The US Covered Nearly 50% of Global Oncology Medicine Spending in 2017 – a market update from IQVIA

“We are at a remarkable point of cancer treatment,” noted Murray Aitken, Executive Director, IQVIA Institute for Human Data Science, in a call with media this week. 2017 was a banner year of innovative drug launches in oncology, Aitken coined, with more drugs used more extensively, driving improved patient for people dealing with cancer. This upbeat market description comes out of a report on Global Oncology Trends 2018 from the IQVIA Institute for Human Data Science. The subtitle of the report, “Innovation, Expansion and Disruption,” is appropriately put. The report covers these three themes across four sections: advances in therapies,
The U.S. is a Nation in Pain – America’s Life Expectancy Fell Again in 2016
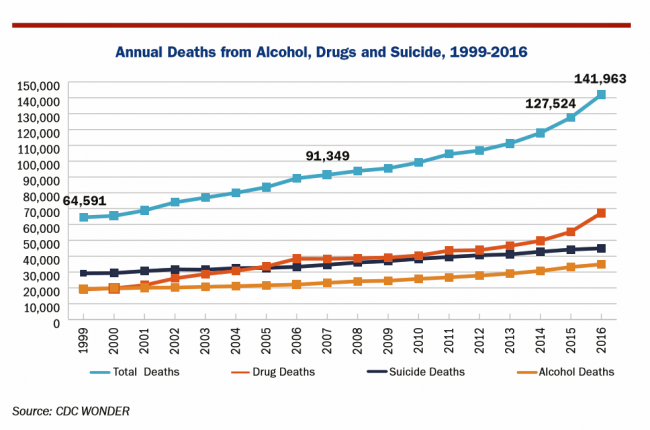
American saw the greatest number of deaths from suicide and alcohol- and drug-induced fatalities was recorded in 2016. That statistic of nearly 142,000 equates to deaths from stroke and exceed the number of deaths among Americans who died in all U.S. wars since 1950, according to Pain in the Nation Update from the Well Being Trust and Trust for America’s Health. The line graph soberly illustrates the growing tragic public health epidemic of mortality due to preventable causes, those deaths of despair as Anne Case and Sir Angus Deaton have observed in their research into this uniquely all-American phenomenon. While this
Having Health Insurance Is a Social Determinant of Health: the implications of growing uninsured in the U.S.
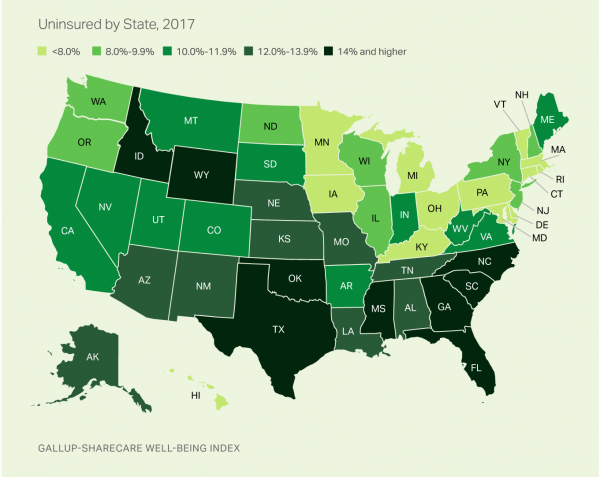
The rolls of the uninsured are growing in America, the latest Gallup-Sharecare Poll indicates. The U.S. uninsurance rate rose to 12.2% by the fourth quarter of 2017, up 1.3 percentage points from the year before. 2017 reversed advancements in health insurance coverage increases since the advent of the Affordable Care Act, and for the first time since 2014 no states’ uninsured rates fell. The 17 states with declines in insurance rates were Arizona, Colorado, Florida, Hawaii, Illinois, Indiana, Iowa, Missouri, New Mexico, New York, North Carolina, South Carolina, Texas, Utah, Washington, West Virginia, Wisconsin, and Wyoming. Among these, the greatest
Universal Health Care and Financial Inclusion – Two Sides of the Wellness Coin

Two weeks in a row, The Economist, the news magazine headquartered in London, included two special reports stapled into the middle of the magazines. Universal health care was covered in a section on 28 April 2018, and coverage on financial inclusion was bundled into the 5th May edition. While The Economist’s editors may not have intended for these two reports to reinforce each other, my lens on health and healthcare immediately, and appreciatively, connected the dots between healthcare coverage and financial wellness. The Economist, not known for left-leaning political tendencies whatsoever, lays its bias down on the cover of the section here: universal healthcare
Re-Imagining Healthcare – a Lesson from Von Clausewitz in the Fog of War

When you’re on the battlefield and you can’t see what lies ahead, go high, recommended General Von Clausewitz in his book, On War. I paraphrase this prescription from the good General-strategist’s book, On War — “War is the realm of uncertainty; three-quarters of the factors on which action in war is based are wrapped in a fog of greater or lesser uncertainty. A sensitive and discriminating judgment is called for; a skilled intelligence to scent out the truth.” Governor Mark Leavitt, who held the post of Secretary of Health and Human Services under President Bush, offered this advice at the recent Liberation
Pharma Spending Gone Bipolar: Generics At One End, Specialty Drugs on the Other
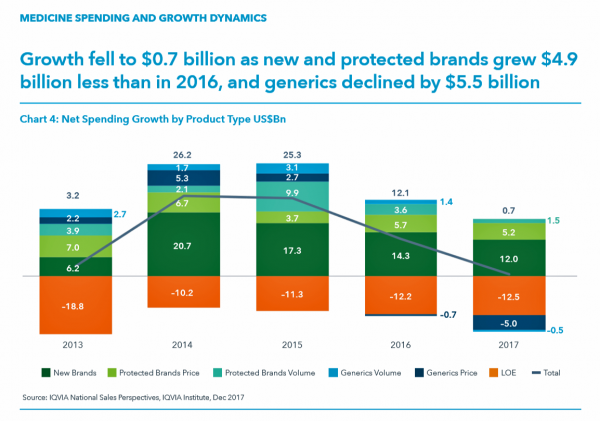
While the use of medicines continues to rise in the U.S., spending grew by only 0.6% in 2017 after accounting for discounts and rebates. In retail and mail-order channels, net spending fell by 2.1%. Prescription drug spending on branded products grew nearly $5 billion less than in 2016; generic drug spending fell by $5.5 billion, according to Medicine Use and Spending in the U.S., a report from the IQVIA Institute for Health Data Science. The report reviews medicines spending in 2017 looking forward to 2022. There were over 5.8 billion prescriptions dispensed in 2017, and generic drugs accounted 90% of
Healthcare Access and Cost Top Americans’ Concerns in Latest Gallup Poll

Healthcare — availability and affordability — is a more intense worry for Americans in March 2018 than crime and violence, Federal spending, guns, drug use, and hunger and homelessness. The Gallup Poll, fielded in the first week of March 2018, found that peoples’ overall economic and employment concerns are on the decline since 2010, at the height of the Great Recession which began in 2008. While 70% of Americans were worried about economic matters in 2010, only 34% of people in the U.S. were worried about the economy, and 23% about unemployment, in March 2018. Gallup has asked this “worry”
How We Spend Versus What We Get: America’s Healthcare Spending Makes for Poor Health
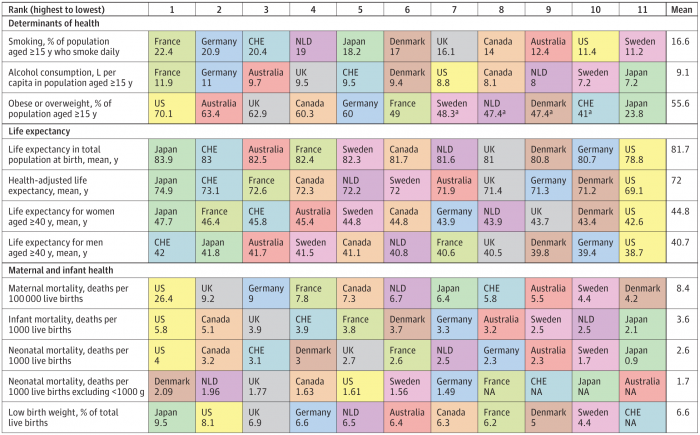
The U.S. spent nearly twice as much as other wealthy countries on healthcare, mostly due to higher prices for both labor and products (especially prescription drugs). And, America spends more on administrative costs compared to other high-income countries. What do U.S. taxpayers get in return for that spending? Lower life spans, higher maternal and infant mortality, and the highest level of obesity and overweight among our OECD peer nations. These sobering statistics were published in Health Care Spending in the United States and Other High-Income Countries this week in JAMA, the Journal of the American Medical Association. The study analyzes
Patient Privacy And Cyber In-Security at HIMSS 2018
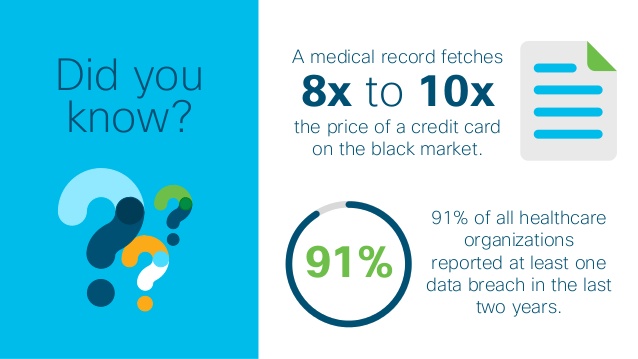
Nearly one-half of Americans experienced a personal data breach in the past three years, the third annual national cybersecurity survey found. Ensuring privacy and cybersecurity should become integrated into the healthcare industry’s consideration of a patient’s consumer experience. This makes sense, given that privacy and cybersecurity ranked the second highest priority to hospitals and healthcare providers polled in HIMSS 2018 Healthcare Leadership Survey. Providers put patient safety as #1. Appropriately, privacy and security were hot topics at HIMSS Annual Conference this year, in respond to providers’ demands for more education and concerns around the challenges. Let’s put these concerns in
Majority Rules? The Right to Affordable Health Care is A Right for All Americans
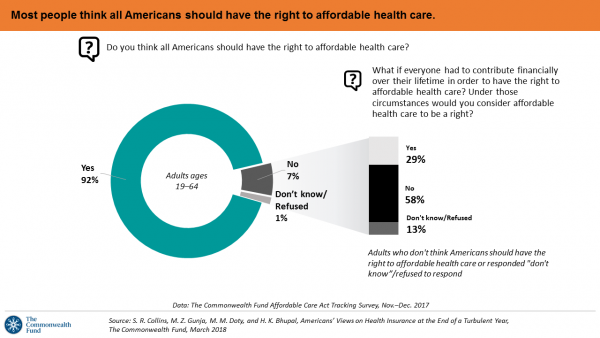
If we’re playing a game of “majority rules,” then everyone in America would have the right to affordable health care, according to a new poll from The Commonwealth Fund. The report is aptly titled, Americans’ Views on Health Insurance at the End of a Turbulent Year. The Fund surveyed 2,410 U.S. adults, age 19 to 64, by phone in November and December 2017. This is the sixth survey conducted by the Fund to track Americans’ views of the Affordable Care Act; the first survey was fielded in mid-to-fall 2013. 9 in 10 working-age adults say “yes” indeed, my fellow Americans
Add Behavioral Data to Social Determinants For Better Patient Understanding
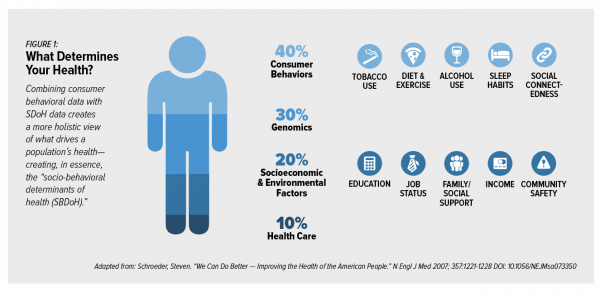
“Health agencies will have to become at least as sophisticated as other consumer/retail industries in analyzing a variety of data that helps uncover root causes of human behavior,” Gartner recommended in 2017. That’s because “health” is not all pre-determined by our parent-given genetics. Health is determined by many factors in our own hands, and in forces around us: physical environment, built environment, and public policy. These are the social determinants of health, but knowing them even for the N of 1 patient isn’t quite enough to help the healthcare industry move the needle on outcomes and costs. We need to
A Tale of Two States: Idaho, Limiting Health Plan Benefits; and Oregon, Moving Toward Universal Health Care
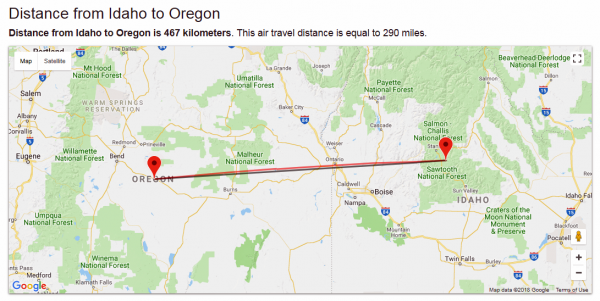
The United States don’t feel very united these days on a whole range of issues. But today, I’m struck by a 180-degree-apart chasm between Idaho and Oregon. While the centers of these two states only lie 290 miles from each other, they are worlds apart when it comes to their views on their residents as health citizens. Idaho. First, let’s travel to Idaho, aka the Gem State due to its rich endowment of natural resources. Health insurers in the state are now allowed to offer plans with limited benefits, escaping the rules for plans in the Affordable Care Act that
The $4 Trillion Health Economy of 2020
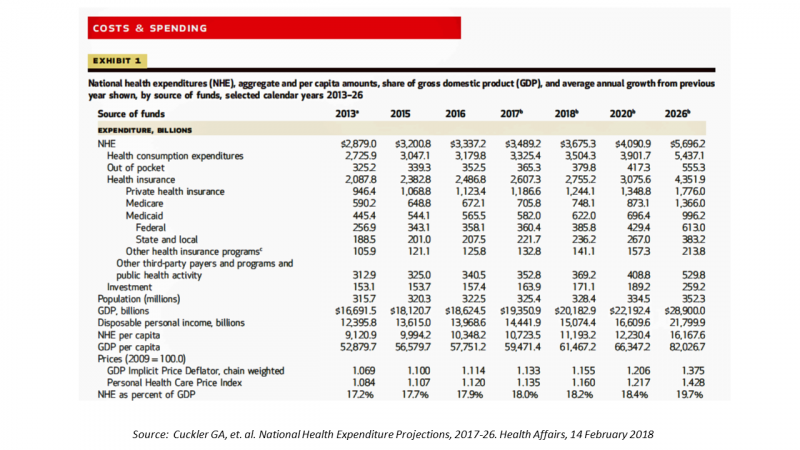
In 2020, national health expenditures (NHE) in the United States will exceed $4 trillion to cover 334.5 million Americans. That equates to 18.4% of the Gross Domestic Product (GDP) and $12,230.40 of health spending per person. I sat in on a press call today with researchers from the Office of the Actuary working in the Centers for Medicare and Medicaid Services (CMS) to review the annual forecast of the NHE, published in Health Affairs in a statistically-dense eleven page article titled, National Health Expenditure Projections, 2017-2026: Despite Uncertainty, Fundamentals Primarily Drive Spending Growth. What are those “fundamentals” pushing up healthcare spending?
Getting Real About Social Determinants of Health
New research points out that real people live real lives, and our assumptions about social determinants of health (SDOH) may need to be better informed by those real lives. I read three reports in the past week sobering up my bullish #SDOH ethos dealing with food deserts, transportation, and health service access — three key social determinants of health. To remind you about the social determinants, here’s a graphic from Kaiser Family Foundation that summarizes the key pillars of SDOH. Assumption 1: Food deserts in and of themselves diminish peoples’ healthy nutrition lifestyles. Low-income households who are exposed to the same food-buying
The United States of Care Launches to Promote Healthcare for All of US

Let’s change the conversation and put healthcare over politics. Sounds just right, doesn’t it? If you’re reading Health Populi, then you’re keen on health policy, health economics, most of all, patients: now playing starring roles as consumers, caregivers, and payors in their own care. Andy Slavitt, former Acting Administrator of the Centers for Medicare and Medicaid Services (CMS), has assembled a diverse group of health care leaders who care about those patients/people, too, appropriately named the United States of Care. Founders include Dr. Bill Frist, former Republican U.S. Senator from Tennessee, Dave Durenberger, former Republican U.S. Senator from Minnesota, and
The 2018 Edelman Trust Barometer – What It Means for Health/Care in America

Trust in the United States has declined to its lowest level since the Edelman Trust Barometer has conducted its annual survey among U.S. adults. Welcome to America in Crisis, as Edelman brands Brand USA in 2018. In the 2018 Edelman Trust Barometer, across the 28 nations polled, trust among the “informed public” in the U.S. “plunged,” as Edelman describes it, by 23 points to 45. The Trust Index in America is now #28 of 28 countries surveyed (that is, rock bottom), dropping below Russia and South Africa. “The public’s confidence in the traditional structures of American leadership is now fully
Most Americans Say Healthcare is #1 Policy Issue Entering 2018

