Healthcare 2030: Are We Consumers, CEOs, Health Citizens, or Castaways? 4 Scenarios On the Future of Health Care and Who We Are – Part 2
This post follows up Part 1 of a two-part series I’ve prepared in advance of the AHIP 2024 conference where I’ll be brainstorming these scenarios with a panel of folks who know their stuff in technology, health care and hospital systems, retail health, and pharmacy, among other key issues. Now, let’s dive into the four alternative futures built off of our two driving forces we discussed in Part 1. The stories: 4 future health care worlds for 2030 My goal for this post and for the AHIP panel is to brainstorm what the person’s
Healthcare 2030: Are We Consumers, CEOs, Health Citizens, or Castaways? 4 Scenarios On the Future of Health Care and Who We Are – Part 1
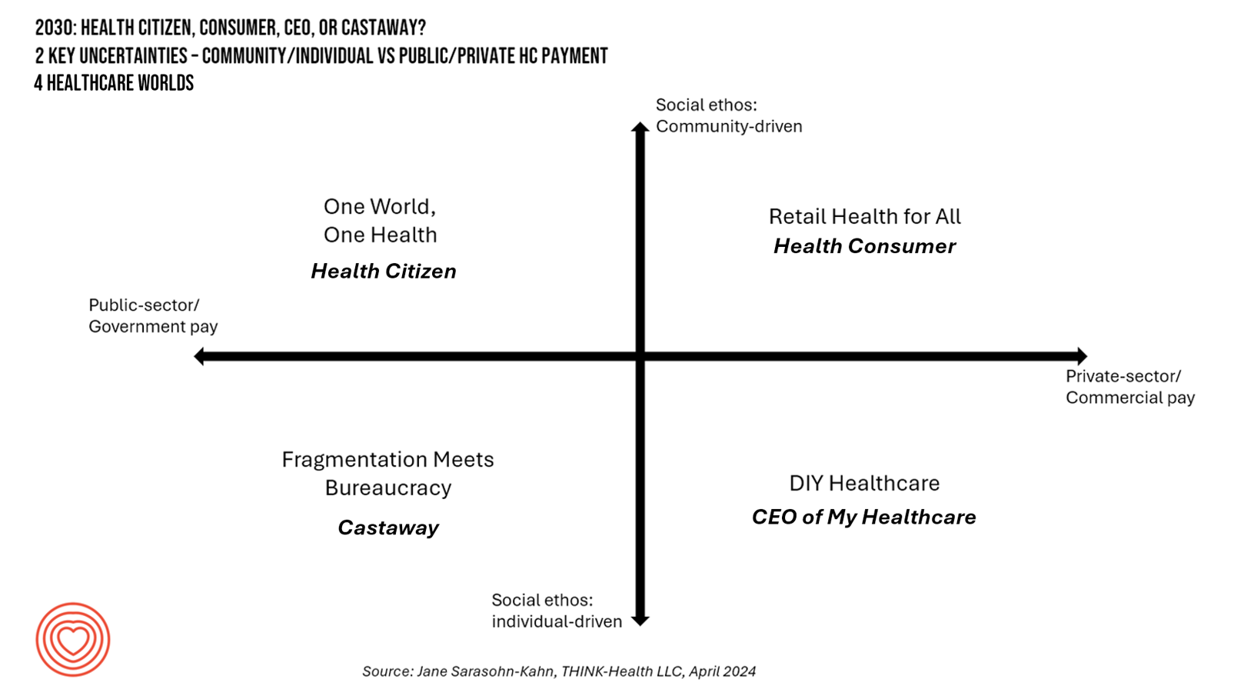
In the past few years, what event or innovation has had the metaphorical impact of hitting you upside the head and disrupted your best-laid plans in health care? A few such forces for me have been the COVID-19 pandemic, the emergence of Chat-GPT, and Russia’s invasion of Ukraine. That’s just three, and to be sure, there are several others that have compelled me to shift my mind-set about what I thought I knew-I-knew for my work with organizations spanning the health care ecosystem. I’m a long-time practitioner of scenario planning, thanks to the early education at the side of Ian
Considering Equity and Consumer Impacts of GLP-1 Drugs – A UBS Economist Weighs In
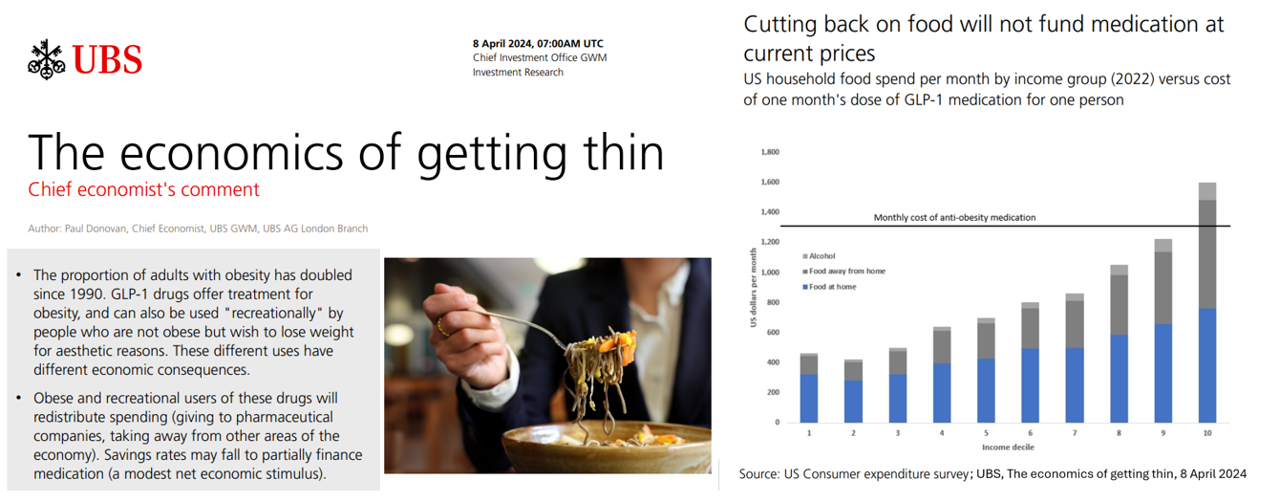
