. The lens on that 2030 future is a consumer-centric delivery model that KPMG believes will be a solution to dealing with a demographic divide between
Will Health Consumers Morph Into Health Citizens? HealthConsuming Explains, Part 5

The last chapter (8) of HealthConsuming considers whether Americans can become “health citizens.” “Citizens” in this sense goes back to the Ancient Greeks: I return to Hippocrates, whose name is, of course, the root of The Hippocratic Oath that physicians take. Greece was the birthplace of Democracy with a capital “D.” Hippocrates’ book The Corpus is thought to be one of the first medical textbooks. The text covered social, physical, and nutritional influences, and the concept of “place” for health and well-being. Here, the discussion detailed the roles of air and water for health. The Hippocratic texts also coached doctors to
Americans’ Trust in U.S. Healthcare Lags Tech — and Women Are Particularly Cynical
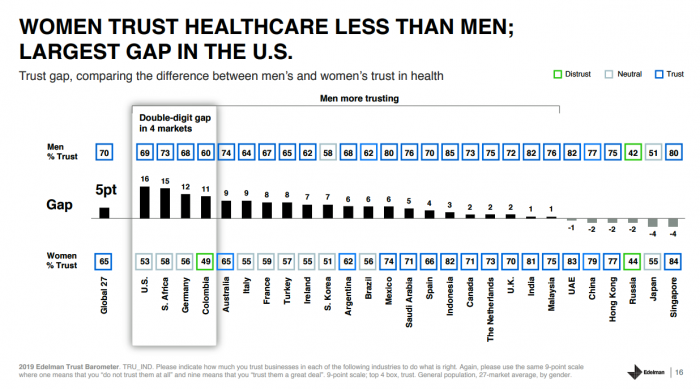
The 2019 Edelman Trust Barometer measured the biggest gap in trust for the healthcare industry between the U.S. “informed public” and the mass population. Fewer American women, too, trust the healthcare industry than men do. “This inequality of trust may be reflective of the mass population continuing to feel left behind as compared to others, even as they recognize the advances that are being made that could benefit them. Given tone and tenor of the day, and particularly among mass population, healthcare may continue to see increasing demands for change and regulation,” Susan Isenberg, Edelman’s head of healthcare, notes in
The Expectation Gap Between What Patients Want Vs What They Get
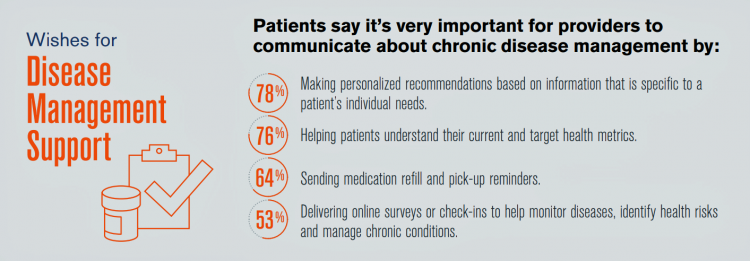
Talk to me, patients are demanding in unison. Most health consumers expect providers to communicate about routine health care and prevention; this is especially true among those patients trying to manage chronic conditions we learn from 10 Ways to Fulfill Patients’ Communication Wish List, a report based on a consumer survey from West, the communications and network infrastructure company. Four in five patients say that talking to “me” means they want personalized recommendations to their unique needs – but only one-third of patients say they’re getting that level of service from their healthcare providers. Most health consumers expect providers to communicate about
What #CES2019 5 Tech Trends to Watch Mean for Health/Care

As #CES2019 kicks off in Las Vegas with today’s first Media Day, the Consumer Technology Association presented its forecast on the 5 Technology Trends to Watch in 2019 — and they all play into health, wellness, and medical care. The five trends are: Artificial Intelligence on the Rise Envisioning the Smart Home of the Future Digital Health Tech Empowers Patients Esports and Sports Technology, and Smart Cities Promote Resilience. Here are how these five mega-trends can bolster our health and healthcare products and services over the next decade. AI is indeed on-the-rise in healthcare: as I have begun planning my agenda for
Nurses are the most trusted profession in America, followed by doctors and pharmacists

Nurses rank top in Americans’ minds for the seventeenth year-in-a-row, Gallup found in its annual survey of honesty and ethics in professions. At the bottom of the list for honesty and ethics in 2018, Gallup points to U.S. Congressional representatives, “Mad Men” and Women of advertising, telemarketers, and folks who sell autos. Congress-folk and car salespeople have ranked at the low-trust bottom for many years in this Gallup poll. While the 3 health care professions rose once again to the top of the job-trust roster, nurses rank far greater than doctors and pharmacists by a 17-point margin of consumers rating the
Costs, Consumerism, Cyber and Care, Everywhere – The 2019 Health Populi TrendCast

Today is Boxing Day and St. Stephens Day for people who celebrate Christmas, so I share this post as a holiday gift with well-wishes for you and those you love. The tea leaves have been brewing here at THINK-Health as we prepared our 2019 forecast at the convergence of consumers, health, and technology. Here’s our trend-weaving of 4 C’s for 2019: costs, consumerism, cyber and care, everywhere… Health care costs will continue to be a mainstream pocketbook issue for patients and caregivers, with consequences for payors, suppliers and ultimately, policymakers. Legislators inside the DC Beltway will be challenged by the
Most U.S. Physicians, Burned Out, Favor A Flavor of Single Payer Health System