Concerns about health care are, by a large margin, the top domestic policy issue U.S. voters identified as they enter 2018. The proportion of Americans citing healthcare as the top public agenda priority grew by 50% since 2016, from 31% two years ago to 48%. Taxes rank #2 this year, garnering 31% of Americans’ concerned, followed by immigration, which has remained flat cited by about one-in-four Americans. The Associated Press (AP)-NORC Center for Public Affairs Research polled 1,444 U.S. adults 18 and over between November 30 and December 4, 2017 for this survey. While one-half of Americans would like the
Nurses Rate Highest for Ethics in American Professions Once Again in Gallup Poll
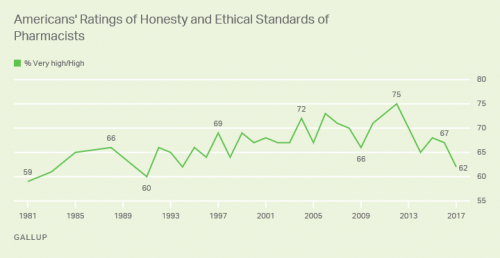
Nurses working in the U.S. are number one when it comes to ethics and honesty, the Gallup Poll found for the sixteenth year in a row. After nurses, military officers, grade school teachers, medical doctors and pharmacists rank second through fifth in ethical-line behind top-rated nursing. It’s important to note that consumers have ranked pharmacists and doctors in second and third place in this annual survey for many years. This year, both professions fall below the military and teachers. Nurses have been #1 in this study every year since Gallup launched the survey in 1999, except for 2001 when firefighters topped
Health Consumers Face the New Year Concerned About Costs, Security and Caring – Health Populi’s 2018 Forecast
As 2018 approaches, consumers will gather healthy New Year’s Resolutions together. Entering the New Year, most Americans are also dealing with concerns about healthcare costs, cybersecurity, and caring – for physical health, mental stress, and the nation. Healthcare costs continue to be top-of-mind for consumer pocketbook issues. Entrenched frugality is the new consumer ethos. While the economy might be statistically improving, American consumers’ haven’t regained confidence. In 2018, frugality will impact how people look at healthcare costs. 88% of US consumers are likely to consider cost when selecting a healthcare provider, a Conduent survey found. Physicians know this: 81% of
Support for the Affordable Care Act the Highest Since Passage
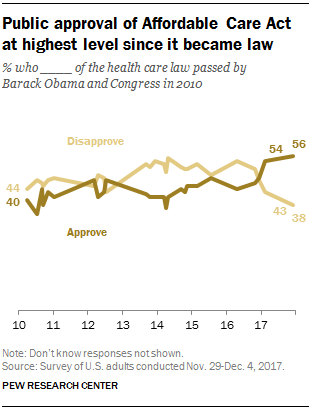
Americans’ approval of the Affordable Care Act reached its apex in December 2017, the Pew Research Center found. The proportion of people approving the ACA has been growing since the middle of 2016, now at 56% of the public. The timing of this survey, conducted at the end of November and first few days of December 2017, coincides with Congress’s arm-wrestling a tax bill that would eliminate the individual mandate for health insurance which is an ACA building block for universal coverage in the United States. Most people in the U.S. also believe that the ACA has had a positive
The Patient as Payor – Consumers and the Government Bear the Largest Share of Healthcare Spending in America
The biggest healthcare spenders in the United States are households and the Federal government, each responsible for paying 28% of the $3.3 trillion spent in 2016. Private business — that is, employers covering healthcare insurance — paid for 20% of healthcare costs in 2016, based on calculations from the CMS Office of the Actuary’s report on 2016 National Health Expenditures. The positive spin on this report is that overall national health spending grew at a slower rate in 2016, at 4.3% after 5.8% growth in 2015. This was due to a decline in the growth rates for the use of
Six Healthcare News Stories to Keep Hospital CFOs Up At Night
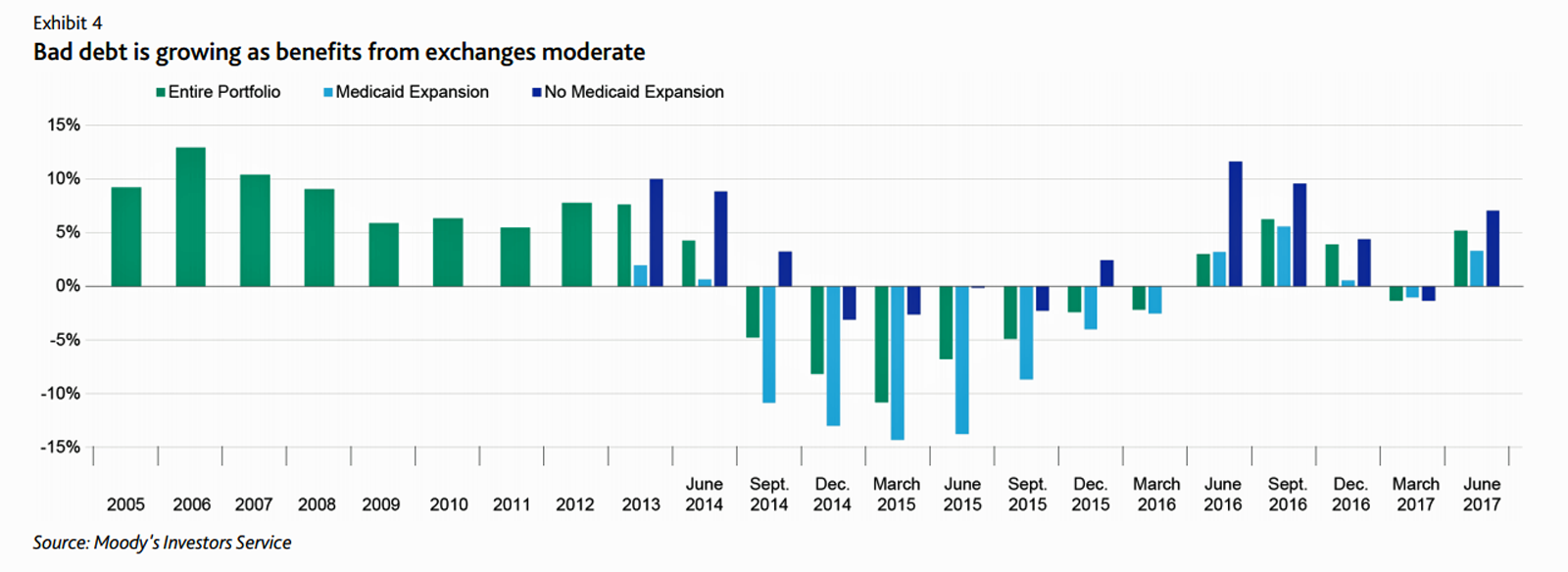
At this moment, the healthcare job I’d least like to have is that of a non-profit hospital Chief Financial Officer (CFO). Five news stories, published in the past 24 hours, tell the tale: First, Moody’s forecast for non-profit hospitals and healthcare in 2018 is negative due to reimbursement and expense pressures. The investors report cited an expected contraction in cash flow, lower reimbursement rates, and rising expense pressures in the midst of rising bad debt. Second, three-quarters of Federally Qualified Health Centers plan to lay off staff given lack of budget allocations resulting from Congressional inaction. Furthermore, if the $3.6
Don’t Touch My Entitlements to Pay For Tax Reform, Most Americans Say to Congress
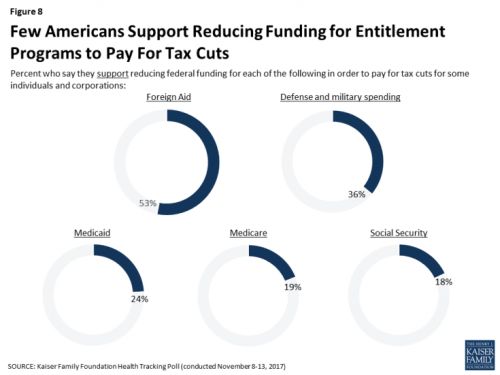
To pay for tax cuts, take money from foreign aid if you must, 1 in 2 Americans say. But do not touch my Medicaid, Medicare, or Social Security, insist the majority of U.S. adults gauged by the November 2017 Kaiser Health Tracking Poll. This month’s survey looks at Americans’ priorities for President Trump and the Congress in light of the GOP tax reforms emerging from Capitol Hill. While reforming taxes is considered a top priority for the President and Congress by 3 in 10 people, two healthcare policy issues are more important to U.S. adults: first, 62% of U.S. adults
U.S. Healthcare Spending & Outcomes in Five Charts: #EpicFail in the 2017 OECD Statistics
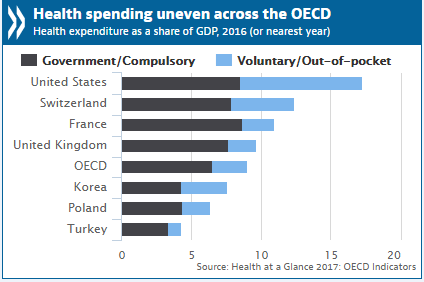
“Spend more. Get less.” If a retailer advertised using these four words, how many consumers would buy that product or service? This is the American reality of healthcare spending in 2016, told in the OECD report, Health at a Glance 2017. I present five charts from the study in this post, which together take the current snapshot health-economic lesson for the U.S. First, look at health expenditures as a share of gross domestic product: the U.S. is number one above Switzerland, France, and the UK, and about two times the OECD average. Note, too, the proportion of out-of-pocket and so-called
Health Care Is 2.5 More Expensive Than Food for the Average U.S. Family
The math is straightforward. Assume “A” equals $59.039, the median household income in 2016. Assume “B” is $18,142, the mean employer-sponsored family insurance premium last year. B divided by A equals 30.7%, which is the percent of the average U.S. family’s income represented by the premium cost of health insurance. Compare that to what American households spent on food: just over $7,000, including groceries and eating out (which is garnering a larger share of U.S. eating opportunities, a topic for another post). Thus, health care represents, via the home’s health insurance premium, represents 2.5 times more than food for the
Income Inequality For Older Americans Among Highest in the World – What This Means for Healthcare
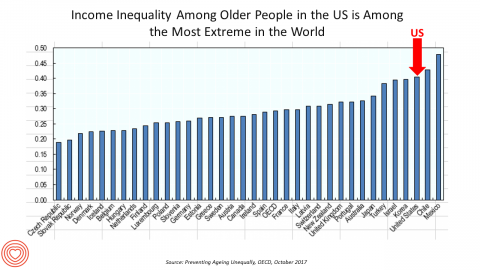
Old-age inequality among current retirees in the U.S. is already greater than in ever OECD country except Chile and Mexico, revealed in Preventing Ageing Unequally from the OECD. Key findings from the report are that: Inequalities in education, health, employment and income start building up from early ages At all ages, people in bad health work less and earn less. Over a career, bad health reduces lifetime earnings of low-educated men by 33%, while the loss is only 17% for highly-educated men Gender inequality in old age, however, is likely to remain substantial: annual pension payments to the over-65s today are
What Patients Feel About Technology, Healthcare Costs and Social Determinants
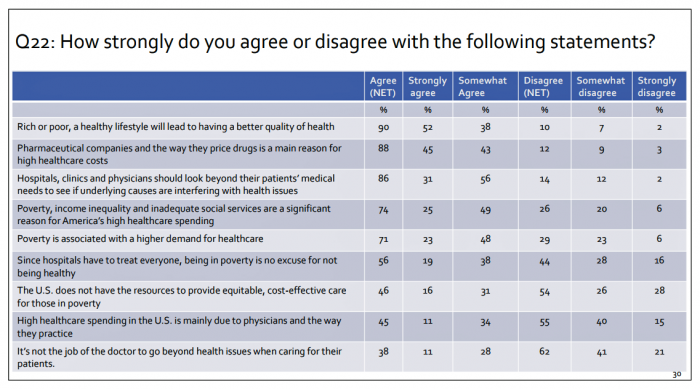
U.S. consumers feel positive about the roles of technology and social determinants in improving healthcare, but are concerned about costs, according to the 2017 Patient Survey Report conducted for The Physicians Foundation. The survey gauged patients’ perspectives across four issues: the physician-patient relationship, the cost of healthcare, social determinants of health, and lifestyle choices. Two key threads in the research explain how Americans feel about healthcare in the U.S. at this moment: the role of technology and the cost of health care. First, the vast majority of consumers view technology, broadly defined, as important for their health care. 85% of people
A Lesson in Healthcare Data Distrust, Brought to Us By Aetna
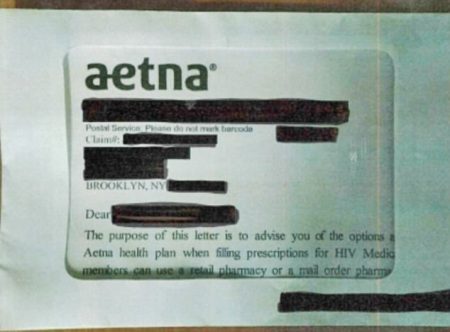
The importance of trust in healthcare cannot be overestimated. Trust underpins peoples’ health engagement. Trust eroded repels people from seeking necessary health care services. So what do we make of Aetna’s appalling breach of patient privacy when the health insurer, whose 23 million members sign HIPAA agreements, sent a letter to some 12,000 members who are managing HIV….and the envelope in which these letters were mailed had a glassine window that exhibited the advisory showing the words, “The purpose of this letter is to advise you of the options…Aetna health plan when filling prescriptions for HIV Medic….members can use a
Women’s Access to Health Care Improved Under the Affordable Care Act
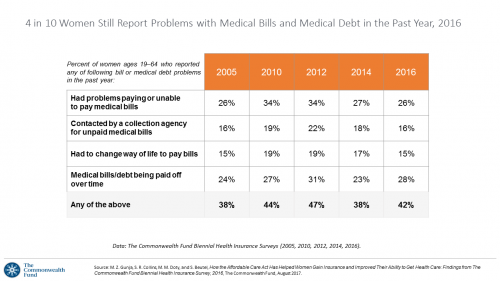
The Affordable Care Act (ACT) was implemented in 2010. Since the inception of the ACA, the proportion of uninsured women in the U.S. fell by nearly one-half, from 19 million in 2010 to 11 million in 2016. The Commonwealth Fund has documented the healthcare gains that American women made since the ACA launch in their issue brief, How the Affordable Care Act Has Helped Women Gain Insurance and Improved Their Ability to Get Health Care, published earlier this month. The first chart talks about insurance: health care plan coverage, which is the prime raison d’être of the ACA. It’s
Loneliness and Isolation Kill: Health Depends on Purpose
In the U.S., one-third of people age 65 and over have difficulty walking 3 city blocks. Hold that thought, and consider the role of purpose in life: purpose drives well-being, inoculating one’s life with meaning, direction, and goals, as the On Purpose guru Victor Strecher explains in his amazing graphic manifesto. Having a higher sense of purpose in life is associated with higher probability of people engaging in healthier behaviors, such as greater physical activity and seeking preventive healthcare; better biological functioning; and, lower risk of disease. Four researchers from the Harvard School of Public Health connected the dots between
Healthcare Quality and Access Disparities Persist in the U.S.
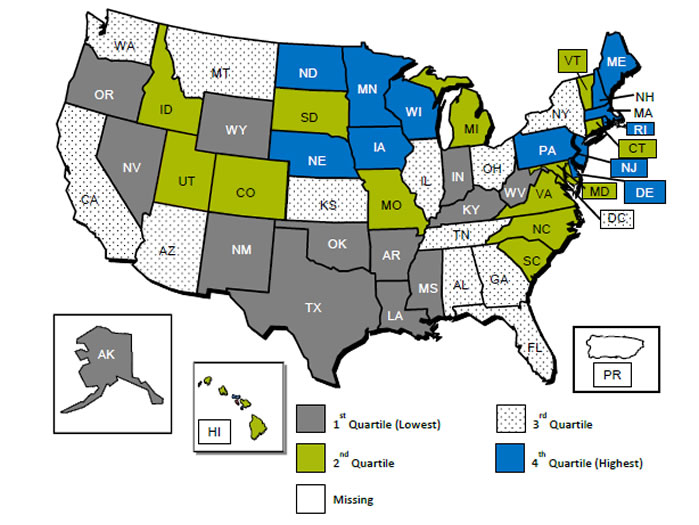
In 2015, poor and low-income people in America had worse health care than high-income households; care for nearly half of the middle-class was also worse than for wealthier families. Welcome to the 2016 National Healthcare Quality and Disparities Report from the Agency for Healthcare Research and Quality (AHRQ). The report assesses many measures quantifying peoples’ access to health care, such as uninsurance rates (which improved between 2010 and 2016), and quality of health care — including person-centered care, patient safety, healthy living, effective treatment, care coordination, and care affordability. While some disparities lessened between 2000 and 2015, disparities
Most Americans, Including Republicans, Want President Trump’s Administration to Make the ACA Work – Not Fail
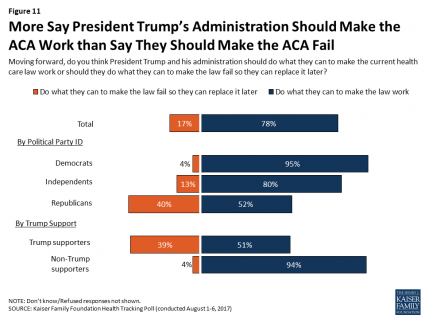
8 in 10 Americans want President Trump and his administration to do what they can to make the Affordable Care Act work, according to the latest August 2017 health tracking poll from Kaiser Family Foundation (KFF). By political party affiliation, this includes 95% of Democrats, 80% of Independents, and 52% of Republicans (that is, to emphasize the point, just over half, a majority, of Republicans). More Americans are also relieved and happy, versus disappointed and angry, that the ACA repeal did not occur (thus far), the second chart illustrates. To be sure, a majority of Republicans register anger and disappointment,
Health Equity Lessons from July 23, 1967, Detroit
On July 23, 1967, I was a little girl wearing a pretty dress, attending my cousin’s wedding at a swanky hotel in mid-town Detroit. Driving home with my parents and sisters after the wedding, the radio news channel warned us of the blazing fires that were burning in a part of the city not far from where we were on a highway leading out to the suburbs. Fifty years and five days later, I am addressing the subject of health equity at a speech over breakfast at the American Hospital Association 25th Annual Health Leadership Summit today. In my talk,
Fix the ACA, Most Americans Say
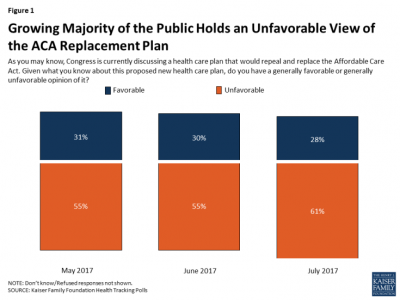
61% of Americans hold negative views of repealing-and-replacing the Affordable Care Act, according to the July 2017 Health Tracking Poll from the Kaiser Family Foundation. This month’s survey focused on Americans’ views on Republican legislative efforts to repeal and replace the Affordable Care Act (ACA). As of the writing of this post, the majority of the Senate rejected the full repeal of the ACA, but the situation is very fluid. Note that this poll was conducted by phone between July 5-10, 2017, among 1,183 U.S. adults ages 18 and older. The column chart here illustrates that the proportion of people
Weaving Accenture’s Five Digital Health Technology Trends for 2017