Since the introduction of GLP-1 drugs on the market, their use has split into two categories: for obesity and “recreationally,” according to the Chief Economist with UBS (formerly known as Union Bank of Switzerland). Paul Donovan, said economist, discusses The economics of getting thin in his regularly published comment blog. “These different uses have different economic consequences,” Donovan explains: Obese patients who use GLP-1s should become more productive employees, Donovan expects — less subject to prejudice, and less likely to be absent from work. While so-called recreational GLP-1 consumers may experience these
A Springtime Re-Set for Self-Care, From Fitness to Cozy Cardio: Peloton’s Latest Consumer Research
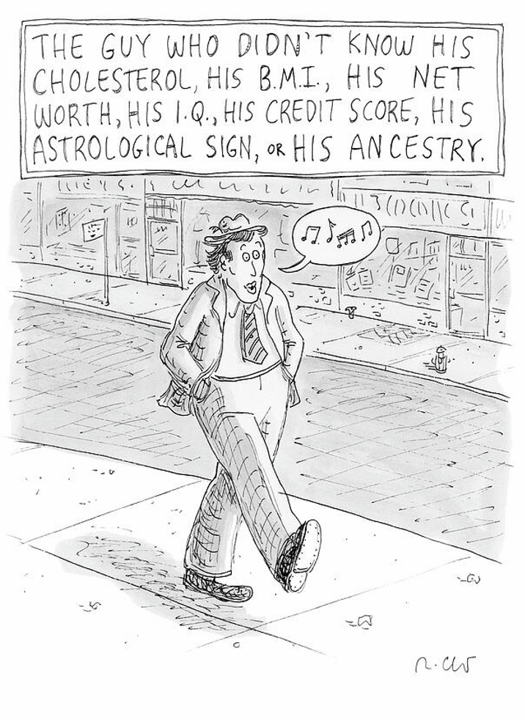
How many people do you know that don’t know their cholesterol or their BMI, their net worth or IQ, their credit score, astrological sign, or ancestry pie-chart? Chances are fewer and fewer as most people have gained access to medical records and lab test results on patient portals, calorie burns on smartwatches, credit scores via monthly credit card payments online, and completing spit tests from that popularly gifted Ancestry DNA test kits received during the holiday season. Meet “The Guy Who Didn’t Know His Cholesterol” conceived by Roz Chast,
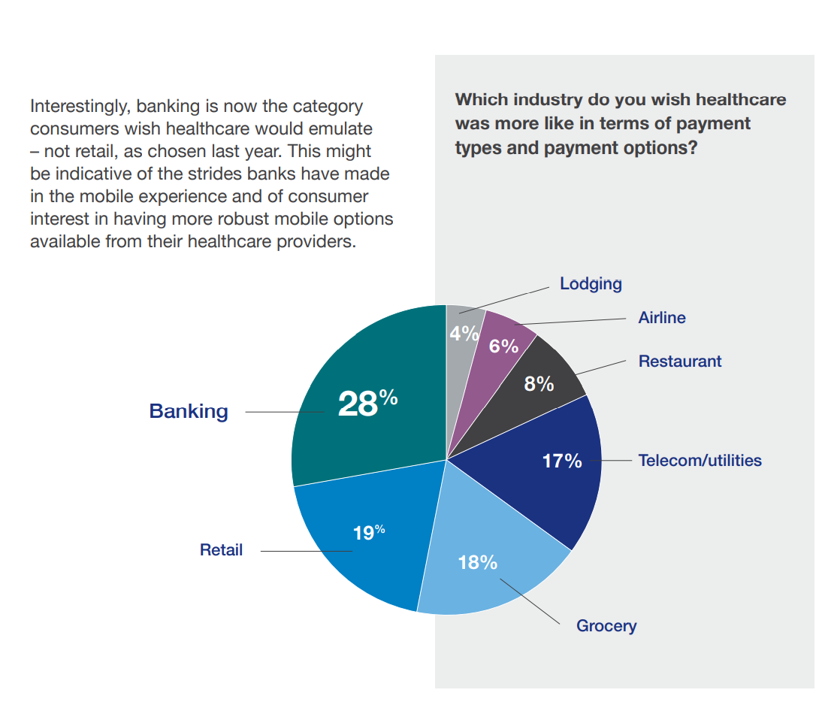
Consumers Are So Over Their Paper Chase in Health Care Payments