Most physicians feel some level of burnout, hassled by electronic health records and lost autonomy. No wonder, then, that a majority of doctors favor some type single payer health system — one-quarter fully single payer, a la Britain’s National Health Service; and another one-third a single payer combined with a private insurance option, discovered in the 2018 Survey of America’s Physicians report on practice patterns & perspectives, published by The Physicians Foundation. Eight in ten physicians are working at full-capacity or are over-extended, the survey found. Furthermore, 62% of doctors are pessimistic about the future of medicine. Physician burnout is a
The Digital Health Consumer According to Rock Health
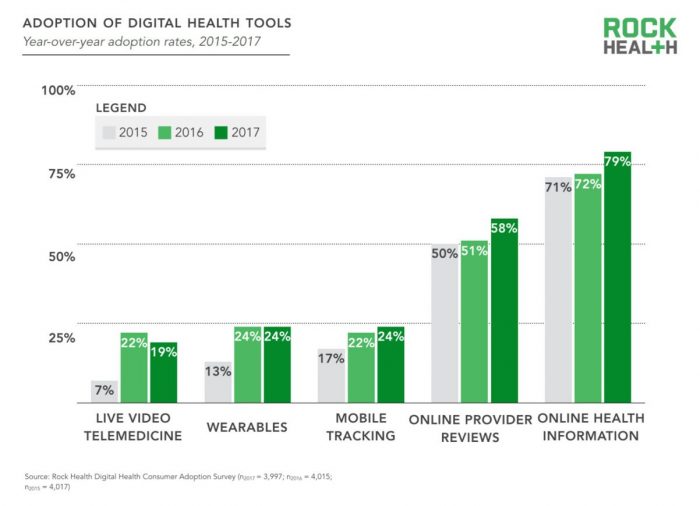
Looking for health information online is just part of being a normal, mainstream health consumer, according to the third Rock Health Digital Health Consumer Adoption Survey published this week. By 2017, 8 in 10 U.S. adults were online health information hunters. Six in 10 Americans looked for reviews of healthcare providers online, another new-normal consumer digital health activity. But only one in four people had used wearable technology for health, and one in five had participated in a live video telemedicine encounter. The Rock Health team observes that “the needle has not moved equally across every type of digital health solution.” Thus the
Patients have ambitious health goals, and look to doctors for help

Consumers have health goals across many dimensions, topped with eating well, getting fit, reducing stress, sleeping better, feeling mentally well, and improving personal finances. That’s an ambitious health-and-wellness list, identified in the Health Ambitions Study, the first such research Aetna has published. Six in ten people are looking to food and nutrition for health, whether as “medicine” to deal with chronic conditions, for weight loss or general wellness, which is a frequent theme here on Health Populi. Consumers embrace their food habits as a key self-care determinant of health. Fitness, cited by most consumers, is also a can-do, self-powered activity
Healthcare EveryWhere: Philips and American Well Streamline Telehealth

Two mature companies in their respective healthcare spaces came together earlier this month to extend healthcare services where patients live and doctors work, via telehealth services. Philips, celebrating 127 years in business this year, has gone all-in on digital health across the continuum of care, from prevention and healthy living to the ICU and hospital emergency department. American Well is among the longest operating telehealth companies, founded in 2006. Together, these two established organizations will transcend physician offices and ERs and deliver virtual care in and beyond the U.S. I had the opportunity to sit down with Ido Schoenberg, MD,
Hug Your Physician: S/He Needs It – Listening to the 2018 Medscape National Physician Burnout & Depression Report

Two in five U.S. physicians feels burned out, according to the Medscape National Physician Burnout & Depression Report for 2018. This year, Medscape explicitly adds the condition of “depression” to its important study, and its title. In 2017, the Medscape report was about bias and burnout. Physicians involved in primary care specialties and critical care are especially at-risk for burnout, the study found. One in five OBGYNs experience both burnout and depression. Furthermore, there’s a big gender disparity when it comes to feeling burned out: nearly one-half of female physicians feel burnout compared with 38% of male doctors. Being employed by
The Cloud’s Growing Role in Consumer-Pharma Health Engagement

The pharmaceutical industry is facing a multitude of political, regulatory, and financial uncertainties in and beyond 2018. But there’s one thing I know for sure about pharma’s morphing business model: it’s that patients are playing a growing role in the industry’s future well-being. That is, if the industry can meet health consumers where they want to be met. Patients want more communication and support from pharma companies, a new study from Accenture found. In fact, over one-third of patients tell their health care providers about pharma patient-service programs: this chart from Accenture’s study illustrates the top seven ways providers hear





 Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors.
Interviewed live on BNN Bloomberg (Canada) on the market for GLP-1 drugs for weight loss and their impact on both the health care system and consumer goods and services -- notably, food, nutrition, retail health, gyms, and other sectors. Thank you, Feedspot, for
Thank you, Feedspot, for  As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...
As you may know, I have been splitting work- and living-time between the U.S. and the E.U., most recently living in and working from Brussels. In the month of September 2024, I'll be splitting time between London and other parts of the U.K., and Italy where I'll be working with clients on consumer health, self-care and home care focused on food-as-medicine, digital health, business and scenario planning for the future...