Technology should serve people, and Accenture has identified five major key trends that, together, could forge a person-centered, -friendly, -empowering healthcare system. This is Accenture’s Digital Health Technology Vision for 2017. “Should” and “could” are the important adverbs here, because if tech doesn’t deliver, driving efficiency and effectiveness, personalizing medical treatments, and inspiring people to become more health literate and health-engaging, then tech is just a Field of Dreams being built and available, with no people taking advantage of the potential benefits. The five new-new tech trends are: AI is the new UI, where healthcare experience is everything Ecosystem power
Self-Pay Healthcare Up, Hospital Revenues Down
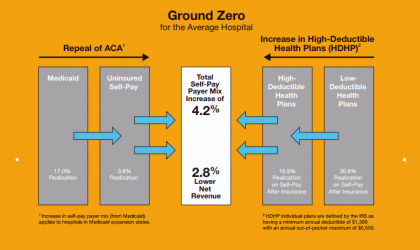
For every 4.2% increase in a hospital’s self-pay patient population, the institution’s revenues would fall by 2.8% in Medicaid expansion states. This is based on the combination of a repeal of the Affordable Care Act and more consumers moving to high-deductible health plans. That sober metric was calculated by Crowe Horwath, published in its benchmarking report published today with a title warning that, Self-Pay Becomes Ground Zero for Hospital Margins. The “ground zero” for the average U.S. hospital is the convergence of a potential repeal of the Affordable Care Act (ACA), which could increase the number of uninsured Americans by 22 million
Is There Political Will for Healthcare Access in the US?
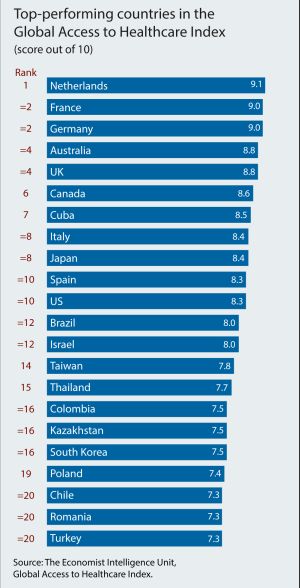
The Netherlands, France and Germany are the best places to be a patient, based on the Global Access to Healthcare Index, developed by the Economist Intelligence Unit (EIU). Throughout the world, nations wrestle with how to provide healthcare to health citizens, in the context of stretched government budgets and demand for innovative and accessible services. The Global Access to Healthcare Index gauges countries’ healthcare systems in light of peoples’ ability to access services, detailed in Global Access to Healthcare: Building Sustainable Health Systems. The United States comes up 10th in line (tied with Spain) in this analysis. Countries that score the
The Pursuit of Health Equity and the State of U.S. Health Care
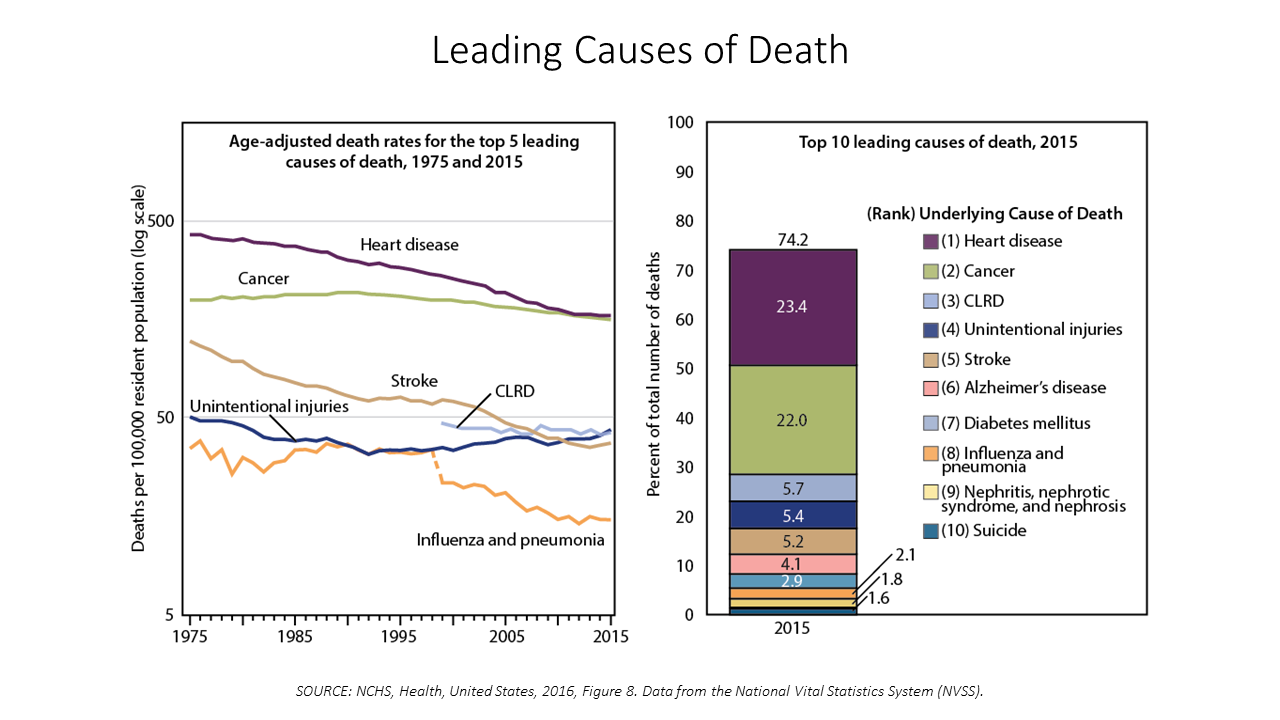
Between 2014 and 2015, death rates increased for eight of the ten leading causes; only death rates caused by cancer fell, and mortality rates for influenza and pneumonia stayed flat. The first chart paints this sobering portrait of Americans’ health outcomes, presented in the CDC’s data-rich 488-page primer, Health, United States, 2016. Think of this publication as America’s annual report on health. Every year, it is prepared and submitted to the President and Congress by the Secretary of the Department of Health and Human Services. This year’s report was delivered by DHHS Secretary Tom Price to President Trump and the
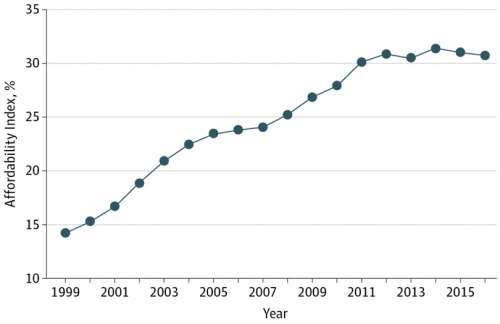
Costs of Healthcare Top Americans’ Financial Concerns: It’s Financial Health Matters Day
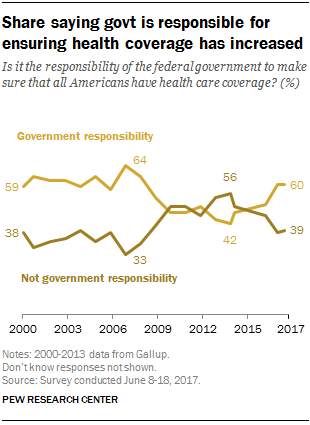
Americans are most worried about healthcare costs among all financial concerns; most people in the U.S. also believe the Federal government should ensure that all people have health coverage. Two polls published in the past week point to the fact that most U.S. health citizens are concerned about health care for themselves and their families, driving a growing proportion of people to favor a single-payer health system. The first line chart illustrates a dramatic trajectory up of the number of American identifying healthcare costs as their #1 financial problem, rising from 10% of people in 2013 to 17% in 2017.
Shopping Food for Health: the 2017 U.S. Grocery Shopper Trends
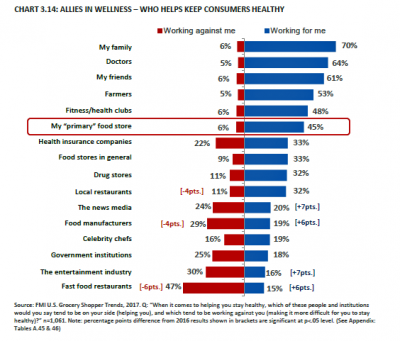
Wellness is at the grocery store, the vast majority of U.S. health citizens say. 8 in 10 U.S. shoppers are concerned about the nutritional content in the food they eat. As grocery shoppers look for more fresh and less processed foods, grocery stores are seen as trusted allies for meeting wellness needs. Grocers are coupling the growth of more healthy packaged foods in the middle of the store with more fresh and prepared food options that consumers see as healthier than restaurant meals, according to U.S. Grocery Shopper Trends 2017 from FMI (the Food Marketing Institute) and Hartman Group. While
Global Drug Sales Forecasts Fall For Next Five Years
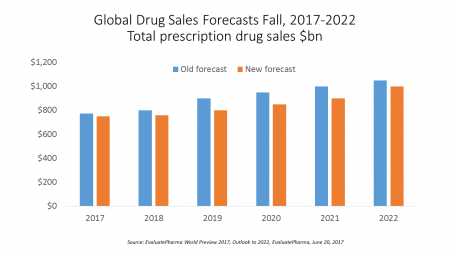
Total prescription drug sales have been trimmed, based on calculations of EvaluatePharma which forecasts a $390 bn drop in revenues between 2017 and 2022. “Political and public scrutiny over pricing of both new and old drugs is not going to go away,” EvaluatePharma called out in its report. The intense scrutiny on pharma industry pricing was fostered by Martin Shkreli in his pricing of Daraprim (taking a $13.50 product raising the price to $750), Harvoni and Sovaldi pricing for Hepatitis C therapies, and last year’s EpiPen pricing uproar. A May 2017 analysis of prescription drug costs by AARP judges that, “Nothing
Pharmacy and Outpatient Costs Will Take A Larger Portion of Health Spending in 2018
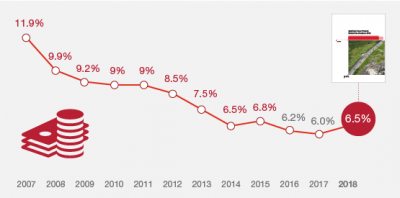
Health care costs will trend upward by 6.5% in 2018 according to the forecast, Medical Cost Trends: Behind the Numbers 2018, from PwC’s Health Research Institute. The expected increase of 6.5% is a half-percentage point up from the 2017 rate of 6.0%, which is 8% higher than last year’s rate matching that of 2014. PwC’s Health Research Institute has tracked medical cost trends since 2007, as the line chart illustrates, when trend was nearly double at nearly 12%. The research consider medical prices, health care services and goods utilization, and a PwC employer benefit cost index for the U.S. The key
Across Party Lines, Few Americans Believe the AHCA Keeps President Trump’s Healthcare Promises
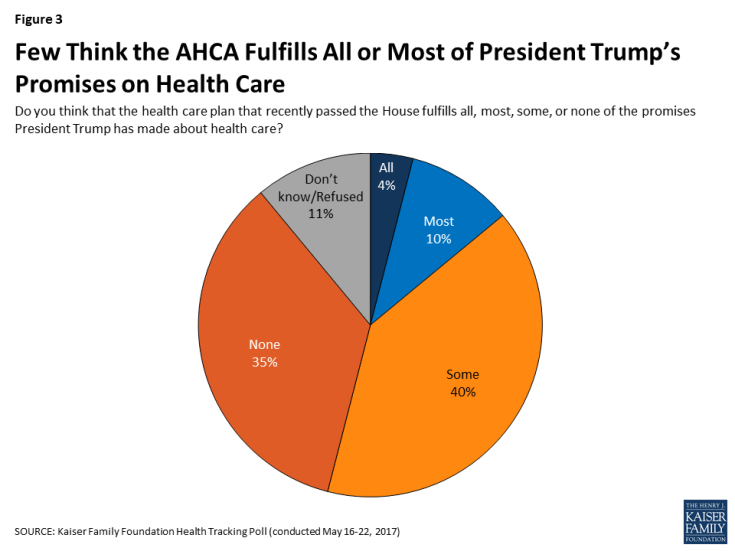
Only 14% of U.S. adults think that the American Healthcare Act (AHCA) fulfills all or most of President Trump’s campaign promises on health care, according to the May 2017 Kaiser Health Tracking Poll, released today. But political party lines surface when people area asked, overall, “given what you know about this proposed new health care plan, do you have a generally favorite or unfavorable opinion of it?” 55% of U.S. adults have an unfavorable view of the AHCA; however, the split across parties is quite clear: 84% of Democrats have an unfavorable view of the AHCA 57% of Independents ahve
A New Health Risk: Hacked Personal Medical Devices
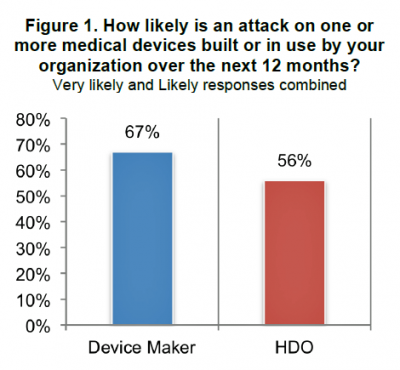
We have entered an era of insecurity in healthcare in America. While major attention is being paid to healthcare insurance and service insecurity, food insecurity and financial insecurity, there’s another one to add to this list: medical device security. As more medical devices have moved into the digital internet-connected mode, the risk for malware, ransomware, and overall hack-ability grows. This increasing and challenging risk is covered in the report, Medical Device Security: An Industry Under Attack and Unprepared to Defend from Ponemon Institute. Ponemon Institute has been tracking information security across industries, including healthcare, for several years. In this survey, sponsored
Shopping Food for Health is Mainstream, But Nutrition Confusion is Super-Sized
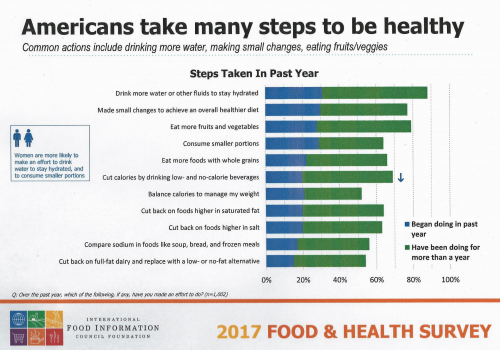
Americans are overwhelmingly keen to use food for their health, and overwhelmed by the amount of nutrition information they face to make good shopping and eating decisions. Welcome to “food confusion,” a phenomenon gleaned from the 12th Annual Food and Health Survey conducted by the International Food Information Council Foundation (IFIC). This 12th annual survey from IFIC finds that most Americans take many steps to be healthy. In the past year, the most popular health-steps include drinking more for hydration, making small changes to achieve a healthier diet, consuming smaller portions, eating more fruits and vegetables, and eating more whole grains.
Americans Say Healthcare is the Nation’s #1 Problem – Tied with Dissatisfaction with Government
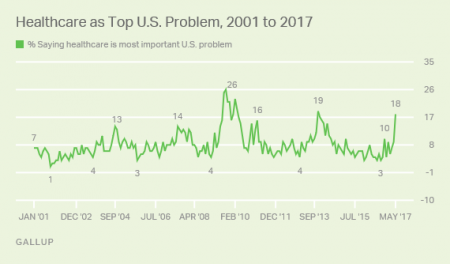
Healthcare tops the list of Americans’ concerns, tied with a dissatisfaction for government, this month (May 2017). According to a Gallup poll published 12 May, poor government leadership and healthcare are together the most important problem currently facing the U.S. Immigration, the economy, jobs, and race relations are distance 3rd places in this survey, which was conducted during the first week of May 2017 among 1,011 U.S. adults 18 years and older. The highest percent of Americans citing healthcare as America’s most important problem was 26%, found in August/September 2008 when town hall meetings round the country were protesting healthcare
Women and Children First? What the AHCA Holds for Vulnerable Populations

In accounting, there’s a rule with acronym “LIFO;” this stands for “last in, first out,” which requires taking account of the most recent cost of products being the first ones to be expensed on the ledger. I’m thinking about LIFO when it comes to the American Health Care Act (AHCA) which narrowly passed through Congress yesterday by 4 votes, with a final tally of 217 to 213. Why “LIFO?” Because long-uninsured folks who just recently received access to health insurance as an on-ramp to health care services could lose this benefit, just months after joining the ranks of the insured. Among
Medicines in America: The Half-Trillion Dollar Line Item
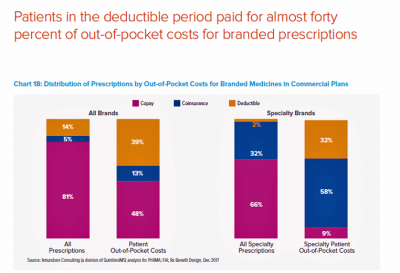
Prescription drug spending in the U.S. grew nearly 6% in 2016, reaching $450 billion, according to the QuintilesIMS Institute report, Medicines Use and Spending in the U.S., published today. U.S. drug spending is forecasted to grow by 30% over the next 5 years to 2021, amounting to $610 billion. In 2016, per capita (per person) spending on medicines for U.S. health citizens averaged $895. Specialty drugs made up $384 of that total, equal to 43% of personal drug spending, shown in the first chart. Spending on specialty drugs continues to increase as a proportion of total drug spending: traditional medicines’ share
Most Physicians Say Patients, Doctors and Hospitals Are All Losers Under Trump
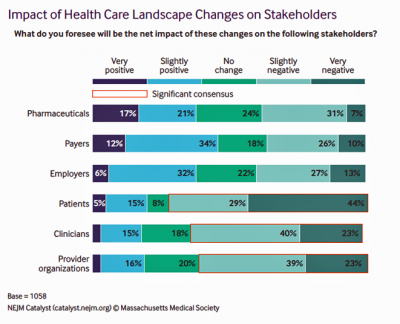
“Overall, Council members express pessimism about the health are landscape in the wake of the Trump administration’s proposed plans, citing no clear winners, only losers: patients, clinicians, and provider organizations.” This is the summary of the Leadership Survey report, Anticipating the Trump Administration’s Impact on Health Care, developed by the New England Journal of Medicine‘s NEJM Group. The first chart illustrates the “biggest healthcare losers” finding, detailed on the bottom three bars of patients, clinicians, and provider organizations. The stakeholders that will fare best under a President Trump healthcare agenda would be drug companies, payers, and employers. The biggest loser
The Power of Joy in Health and Medicine – Learning From Dr. Regina Benjamin