As we start the month of April 2024 in the U.S., it’s tax season in America with Federal (and other) income taxes due on the 15th of the month. This is also the time my research clock alarm goes off for an important annual report that describes the latest profile of the patient-as-payer in the U.S. ‘Tis the season for J.P. Morgan’s InstaMed team to analyze health care payments data, describing the experiences of consumers, providers and payers in the Trends in Healthcare Payments Fourteenth Annual Report. The overall takeaway for
Peering Into the Hidden Lives of Patients: a Manifesto from Paytient and Nonfiction
Having health insurance in America is no guarantee of actually receiving health care. It’s a case of having health insurance as “necessary but not sufficient,” as the cost of deductibles, out-of-pocket coinsurance sharing, and delaying care paint the picture of The Hidden Lives of Workplace-Insured Americans. That’s the title of a new report that captures the results of a survey conducted in January 2024 among 1,516 employed Americans who received employer-sponsored health insurance. The study was commissioned by Paytient, a health care financial services company, engaging the research firm Nonfiction to conduct the study
Celebrating World Sleep Day 2024 – Sleep Equity for Global Health

On the long list of things people can do to bolster their well-being, sleep ranks third after eating well and being physically active. We are calling out sleep as a key ingredient for health today, World Sleep Day 2024. Yes, it’s a real thing, and this year speaks to the theme of Sleep Equity for Global Health. The data point here comes from Datassential‘s latest consumer survey conducted across all adult age groups in the U.S. This information was shared with us yesterday during the company’s session covering Health and the Food & Beverage