Former Surgeon General Dr. Regina Benjamin was the first person who quoted to me, “Health isn’t in the doctor’s office. It’s where people live, work, play and pray,” imparting that transformational mantra to me in her 2011 interview with the Los Angeles Times. I wrote about that lightbulb moment here in Health Populi. Dr. Benjamin was the 18th Surgeon General, appointed by President Obama in 2009. As “America’s Doctor,” she served a four-year term, her mission focused on health disparities, prevention, rual health, and children’s health. Today, Dr. Benjamin wears many hats: she’s the Times Picayune/NOLA.com professor of medicine at
Telehealth and Virtual Healthcare Are Mainstreaming
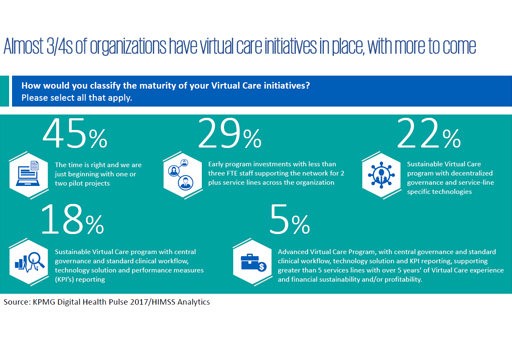
As the annual meeting of the American Telemedicine Association convenes this week in Orlando, there’s a lot of telehealth news to curate. The topline of it all: virtual healthcare is mainstreaming, with more providers, payors, and patients aligning in support of virtual health care delivery. Three-quarters of providers have some form of basic telemedicine or telehealth in place. One-third of healthcare providers use some flavor of virtual care technology in their workflow, according to research from KPMG and HIMSS Analytics summarized in the first graphic. KPMG sees virtual care options — remote patient monitoring, enhanced portals, and web interactions for patient-provider
Health Care Costs Are A Top Worry for Americans Across Political Parties
Health care costs are out-of-reach for more Americans, among both people who have insurance through the workplace or via health insurance exchanges. The first chart illustrates the growing healthcare affordability challenge for American health consumers, discussed in a data note to the Kaiser Family Foundation Health Tracking Poll in March 2017. In 2017, 43% of consumers found it difficult to meet the health care deductible before insurance would kick in 37% of consumers found it difficult to pay for the cost of health insurance each month 31% said it was difficult to pay for copayments for doctor visits and prescription drugs.
Most Americans Favor Some Flavor Of National Health Care Plan
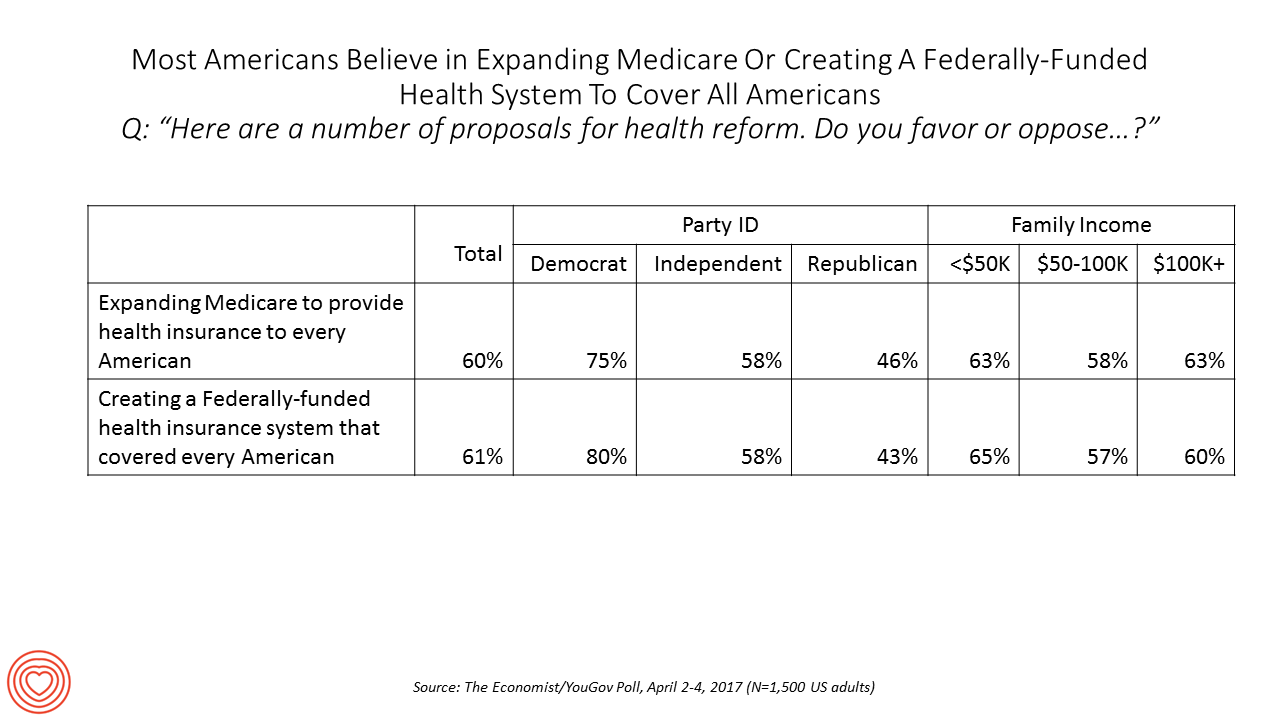
Most US adults favor some kind of national health care plan, based on an Economist/YouGov poll conducted in April 2017. Six in ten people are for expanding so-called “Medicare for All,” where the health plan that currently serves older Americans would extend to all U.S. health citizens. Six in ten people would also favor a Federally-funded health insurance system that would cover all Americans — that is, universal health care. The table details this poll question by political party identification and family income. At least 3 in 4 Democrats would be more likely to favor either of the two healthcare
Valuing Children = Valuing Health: Learning From Florence, Italy

This week I celebrate two spring holy holidays in one city that embraces spirituality, civility, and culture: Florence, Italy. Today, I had the special opportunity to tour Ospedale degli Innocenti: the Hospital of the Innocents. The hospital is now an institute for studying the culture and economics of children, and a museum telling a unique story of Florentine babies born in the early 15th century, spanning our contemporary era. The founding and root history of this beautiful place has lessons to teach us even today. It is key to realize, first, that Florentine humanism exalted the ideal virtues of the
Health Inequity in the United States – A View From Across the Pond
The statistics on the health of people living in America illustrate a divide between have’s and have-not’s. Average life expectancy is lower in the US compared with other wealthy nations: the wealthiest Americans live 10 to 15 years longer than the poorest, according to a landmark article in JAMA from 2016 studying the relationship between income inequality and mortality. See the first chart: this illustrates that people living in the US whose income reaches the top 95th percentile far outlive folks in the bottom 5th percentile of income. I find myself in London, England, this week, across the Pond (that is,
A New Risk Factor For Mental Health: Climate Change
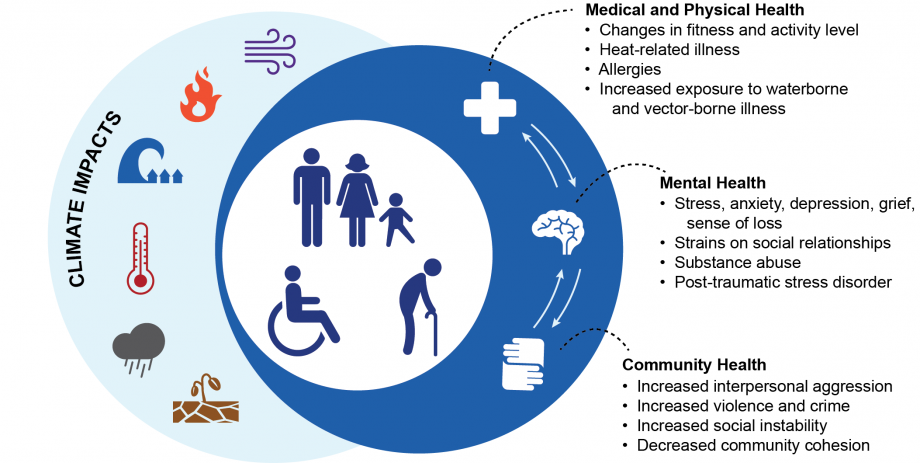
We make our health across many dimensions: via nutrition, safe physical/built environments, financial wellness, education, and the environment among them. In this last category, the environment, new research finds that climate change has a significant impact on health. The report, Mental Health and Our Changing Climate: Impacts, Implications, and Guidance, was sponsored by the American Psychological Association in conjunction with Climate for Health and ecoAmerica. “Climate change-induced severe weather and other natural disasters have the most immediate effects on mental health in the form of the trauma and shock due to personal injuries, loss of a loved one, damage to
Pharma Industry Reputation Declines Second Year In A Row
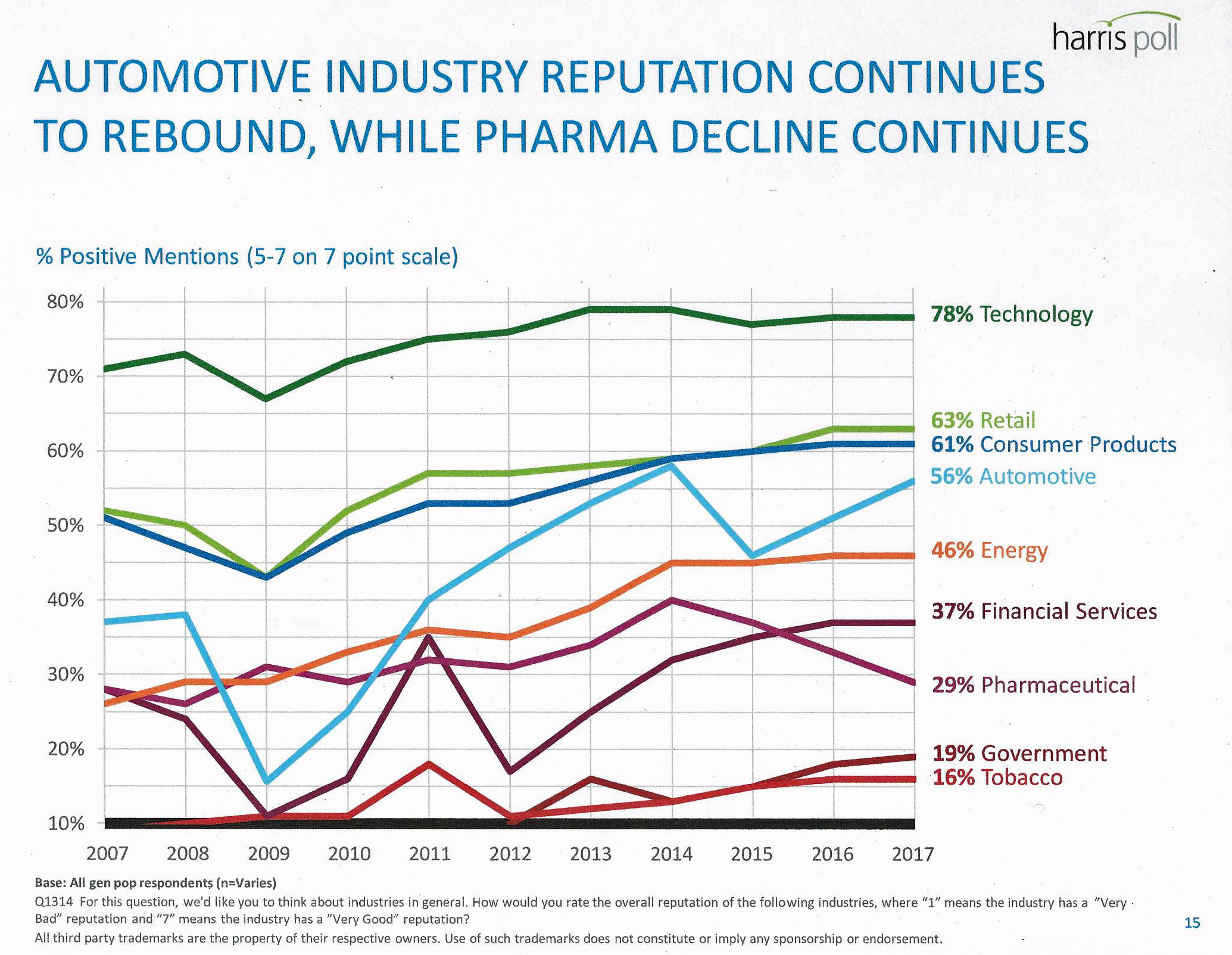
U.S. consumers love technology, retail, and consumer products; automotive company reputations are improving, even with Volkswagen’s emission scandal potentially tarnishing the industry segment. The only corporate sector whose reputation fell in 2016 was the pharmaceutical industry’s, according to the Harris Poll’s 2017 Reputation Quotient report. The line chart illustrates the decline of pharma’s reputation, which puts it on par with its consumer perceptions in 2010 — just before Medicare Part D was legislated and implemented, which improved pharma’s image among American health citizens (especially older patients who tend to be more frequent consumers of prescription drugs). Pharma’s reputation quotient is back
States That Expanded Medicaid Improved Healthcare Access & Patient Outcomes
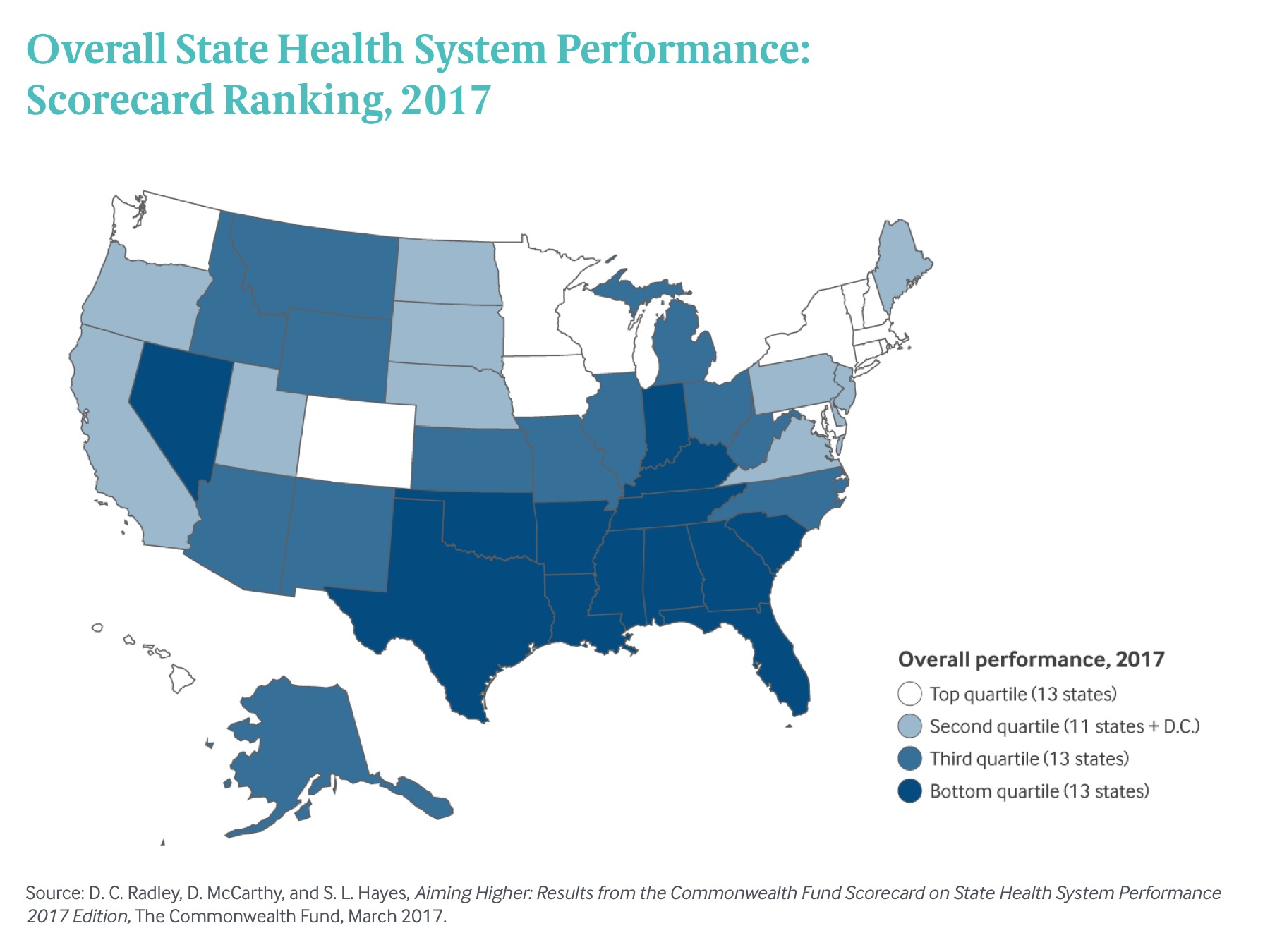
States that expanded Medicaid since the start of the Affordable Care Act made greater health system access improvements than those States that did not expand Medicaid, according to Aiming Higher: Results from the Commonwealth Fund Scorecard on State Health System Performance. There’s good news and bad news in this report: on the upside, nearly all states saw health improvements between 2013 and 2015, and in particular, for treatment quality and patient safety. Patient re-admissions to hospitals also fell in many states. But on the downside, premature deaths increased in nearly two-thirds of states, a reversal in the (improving) national mortality
Americans Are Not Sold On the American Health Care Act
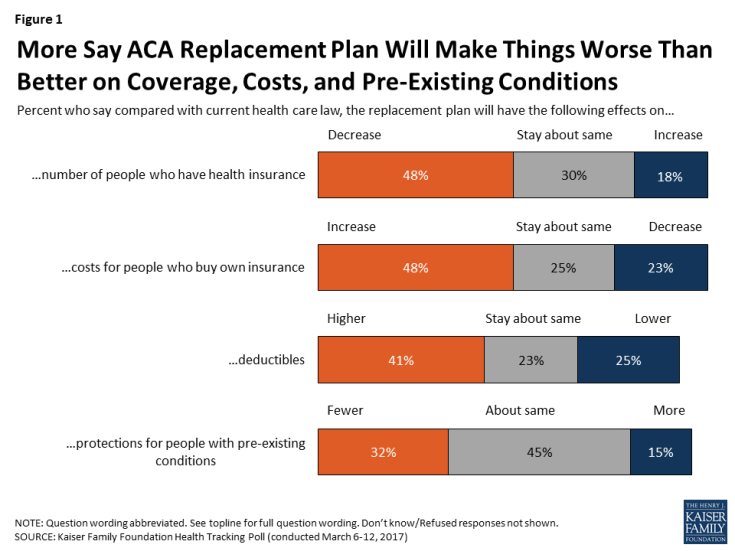
Most Americans do not believe that TrumpCare, the GOP plan to replace the Affordable Care Act (the ACA, aka ObamaCare), will make things better for U.S. health citizens when it comes to peoples’ health insurance coverage, the premium costs charged for those health plans, and protections for people with pre-existing medical conditions. The March 2017 Kaiser Family Foundation Health Tracking Poll examined U.S. adults’ initial perceptions of AHCA, the American Health Care Act, which is the GOP’s replacement plan for the ACA. There are deep partisan differences in perceptions about TrumpCare, with more Republicans favorable to the plan — although not
The Healthcare Reform Issue Americans Agree On: Lowering Rx Costs
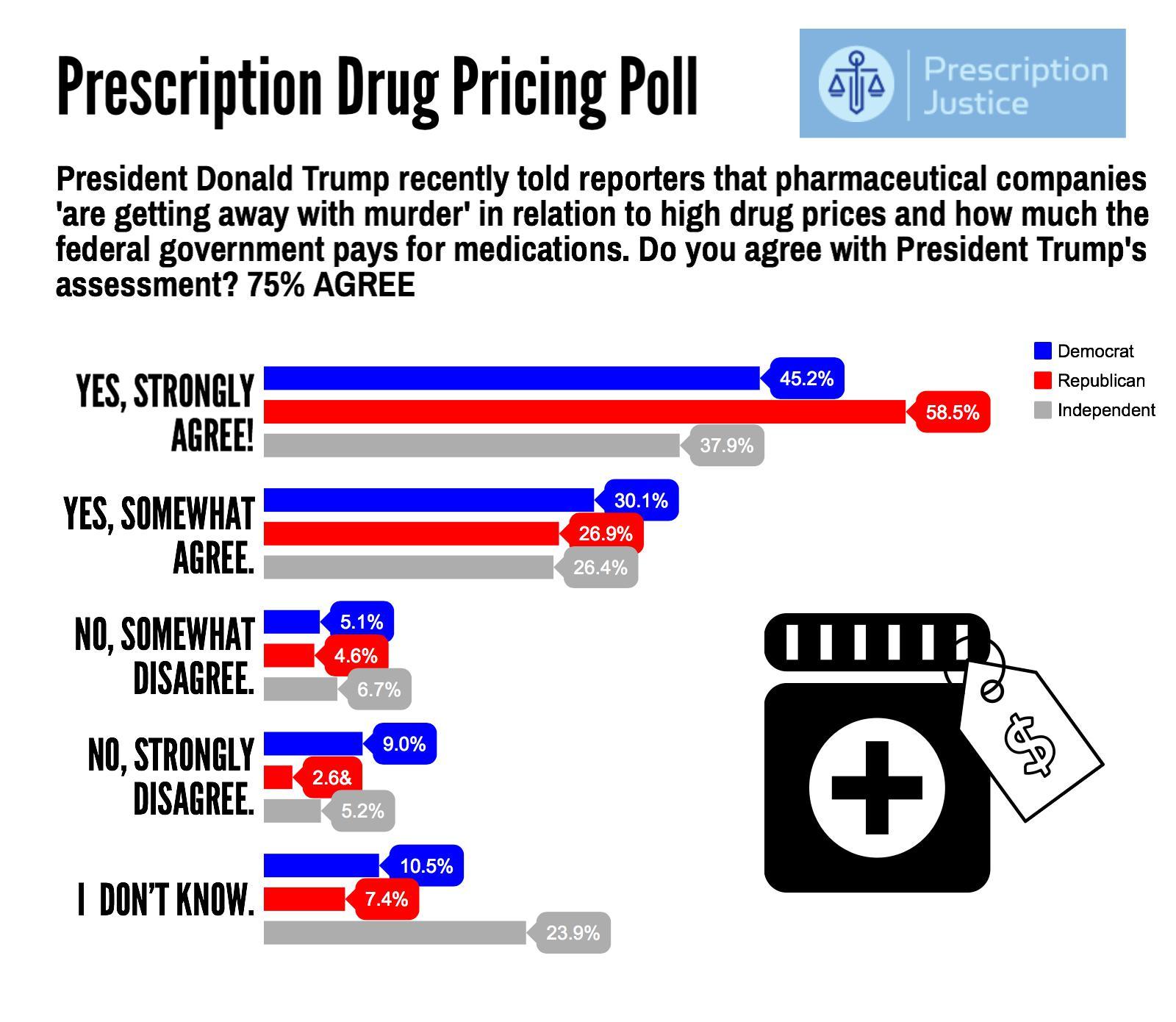
Yesterday, the Tweeter-in-Chief President Donald Trump tweeted, “I am working on a new system where there will be competition in the Drug Industry. Pricing for the American people will come way down!” Those 140 characters sent pharma stocks tumbling, as illustrated by the chart for Mylan shares dated 7 March 2017. This is one issue that Americans across the political spectrum agree on with the POTUS. The latest Zogby poll into this issue, conducted for Prescription Justice, found 3 in 4 Americans agree that pharmaceutical companies are “getting away with murder,” as President Trump said in a TIME magazine interview
Your Zip Code Is Your Wellness Address

Geography is destiny, Napoleon is thought to have first said. More recently, the brilliant physician Dr. Abraham Verghese has spoken about “geography as destiny” in his speeches, such as “Two Souls Intertwined,” The Tanner Lecture he delivered at the University of Utah in 2012. Geography is destiny for all of us when it comes to our health and well-being, once again proven by Gallup-Healthways in The State of American Well-Being 2016 Community Well-Being Rankings. The darkest blue circles in the U.S. map indicate the metro areas in the highest-quintile of well-being. The index of well-being is based on five metrics, of consumer self-ranking
Will Republican Healthcare Policy “Make America Sick Again?” Two New Polls Show Growing Support for ACA

Results of two polls published in the past week, from the Kaiser Family Foundation and Pew Research Center, demonstrate growing support for the Affordable Care Act, aka Obamacare. The Kaiser Health Tracking Poll: Future Directions for the ACA and Medicaid was published 24 February 2017. The first line chart illustrates the results, with the blue line for consumers’ “favorable view” on the ACA crossing several points above the “unfavorable” orange line for the first time since the law was signed in 2010. The margins in February 2017 were 48% favorable, 42% unfavorable. While the majority of Republicans continue to be solidly
20% of the US Economy Will Be Healthcare Spending in 2025

Price increases and growing use of healthcare services will drive national health spending (NHE) in the U.S. to 20% of the nation’s economy by 2025, according to projections calculated by a team from the Centers for Medicare and Medicaid Services (CMS). Health spending will reach $3.6 trillion dollars this year. These were published in a Web-First article in Health Affairs on 15 February 2017 The caveat on these numbers is that the CMS team used economic models based on “current-law framework:” these make no assumptions about legislative changes that may occur in healthcare reform between 2017 and 2025. While that’s a
Americans Far More Likely to Self-Ration Prescription Drugs Due To Cost

Americans are more than five times more likely to skip medication doses or not fill prescriptions due to cost than peers in the United Kingdom or Switzerland. U.S. patients are twice as likely as Canadians to avoid medicines due to cost. And, compared with health citizens in France, U.S. consumers are ten-times more likely to be non-adherent to prescription medications due to cost. It’s very clear that more consumers tend to avoid filling and taking prescription drugs, due to cost barriers, when faced with higher direct charges for medicines. This evidence is presented in the research article, Cost-related non-adherence to prescribed
Medical Debt Is A Risk Factor For Consumers’ Financial Wellness
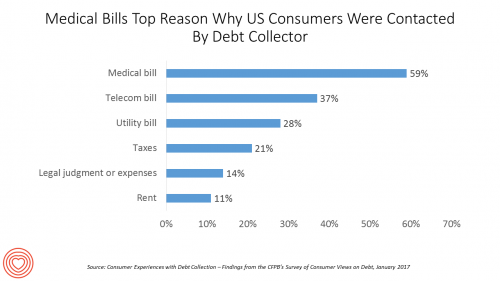
The top reason US consumers hear from a debt collector is due to medical bills, for 6 in 10 people in Americans contacted regarding a collection. This month, the Consumer Financial Protection Bureau (CFPB) published its report on Consumer Experiences with Debt Collection. Medical bill collections are the most common debt for which consumers are contacted by collectors, followed by phone bills, utility bills, and tax bills. The prevalence of past-due medical debt is unique compared with these other types because healthcare cost problems impact consumers at low, middle, and high incomes alike. Specifically: 62% of consumers earning $20,000 to
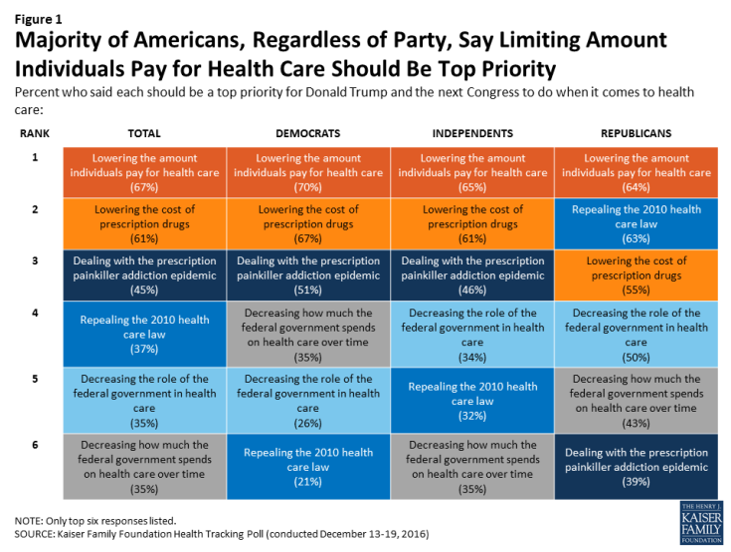
Health Care Costs, Not the ACA, Rank #1 in Americans’ Minds As President Trump Assumes the Presidency
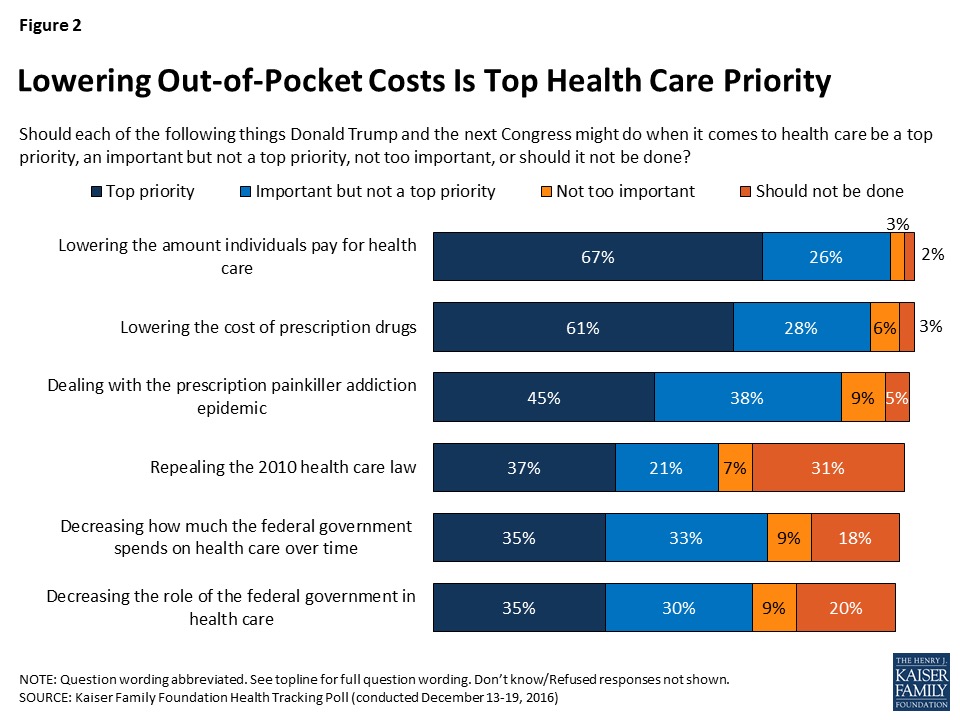
More Americans are worried about their out-of-pocket health care costs than they are about repealing the Affordable Care Act (ACA), according to the Kaiser Family Foundation (KFF) Health Tracking Poll published 6th January 2017, the first KFF poll for the new year. Cost worries fall into two buckets of concerns: the cost of health care, and the cost of prescription drugs. Managing the opioid epidemic falls in third place after health care costs. Repealing the Affordable Care Act? It’s #4 on Americans’ health care priorities as of mid-December 2016, followed by shrinking the Federal’s government’s role in and spending on
Nursing Is Seen As The Most Ethical Profession in America; Congress Members, Least
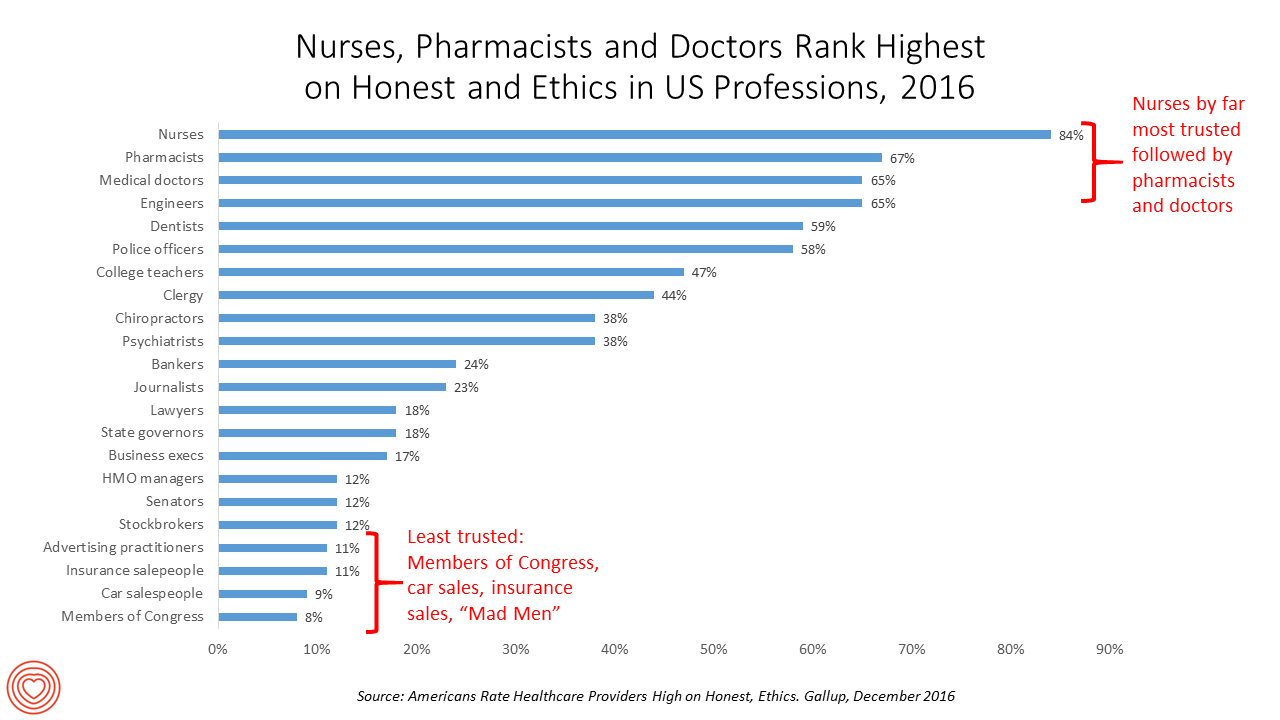
Nurses rank, by far, the top profession for honest and ethics in the U.S. in the 2016 version of the annual Gallup poll on ethics in professions, Americans Rate Healthcare Providers High on Honest, Ethics, published this week. Since 1999, nurses have been #1 in this survey except for the year 2001, when firefighters scored the top spot in light of the 9/11 attack. Another consistency in this survey among U.S. consumers is that pharmacists and physicians top the list once again, after nurses, and the most-trusted professions in America. At the bottom of the roster, as in 2015, are Members
The Shift to Healthcare Value in a Post-Trump America, via PwC
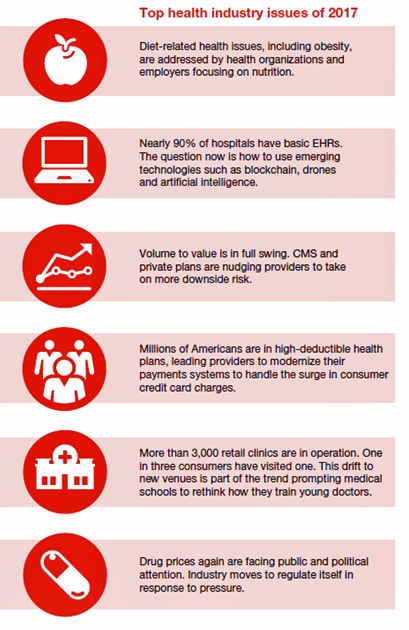
In President Donald Trump’s preliminary thoughts about health care in America, the landscape would feature a mix of tax credits, health savings accounts, high-risk pool, state Medicaid block grants, and regulatory control shifting from the Federal government to the states, according to PwC’s forecast for the new year, Top health industry issues of 2017. PwC frames the 2017 top healthcare issues under the overall strategic imperative of value, with three categories: Adapting for value Innovating for value Building for value. The ten top issues that will shape U.S. healthcare for the next year, PwC expects, will be: An uncertain fate for the
One-Half of Privately-Insured Americans Are Dissatisfied With Healthcare Costs
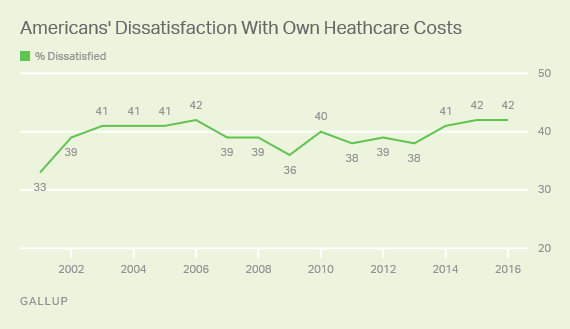
A plurality of Americans, 4 in 10, are dissatisfied with the healthcare costs they face. The level of dissatisfaction varies by a consumer’s type of health insurance, while overall, 42% of people are dissatisfied with costs… 48% of privately insured people are dissatisfied with thei healthcare costs 29% of people on Medicare or Medicaid are dissatisfied 62% of uninsured people are dissatisfied. Gallup has polled Americans on this question since 2014 every November. Dissatisfaction with healthcare costs is up from 38% from the period 2011-2013. As the line chart illustrates, the current levels of cost-dissatisfaction are similar to those felt
U.S. Healthcare Spending Hit Nearly $10,000 A Person In 2015
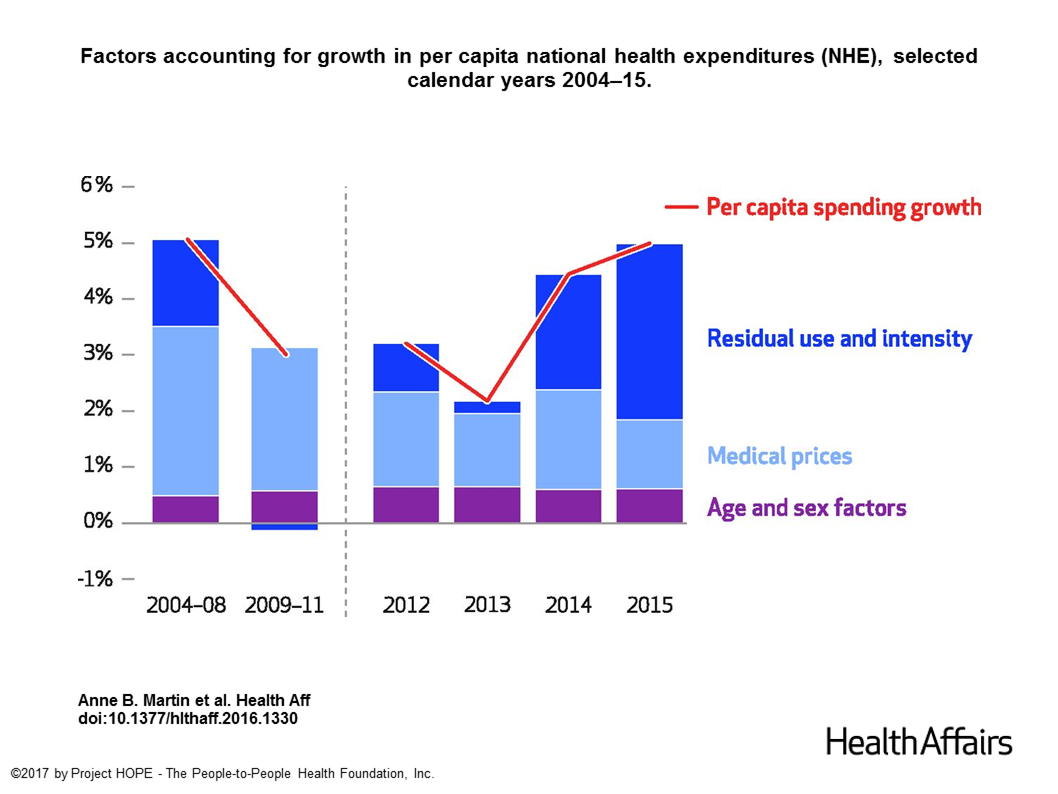
Spending on health care in the U.S. hit $3.2 trillion in 2015, increasing 5.8% from 2014. This works out to $9,990 per person in the U.S., and nearly 18% of the nation’s gross domestic product (GDP). Factors that drove such significant spending growth included increases in private health insurance coverage owing to the Affordable Care Act (ACA) coverage (7.2%), and spending on physician services (7.2%) and hospital care (5.6%). Prescription drug spending grew by 9% between 2014 and 2015 (a topic which I’ll cover in tomorrow’s Health Populi discussing IMS Institute’s latest report into global medicines spending). The topic of
1 in 3 Americans Still Self-Rations Healthcare
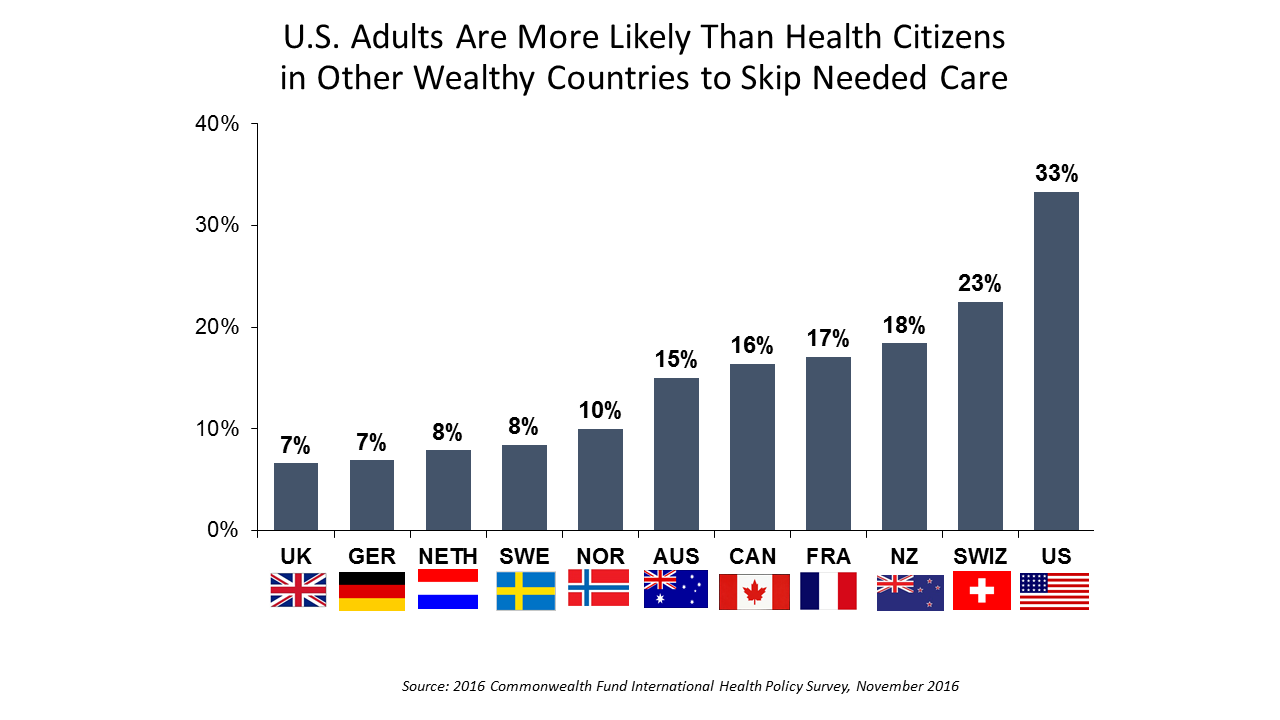
People in the U.S. are much more likely to go without health care they need compared with health citizens in 10 other wealthy countries, according to the Commonwealth Fund’s 2016 international survey. One-third of Americans did not seek care due to costs, including going without recommended care, failing to fill a prescription drug, and/or not seeing a doctor when sick. While this self-rationing proportion of Americans dropped from 37% in 2013, the U.S. still ranks #1 in foregoing necessary healthcare due to cost. “In comparison to adults in the other 10 countries, adult sin the U.S. are sicker and more
Healthcare Reform in President Trump’s America – A Preliminary Look