The Economic Contours of the Change Healthcare Cyber Attack: Taking Stock So Far

On February 22, 2024, I went to a CVS Pharmacy-Inside-Target in my community to fill a prescription for benzonatate 200 mg capsules. I had caught a bad case of the flu the week before, and subsequently suffered a very long tail of a cough. That’s TMI for me to write about in the Health Populi blog, but this story has a current-events twist: the pharmacist could not electronically link with my insurance company to transact my payment. He tried a few work-flows, and ended up using a discount card which in the moment worked for us, and I paid the
A Health Consumer Bill of Rights: Assuring Affordability, Access, Autonomy, and Equity
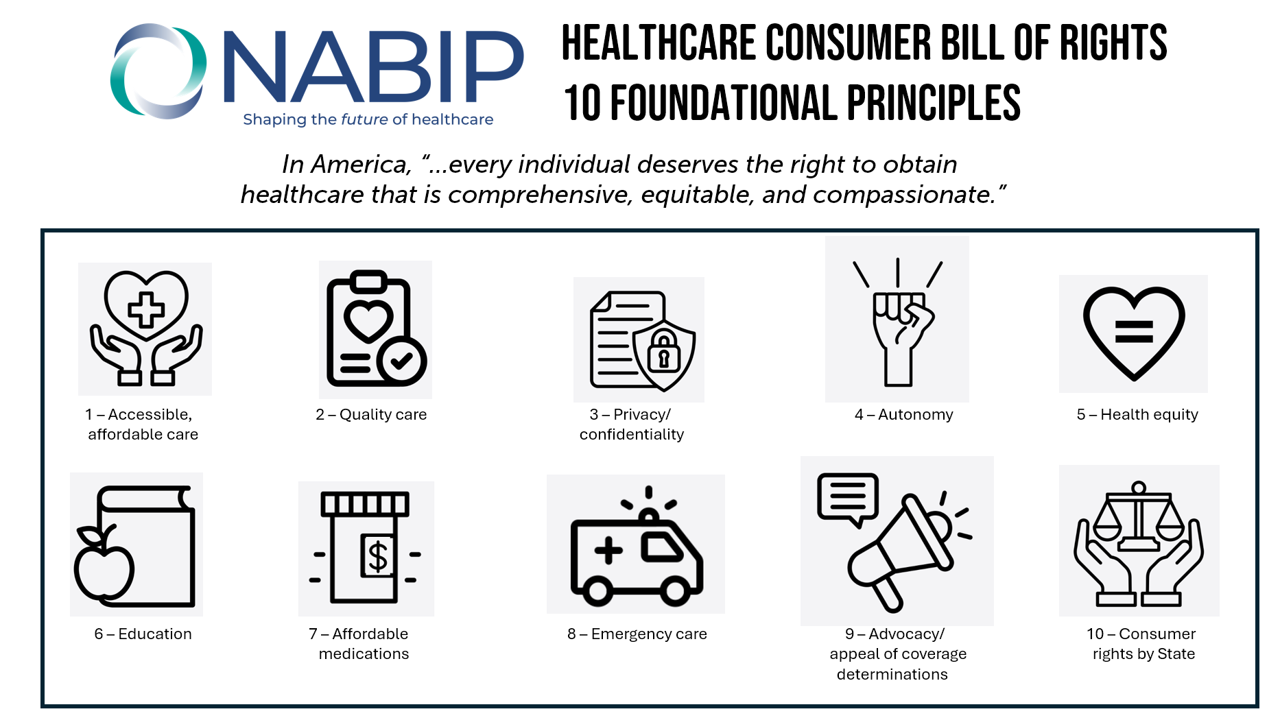
Let’s put “health” back into the U.S. health care system. That’s the mantra coming out of this week’s annual Capitol Conference convened by the National Association of Benefits and Insurance Professionals (NABIP). (FYI you might know of NABIP by its former acronym, NAHU, the National Association of Health Underwriters). NABIP, whose members represent professionals in the health insurance benefits industry, drafted and adopted a new American Healthcare Consumer Bill of Rights launched at the meeting. While the digital health stakeholder community is convening this week at VIVE in Los Angeles to share innovations in health tech, NABIP