It’s the 9th of November, 2016, and Donald Trump has been elected the 45th President of the United States of America. On this morning after #2016Election, Health Populi looks at what we know we know about President Elect-Trump’s health policy priorities. Repeal-and-replace has been Mantra #1 for Mr. Trump’s health policy. With all three branches of the U.S. government under Republican control in 2018, this policy prescription may have a strong shot. The complication is that the Affordable Care Act (aka ObamaCare in Mr. Trump’s tweet) includes several provisions that the newly-insured and American health citizens really value, including: Extending health
Growing Sentiment for a Single Payer Healthcare System in the U.S.
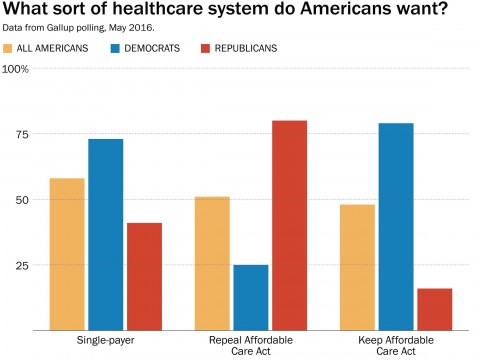
There is growing support for a single payer healthcare system in America, found in the latest Gallup Poll and a survey the organization conducted earlier this year in May 2016. A slight majority of Americans favor a single payer system, shown in the first chart. By political party, that splits into 3 in 4 Democrats pro-single payer, and 4 in 10 Republicans (41%). Note that the 41% of Republicans who favor single payer is a much higher number than the 16% who favor keeping the Affordable Care Act in place. Gallup writes, “The general idea of a single payer system seems to
In #Election2016, Americans Care More About the Cost of Prescription Drugs Than the ACA
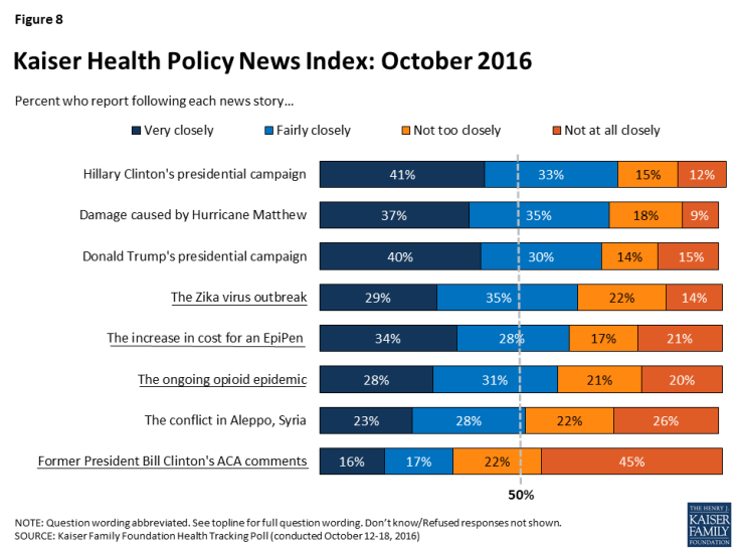
“When thinking about health care priorities for the next president and Congress to address, dealing with the high price of prescription drugs tops the public’s list while issues specific to the Affordable Care Act (ACA), such as repealing provisions of the law or repealing the law entirely, are viewed as top priorities by fewer Americans,” according to the Kaiser Health Tracking Poll for October 2016 – the last such survey to be taken before the 2016 Presidential election. The poster child snapshot image representing the high cost of prescription drugs is the increase in cost for an EpiPen, which among
Americans Have Begun to Raid Retirement Savings for Current Healthcare Costs
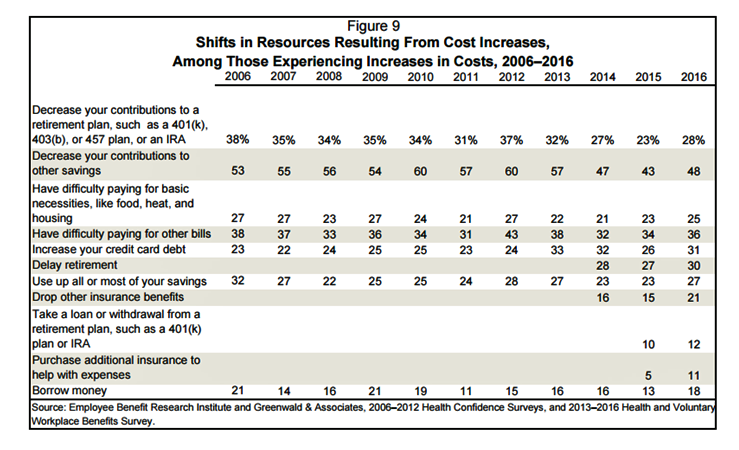
While American workers appreciate the benefits they receive at work, people are concerned about health care costs. And consumers’ collective response to rising health care costs is changing the way they use health care services and products, like prescription drugs. Furthermore, 6 in 10 U.S. health citizens rank healthcare as poor (27%) or fair (33%). This sober profile on healthcare consumers emerges out of survey research conducted by EBRI (the Employee Benefit Research Institute), analyzed in the report Workers Like Their Benefits, Are Confident of Future Availability, But Dissatisfied With the Health Care System and Pessimistic About Future Access and
Stress and Health During #Election2016
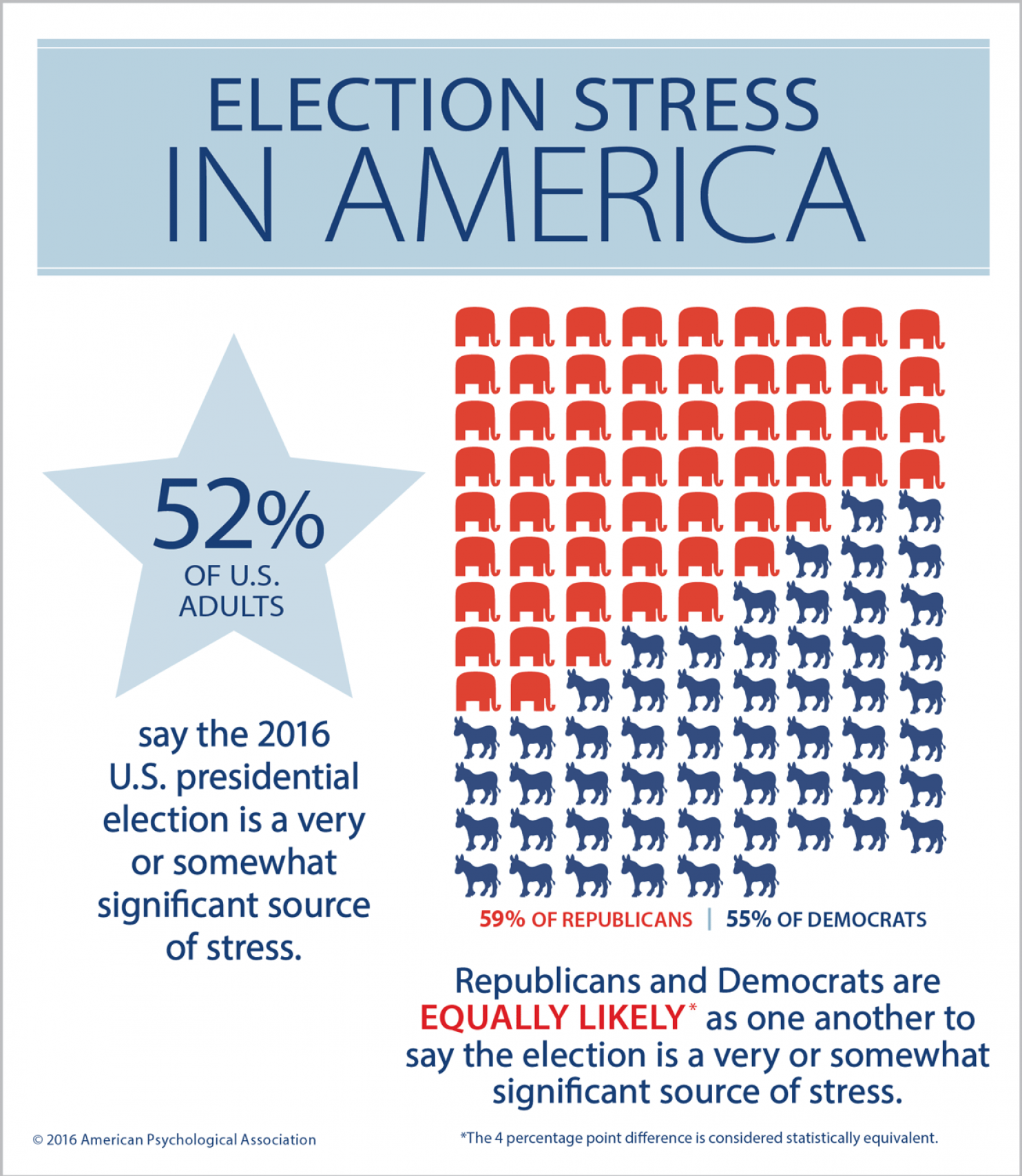
The American Psychological Association, which conducts the annual Stress in America survey, has found rising levels of stress during #Election2016. 1 in 2 U.S. adults says the U.S. presidential election is a source of stress, with Democrats and Republicans equally likely to feel this way. So the APA is offering tips on how we can deal with the health impacts of election season stress. These include: Take a digital break and limiting your media consumption, reading or listening to “just enough to stay informed.” Instead, go for a walk and do things you enjoy. Avoid getting into and limit discussions about the
Costs of Care and the ACA Top Voters’ Healthcare Issues
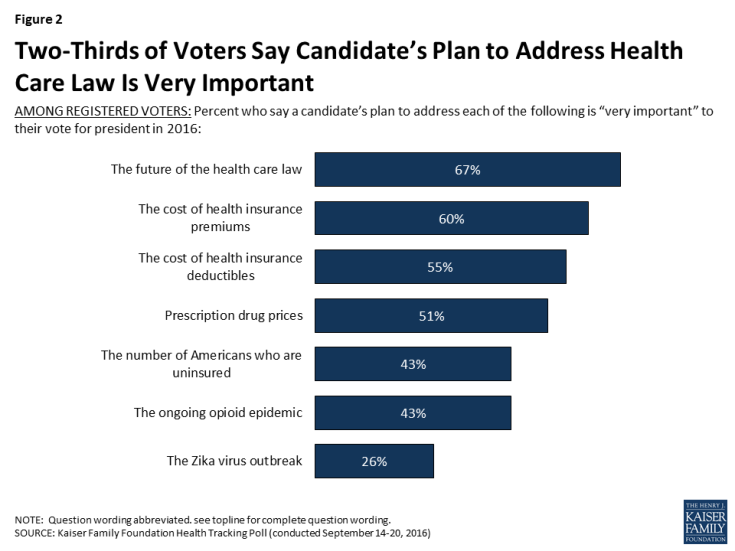
Two in three US voters put the future of the Affordable Care Act as the #1 healthcare issue in the 2016 President election. The ACA is closely followed by healthcare costs — for insurance premiums, deductibles, and prescription drugs, according to the September 2016 Kaiser Health Tracking Poll. The opioid addiction and mortality epidemic is a top healthcare issue for 43% of US voters, and the Zika virus, among 26% of voters. Note that more supporters of Hillary Clinton are healthcare-oriented voters than people who favor Donald Trump. Uninsurance and costs, in addition to the future of the ACA, rank
More Americans See Hillary Clinton As the 2016 Presidential Health Care Candidate
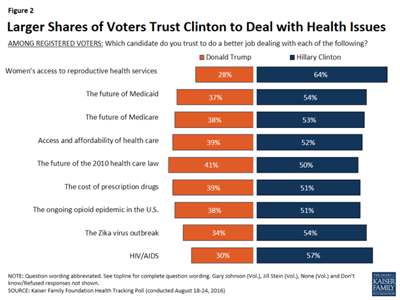
When it comes to health care, more American voters trust Hillary Clinton to deal with health issues than Donald Trump, according to the Kaiser Health Tracking Poll: August 2016 from the Kaiser Family Foundation (KFF). The poll covered the Presidential election, the Zika virus, and consumers’ views on the value of and access to personal health information via electronic health records. Today’s Health Populi post will cover the political dimensions of the August 2016 KFF poll; in tomorrow’s post, I will address the health information issues. First, let’s address the political lens of the poll. More voters trust Hillary Clinton to do
Aging America Is Driving Growth in Federal Healthcare Spending
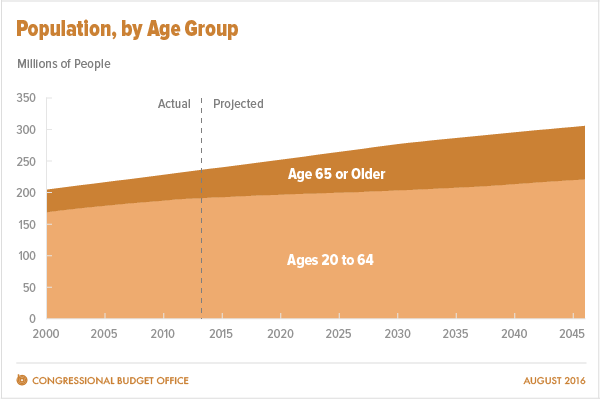
Federal healthcare program costs are the largest component of mandatory spending in the U.S. budget, according to An Update to the Budget and Economic Outlook: 2016 to 2026 from the U.S. Congressional Budget Office (CBO). Federal spending for healthcare will increase $77 billion in 2016, about 8% over 2015, for a total of $1.1 trillion. The CBO believes that number overstates the growth in Medicare and Medicaid because of a one-time payment shift of $22 bn to Medicare (from 2017 back into 2016); adjusting for this, CBO sees Federal healthcare spending growing 6% (about $55 bn) this year. The driver
Health in America: Improving, But Disparities Need Policy Prescriptions
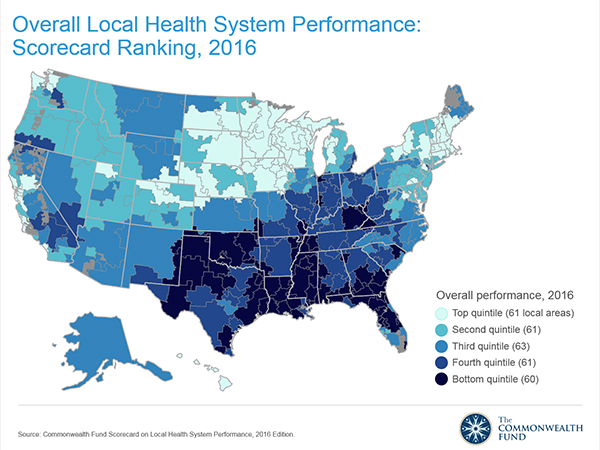
The bad news: mortality rates haven’t improved much and obesity rates rose in one-third of communities. The good news: public health gains can be made in resource-poor communities with the right health policies, based on research from The Commonwealth Fund, Rising to the Challenge, the Fund’s Scorecard on local health system performance for 2016. The top-line of this benchmark report is that health care in the U.S. has, overall, improved more than it’s declined. Among the big levers driving health care improvement in the past year have been the further expansion of health citizens covered with insurance through the Affordable
U.S. Health Spending Will Comprise 20% of GDP in 2025
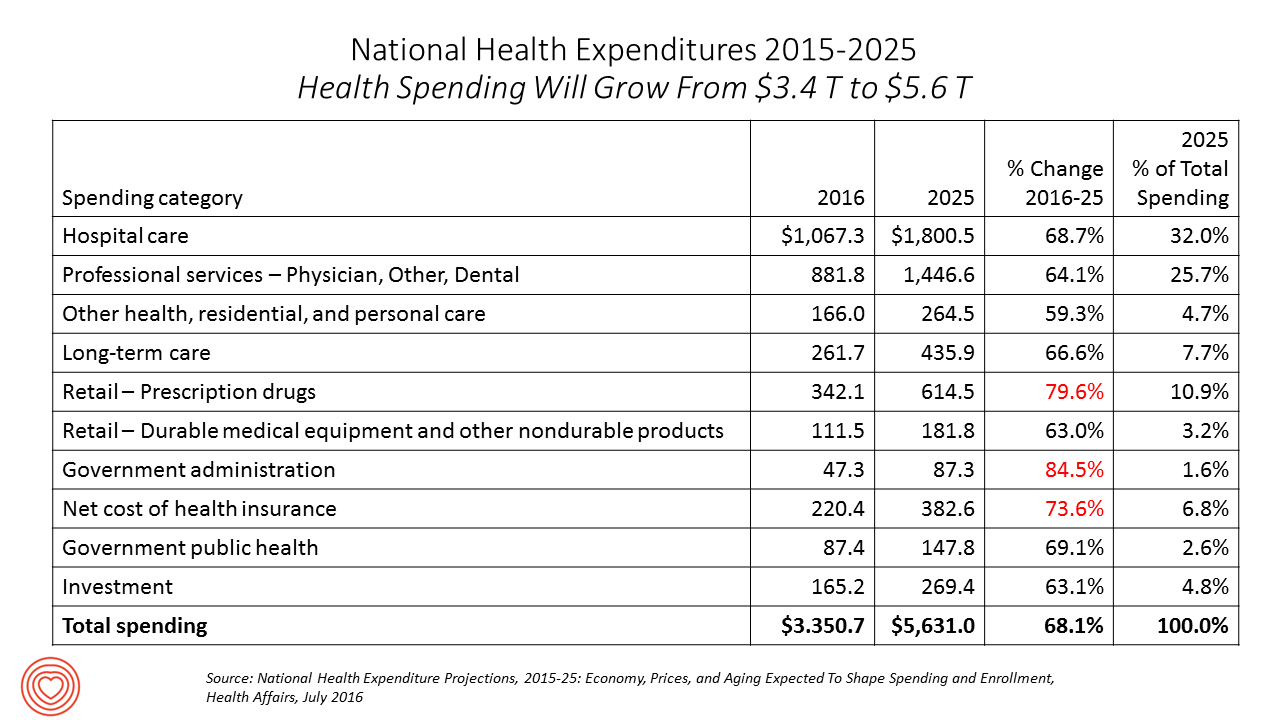
Spending on health care in America will comprise $1 in every $5 of gross domestic product in 2025, according to National Health Expenditure Projections, 2015-25: Economy, Prices, And Aging Expected to Shape Spending and Enrollment, featured in the Health Affairs July 2016 issue. Details on national health spending are shown by line item in the table, excerpted from the article. Health spending will grow by 5.8% per year, on average, between 2015 and 2025, based on the calculations by the actuarial team from the Centers for Medicare and Medicaid Services (CMS), authors of the study. The team noted that the Affordable Care
Health Care Reform: President Obama Pens Progress in JAMA
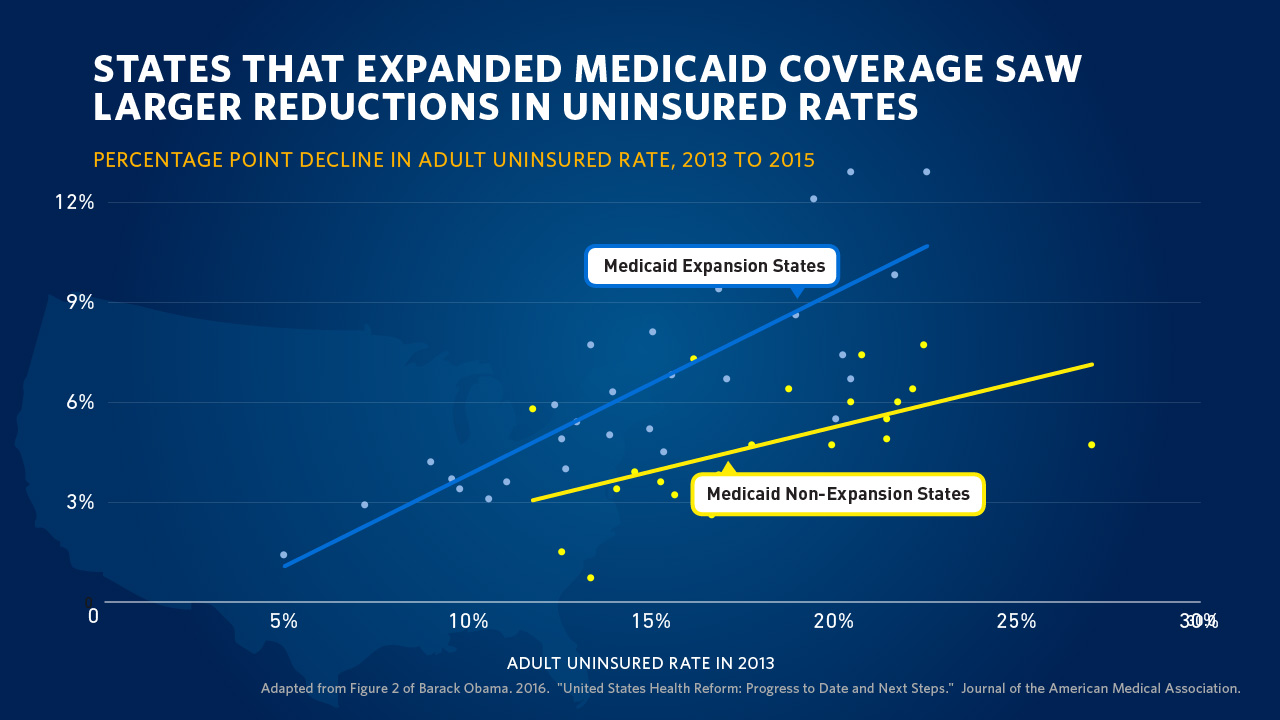
“Take Governor John Kasich’s explanation for expanding Medicaid: ‘For those that live in the shadows of life, those who are the least among us, I will not accept the fact that the most vulnerable in our state should be ignored. We can help them.’” So quotes President Barack Obama in the Journal of the American Medical Association, JAMA, in today’s online issue. #POTUS penned, United States Health Care Reform: Progress to Date and Next Steps. The author is named as “Barack Obama, JD,” a nod to the President’s legal credentials. Governor Kasich, a Republican, was one of 31 Governors who
Most Americans Favor A Federally-Funded Health System
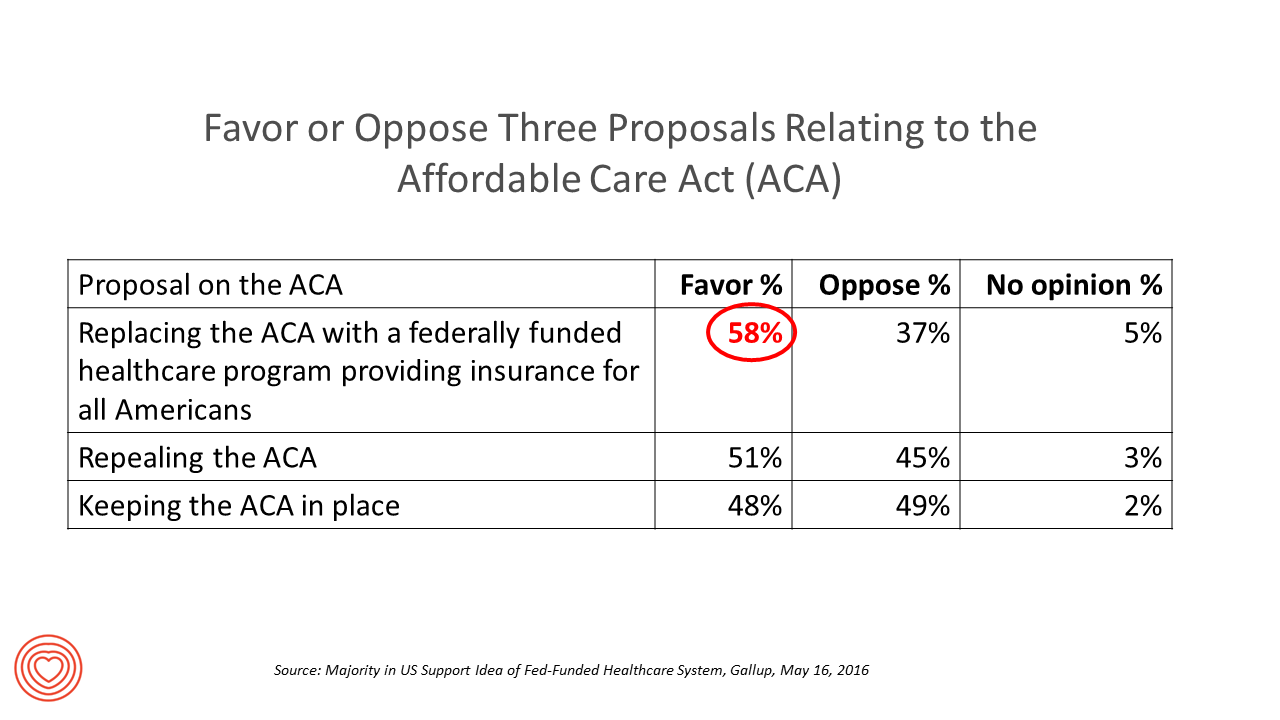
6 in 10 people in the US would like to replace the Affordable Care Act with a national health insurance program for all Americans, according to a Gallup Poll conducted on the phone in May 2016 among 1,549 U.S. adults. By political party, RE: Launch a Federal/national health insurance plan (“healthcare a la Bernie Sanders”): Among Democrats, 73% favor the Federal/national health insurance plan, and only 22% oppose it; 41% of Republicans favor it and 55% oppose it. RE: Repeal the ACA (“healthcare a la Donald Trump”): Among Democrats, 25% say scrap the ACA, and 80% of Republicans say to do
Control Drug Costs and Regulate Pharma, Most Older Americans Say
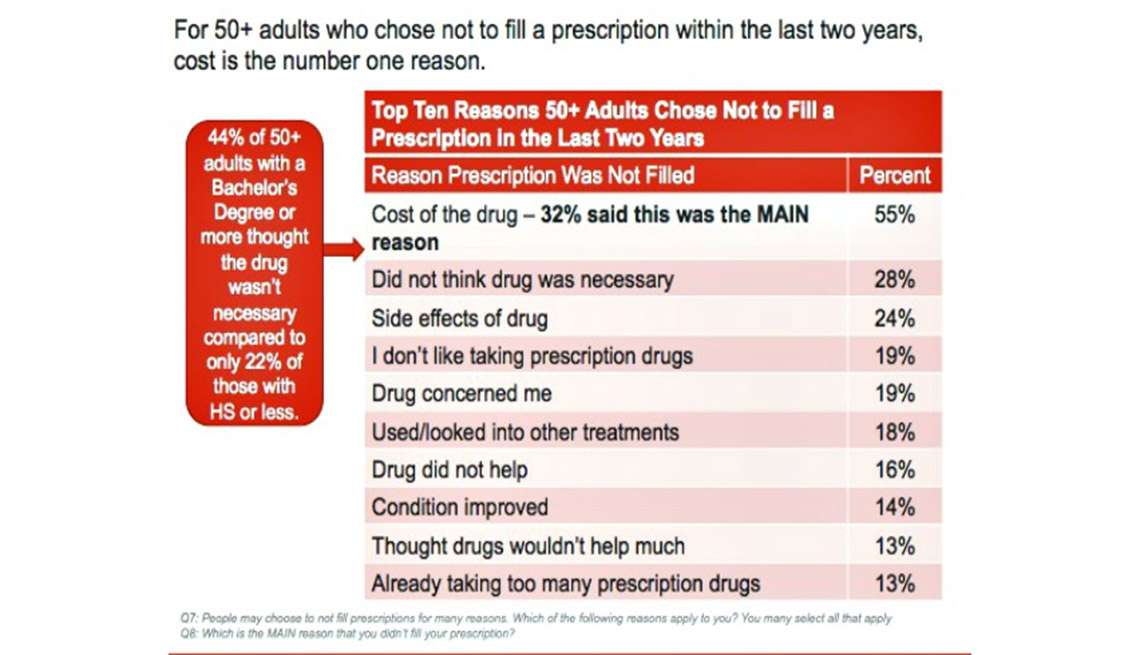
The top reason people in America over 50 don’t fill a prescription is the cost of the drug, according to the AARP 2015 Survey on Prescription Drugs. Eight in 10 people 50+ think the cost of prescription drugs is too high, and 4 in 10 are concerned about their ability to afford their medications. Thus, nearly all people over 50 think it’s important for politicians (especially presidential candidates) to control Rx drug costs. Older consumers are connecting dots between the cost of their medications and direct-to-consumer prescription drug advertising: 88% of the 50+ population who have seen or heard drug
Let’s Make a Deal: Patients Weigh Privacy Paybacks
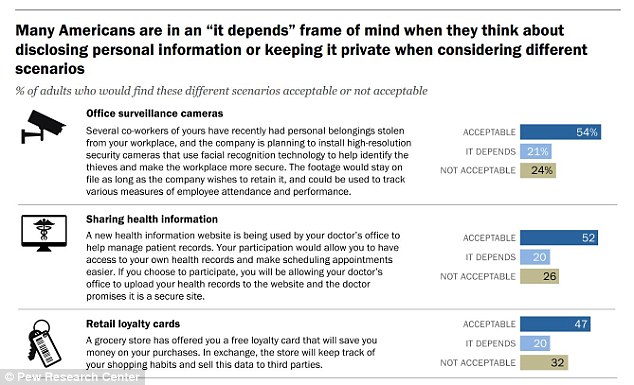
“It depends” is the hedge-phrase that characterizes how Americans see disclosing personal information versus keeping private information private, according to the consumer survey report, Privacy and Information Sharing, published by the Pew Research Center (PRC) in January 2016. U.S. adults see a privacy trade-off, living in the convenience-context of 21st century digital economy in exchange for some form of value. The “it depends” is a factor of what kind of data is geing collected, especially by third parties, how long that data area retained, for what use — vis-à-vis what a person is trading in return which could be a hard dollar
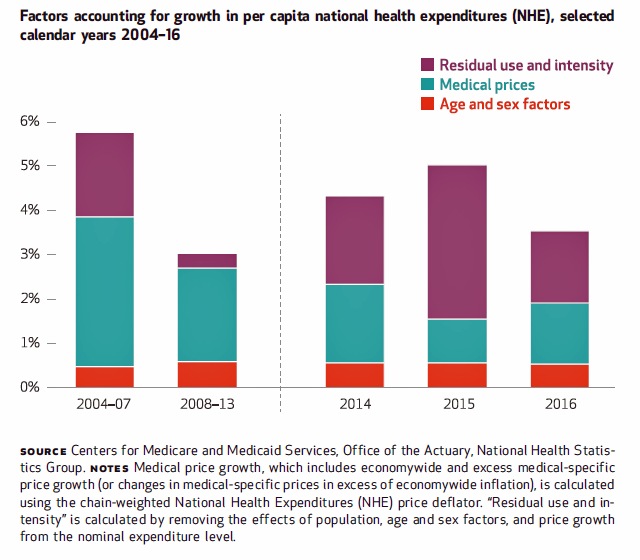
U.S. National Health Spending Up Due to More People Covered and Higher Drug Costs
National health spending in American grew by 5.3% in 2014, hitting the $3 trillion mark. This represented an up-tick nearly twice the growth rate of 2.9% in 2013, the slowest rate of growth in 55 years, according to the latest analysis of the U.S. health economy published by Health Affairs. The first chart illustrates the factors that contribute to that 5.3% growth in health spending. The two largest factors were medical prices and so-called “residual use and intensity.” The medical price increase portion was 1.8% in 2014, up from 1.3% in 2013. The use and intensity component was attributable to
51% of Americans Say It’s Government’s Responsibility To Provide Health Insurance
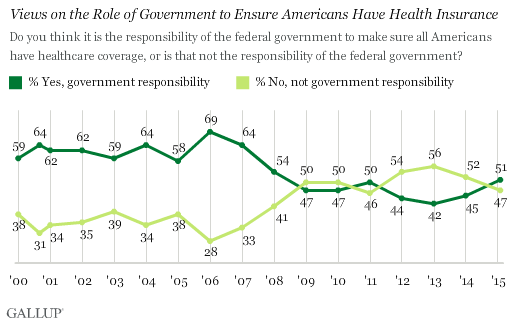
For the first time since 2008, a majority of Americans say government is responsible for ensuring that people have health insurance. The first chart shows the crossing lines between those who see government-assured health insurance in the rising dark green line in 2015, and people who see it as a private sector responsibility. The demographics and sentiments underneath the 51% are important to parse out: people who approve of the Affordable Care Act are over 3x more likely to believe in government sponsoring health insurance versus those who disapprove, 80% compared with 26%. The demographic differences are also striking, detailed
Social Determinants Impact Health More Than Health Care
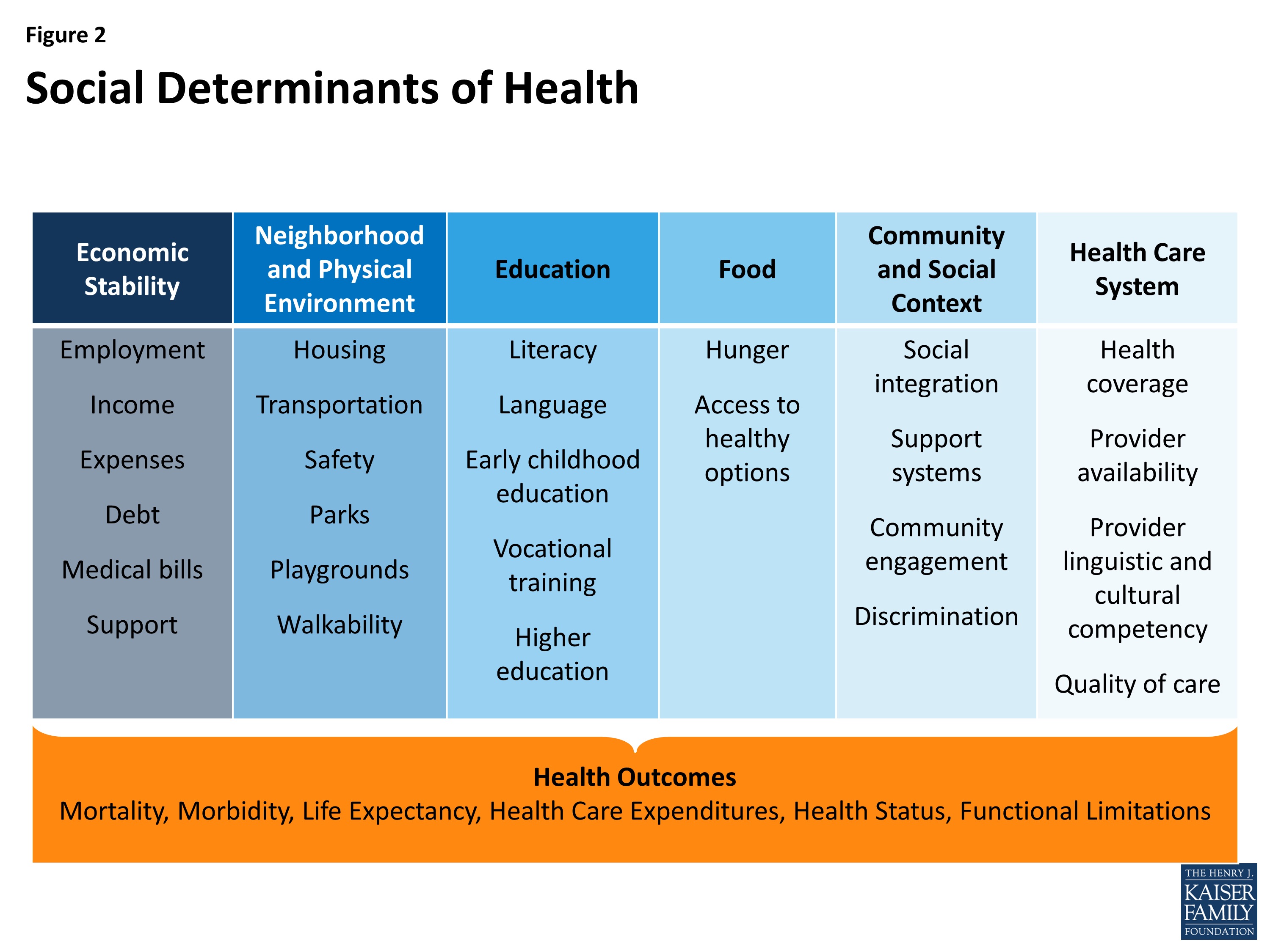
The factors of where people are born, live, work and age — social determinants — shape human health more than health care. Yet in the U.S. much more resource per capita is funneled into healthcare services than into social ones. Beyond Health Care: The Role of Social Determinants in Promoting Health and Health Equity was published by The Kaiser Commission on Medicaid and the Uninsured in November 2015, calling attention to the opportunity and wisdom of baking health into all public policy. The social determinants of health (SDOH) include economic stability, the physical environment and neighborhood, education, food, community and
Health Care Costs Are #1 Pocketbook Issue, and Drug Prices Top the Line Items
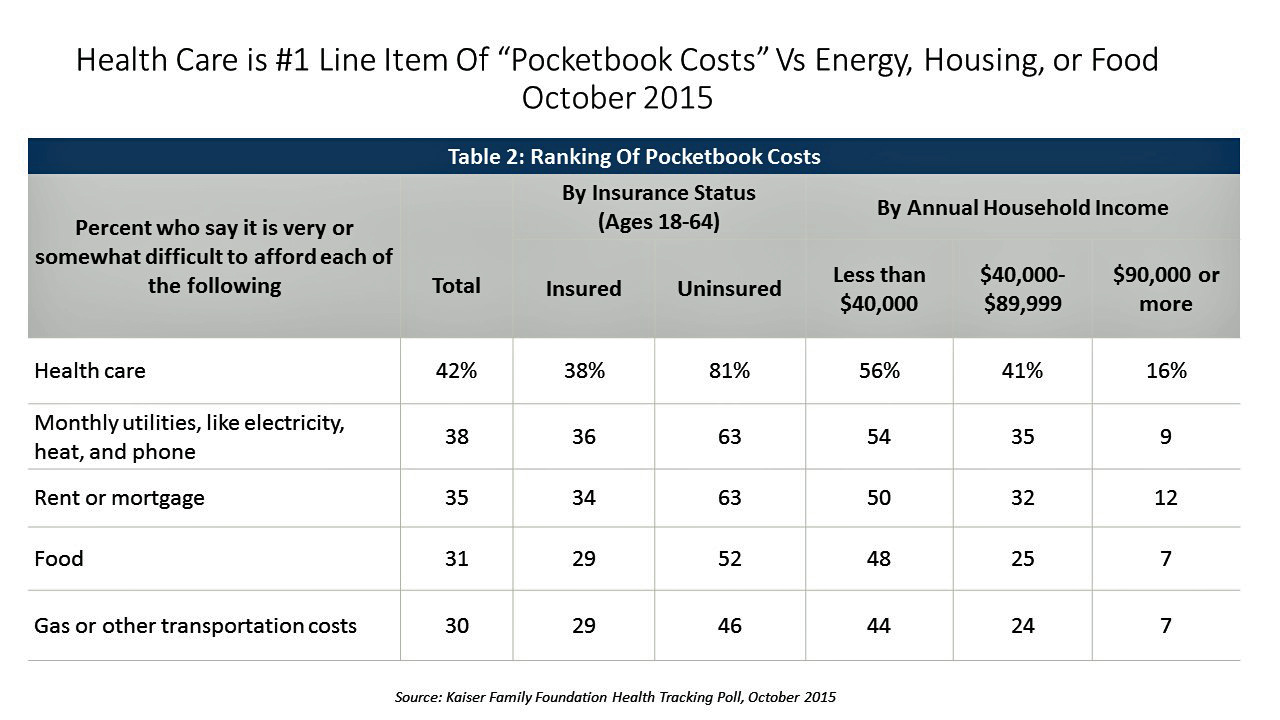
Consumers are most concerned about health care costs among their kitchen table issues, above their ability to afford the utility bill, housing, food, or gas and transportation costs. The October 2015 Kaiser Family Foundation Health Tracking Poll finds 4 in 10 Americans finding it difficult to afford health care, including 16% of people earning $90,000 a year or more. Underneath that worrying healthcare cost umbrella are the price of prescription drugs, which the majority of Democrats, Independents, and Republicans all agree need to be “limited” by government regulation. Ensuring that the public have affordable access to high-cost drugs for chronic conditions
Palliative Care: Getting End of Life Care (W)right
I lost a best friend last week. His memorial service, held this past weekend, was a celebration of his life. And part of that well-lived life was a very conscious planning of his last days. The Economist published its 2015 Quality of Death Index, a data-driven treatise on palliative care, the very week my dear friend Rick died. This gives me the opportunity to discuss palliative care issues with Health Populi readers through The Economist’s lens, and then in the Hot Points below through my personal context of this remarkable man’s end-of-life choices. The Economist ranks 80 countries on several
IoT in Healthcare, Take 3 – Accenture & the Internet of Me in Health