Americans Come Together in Worries About Medical Bills, the Cost of Health Care, and Prescription Drug Costs
In the U.S., national news media, Federal statistics, dozens of business leaders and the Federal Reserve Bank have been talking about an historically positive American economy on a macro level. But among individual residents of the U.S., there is still a negative feeling about the economy in a personal context, revealed in the Kaiser Family Foundation Health Tracking Poll for February 2024. I’ve selected three figures of data from the KFF’s Poll which make the point that in peoples’ negative feelings about the national economy, their personal feelings about medical costs rank high
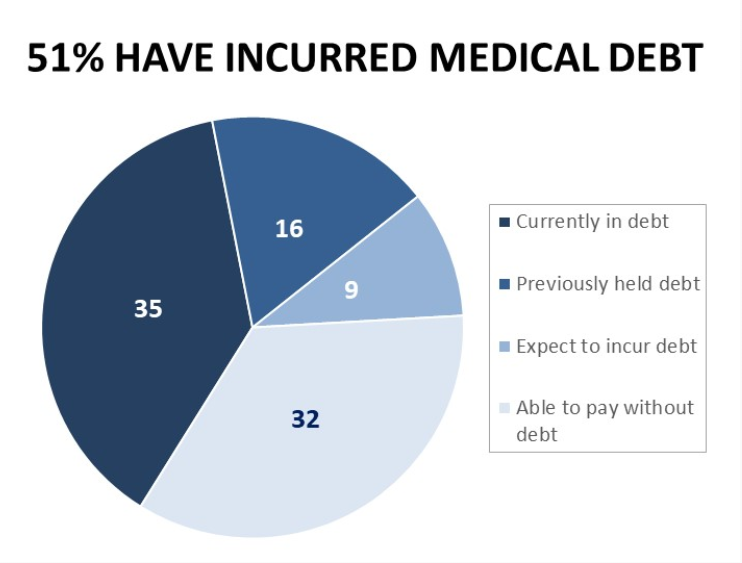
People With Medical Debt Are Much More Likely to Be in Financial Distress in America
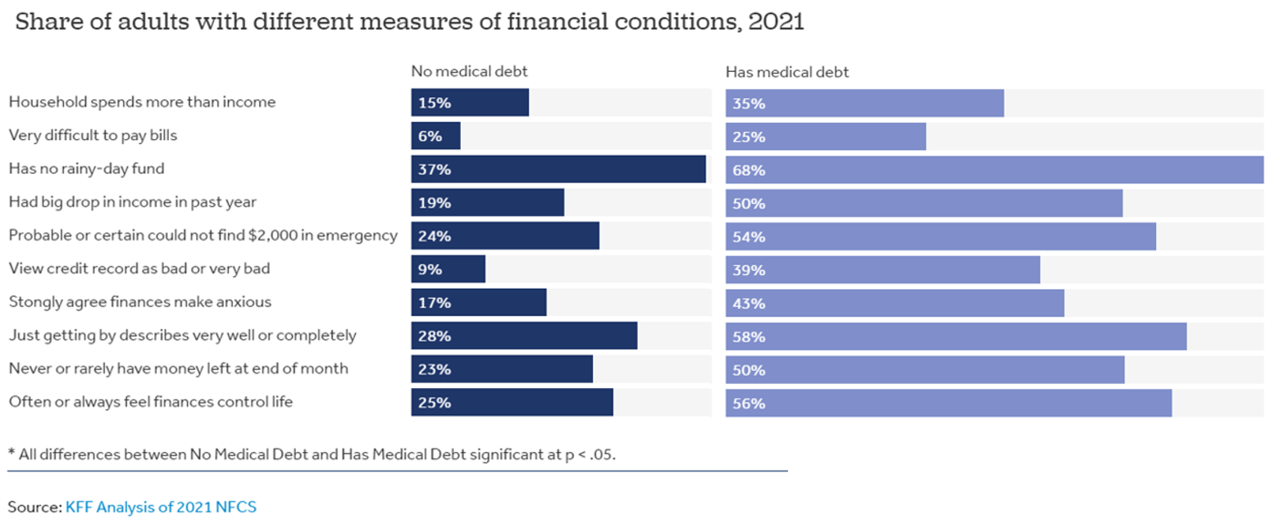
How financially vulnerable are people with medical debt in the U.S.? Significantly more, statistically speaking, we learn from the latest survey data revealed by the National Financial Capabilities Study (NFCS) from the FINRA Foundation. The Kaiser Family Foundation and Peterson Center on Healthcare analyzed the NFCS data through a consumer health care financial lens with a focus on medical debt. Financial distress takes many forms, the first chart inventories. People with medical debt were most likely lack saving for a “rainy day” fund, feel they’re “just getting by” financially, feel their finances control their life, and