We’re entering the era of personalized healthcare promising convenient and meaningful health experiences, according to Accenture’s 2015 Healthcare IT Vision articulated in their report, Top 5 eHealth Trends. This post is third in three published here on Health Populi this week, exploring the growing role of the Internet of Things in health/care. On 8th July, we dug into McKinsey Global Institute’s research on IoT’s influence over nine industries, including human health; and on the 9th, we reviewed Goldman Sachs’ report on digital health’s potential impact on the U.S. healthcare system. Accenture’s five eHealth trends include: The Internet of Me; the Outcome Economy, with
What the SCOTUS ACA ruling means for health consumers
Now that the Affordable Care Act is settled, in the eyes of the U.S. Supreme Court, what does the 6-3 ruling mean for health/care consumers living in America? I wrote the response to that question on the site of Intuit’s American Tax & Financial Center here. The top-line is that people living in Michigan, where the Federal government is running the health insurance exchange for Michiganders, and people living in New York, where the state is running the exchange, are considered equal under the ACA’s health insurance premium subsidies: health plan shoppers, whether resident New Yorkers or Michiganders, can qualify for
The 3 tectonic forces shaping patients – it’s BIO week
Patients in the U.S. are transforming into health care consumers, and in 2015 there are 3 underlying forces shaping that new consumer. This week kicks off the annual BIO conference in Philadelphia, and today Klick Health, the digital communications firm, convenes a group of thought leaders in healthcare to brainstorm markets, financing, and the state of pharmaceutical and life science innovation. An underlying theme throughout this meet-up is patient’s role in health/care. Patients are people, consumers, caregivers, mothers, fathers, sisters, brothers, friends, neighbors, community members, taxpayers, all. We’re old, we’re young, we’re mobile and not-so-much, we’re amputees, we’re migraneurs, we’re cancer
Telehealth goes retail
In the past couple of weeks, a grocery store launched a telemedicine pilot, a pharmacy chain expanded telehealth to patients in 25 states, and several new virtual healthcare entrants received $millions in investments. On a parallel track, the AMA postponed dealing with medical ethics issues regarding telemedicine, the Texas Medical Association got stopped in its tracks in a case versus Teladoc, and the Centers for Medicare and Medicaid Services (CMS) issued a final rule for the Medicare Shared Savings Program that falls short of allowing Accountable Care Organizations (ACOs) to take full advantage of telehealth services. These events beg the
It’s still the prices, stupid – health care costs drive consumerism
“It’s the prices, stupid,” wrote Uwe Reinhardt, Gerald F. Anderson and colleagues in the May 2003 issue of Health Affairs. Exactly twelve years later, three reports out in the first week of June 2015 illustrate that salient observation that is central to the U.S. healthcare macroeconomy. Avalere reports that spending on prescription drugs increased over 13% in 2014, with half of the growth attributable to new product launches over the past two years. Spending on pharmaceuticals has grown to 13% of overall health spending, and the growth of that spending between 2013-14 was the fastest since 2001. In light of
How Growing Income Inequality Hurts Everyone, and Especially Our Health
Income inequality has increased in most developed countries, and especially in the U.S., according to the OECD’s report, In It Together: Why Less Inequality Benefits All, published in May 2015. The red arrow in the first chart shows where the U.S. ranks versus other developed nations in income inequality, which is defined as the wealth gap between rich and poor people. The U.S. has the greatest income inequality in the developed world. The second chart shows data for the U.S. on benefits provided to low-wage workers (the bottom 25% of wage earners) versus high-wage workers (the top 25% of earners).
Hillary and George at HIMSS15
George Bush was the keynote speaker yesterday at HIMSS in Chicago at McCormick Place. As expected and appropriate, the Secret Service detail was at-the-ready to ensure the President’s safety and security. In the morning, members of the press were told by HIMSS’s communications staff that we would be able to watch the speech, live streamed, in the press room, able to cover the event in detail: words have meaning, and many of us were keen to hear how this President, who ushered in the early era of electronic health records, viewed healthcare and information technology then, and now. A fascinating
Doctors who write right: Gawande, Topol and Wachter put people at the center of health/care
There’s a trifecta of books written by three brilliant doctors that, together, provide a roadmap for the 21st century continuum of health care: The Patient Will See You Now by Eric Topol, MD; The Digital Doctor from Robert Wachter, MD; and, Being Mortal, by Atul Gawande. Each book’s take provides a lens, through the eyes of a hands-on healthcare provider, on healthcare delivery today (the good, the warts and all) and solutions based on their unique points-of-view. This triple-review will move, purposefully, from the digitally, technology optimistic “Gutenberg moment” for democratizing medicine per Dr. Topol, to the end-game importance of
The Affordable Care Act As New-Business Creator
While there’s little evidence that the short-term impact of the Affordable Care Act has limited job growth or driven most employers to drop health insurance plans, the ACA has spawned a “cottage industry” of health companies since 2010, according to PwC. As the ACA turned five years of age, the PwC Health Research Institute led by Ceci Connolly identified at least 90 newcos addressing opportunities inspired by the ACA: Supporting telehealth platforms between patients and providers, such as Vivre Health Educating consumers, such as the transparency provider HealthSparq does Streamlining operations to enhance efficiency, the business of Cureate among others
Health care costs, access and Ebola – what’s on health care consumers’ minds
The top 3 urgent health problems facing the U.S. are closely tied for first place: affordable health care/health costs, access to health care, and the Ebola virus. While the first two issues ranked #1 and #2 one year ago, Ebola didn’t even register on the list of healthcare stresses in November 2013. Gallup polled U.S. adults on the biggest health issues facing Americans in early November 2014, and 1 in 6 people named Ebola as the nation’s top health problem, ahead of obesity, cancer, as well as health costs and insurance coverage. Gallup points out that at the time of





 Thanks to Feedspot for identifying
Thanks to Feedspot for identifying  Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.