The Wellness Market Shaped by Health at Home, Wearable Tech, and Clinical Evidence – Thinking McKinsey and Target
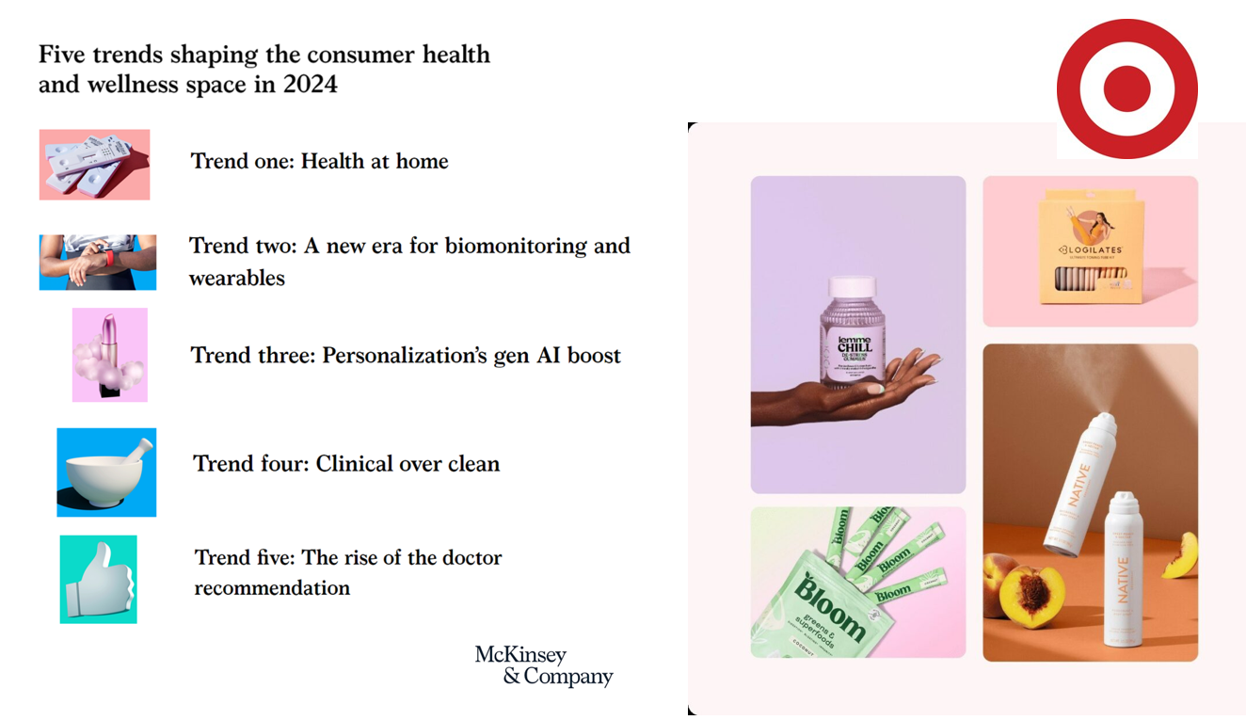
Target announced that the retail chain would grow its aisles of wellness-oriented products by at least 1,000 SKUs. The products will span the store’s large footprint, going beyond health and beauty reaching into fashion, food, home hygiene and fitness. The title of the company’s press release about the program also included the fact that many of the products would be priced as low as $1.99. So financial wellness is also baked into the Target strategy. Globally, the wellness market is valued at a whopping $1.8 trillion according to a report published last week by McKinsey. McKinsey points to five trends
The Trust-Innovation Gap – Welcome to the 2024 Edelman Trust Barometer
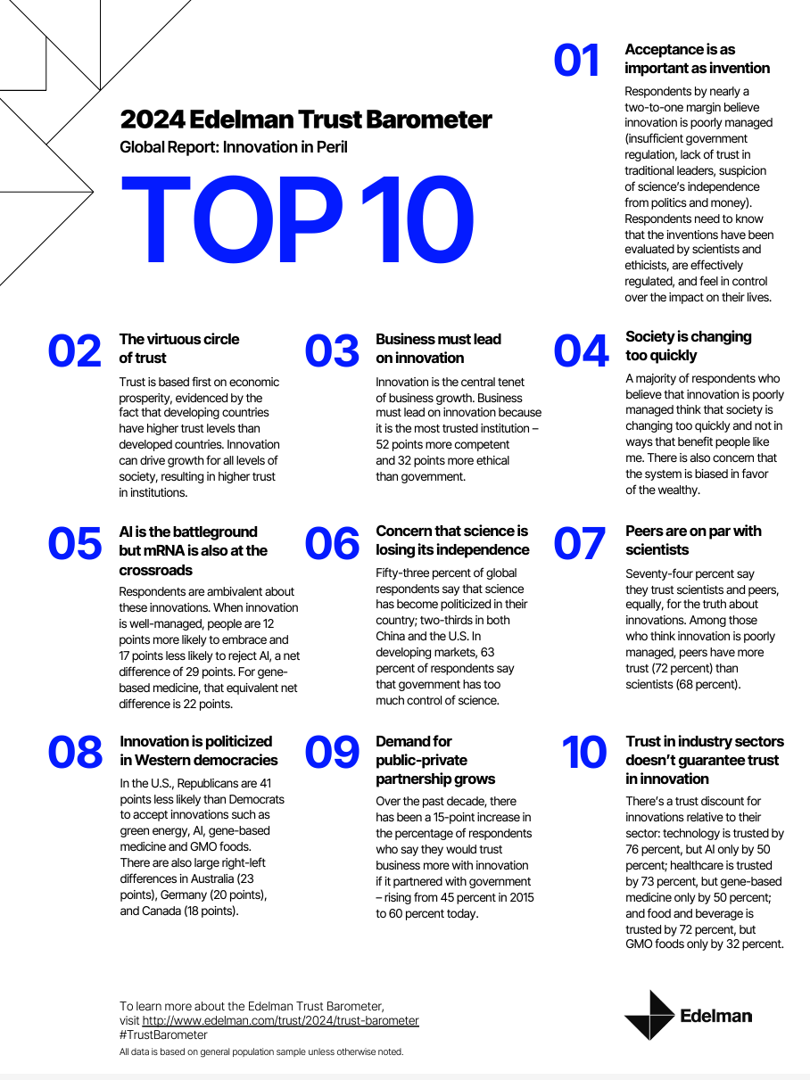
If it’s January, it’s Davos-time — that is the annual meeting of the World Economic Forum convening global experts and passionistas focused on big ideas and challenges facing us mere humans living on Planet Earth. Parallel with the WEF is the annual publication of the 2024 Edelman Trust Barometer, now in its 24th year, focusing on global citizens’ concerns that unite people around the world. For the 2024 study, Edelman’s team fielded the survey in November 2023, collecting input from over 32,000 people living in 28 countries. About 1,150 interviews (plus or minus) were done in each nation which included
In 2024 U.S. Consumers Will Mash Financial Resolutions With Those For Physical Health and Mental Health, Fidelity Finds
One-third of U.S. consumers feel in worse financial shape now than in 2022, with inflation a top concern, discovered in the 2024 New Year’s Financial Resolutions Study from Fidelity Investments. In this 15th annual update of Fidelity’s research into Americans’ New Year’s resolutions for financial health, we learn the mantra that 2024 will be the year of living practically, opening new chapters for saving and paying down debt. Fidelity conducted an online poll among 3,002 U.S. adults 18 and over in October 2023 to gauge peoples’ perspectives on personal finances, and well-being currently and into 2024. This
Healthcare Bills, Affordability, and Self-Rationing Care Will Continue to Challenge U.S. Health Consumers in 2024
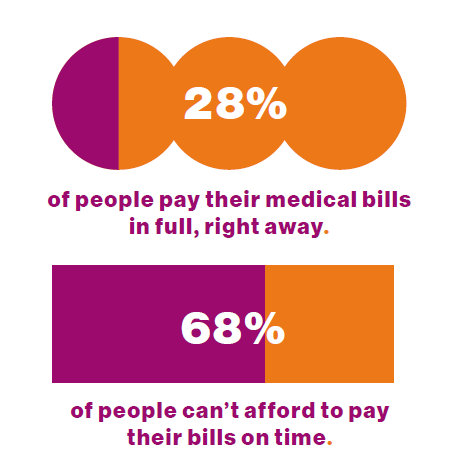
Two-thirds of U.S. consumers say they can’t afford to pay their medical bills on-time, based on the 2023 Consumer Survey from Access One, a financial services company focused on healthcare payments. The report’s title page asks the question, “What options do consumers really want for paying healthcare expenses?” The survey report responds to that question, finding out that nearly one-half of patients have taken some kind of action to reduce their medical expenses. Furthermore, one-third of consumers are not confident they could pay a medical bill of $500 or more. Access One fielded
Accenture’s Great Expectations for a Decade of Deconstruction – the 2024 Life Trends Forecast
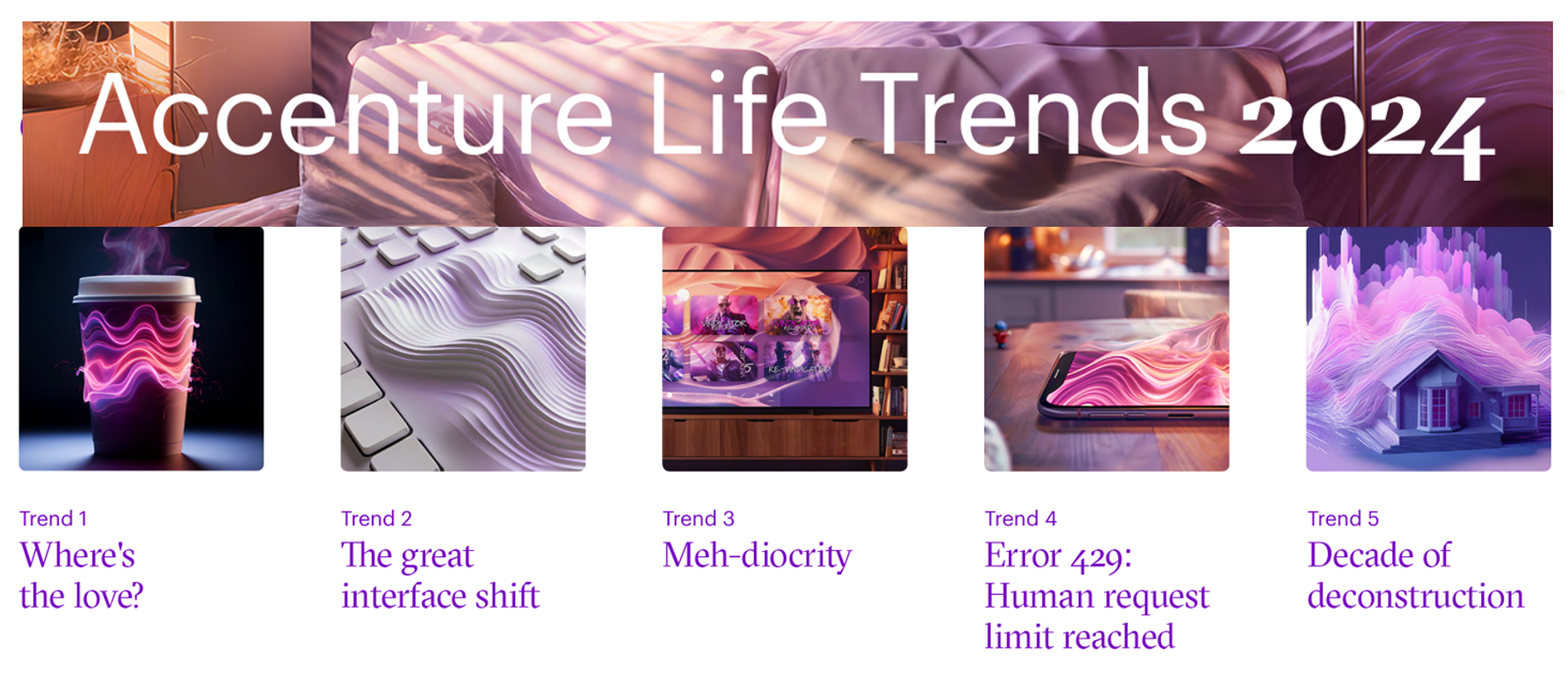
In the company’s 17th annual look into consumers’ “life trends,” Accenture finds that, top-line, “The harmony between people, tech and business is showing tensions, and society is in flux.” And these consumer-facing trends will also shape peoples’ attitudes about their health care, how they access and pay for it, and what kinds of services and support health consumers will expect in this era of “deconstruction.” Taken together, the trends noted in Accenture’s 2024 report on Life Trends finds that one-half of consumers, globally, are changing their life goals, making their jobs and retirement stability more important than
Everybody is Stressed in America, and It’s Not Good for Our Health: the 2023 Update from the American Psychological Association

The U.S. is “a nation recovering from collective trauma,” the according to the latest survey on Stress in America 2023 from the American Psychological Association (APA). The APA has been quantifying Stress in America since 2007; for context, at the end of that year The Great Recession kicked in, and in response President Obama’s team put together assistance to bolster the national economy, jobs, and health technology (codified in the American Recovery and Reinvestment Act). American health citizens are experiencing a deja vu in 2023 akin to their financial stress experienced in the APA 2008 Stress
The 2023 Health Economy – The Evolving Primary Care and Retail Health Convergence Through Trilliant Health’s Lens
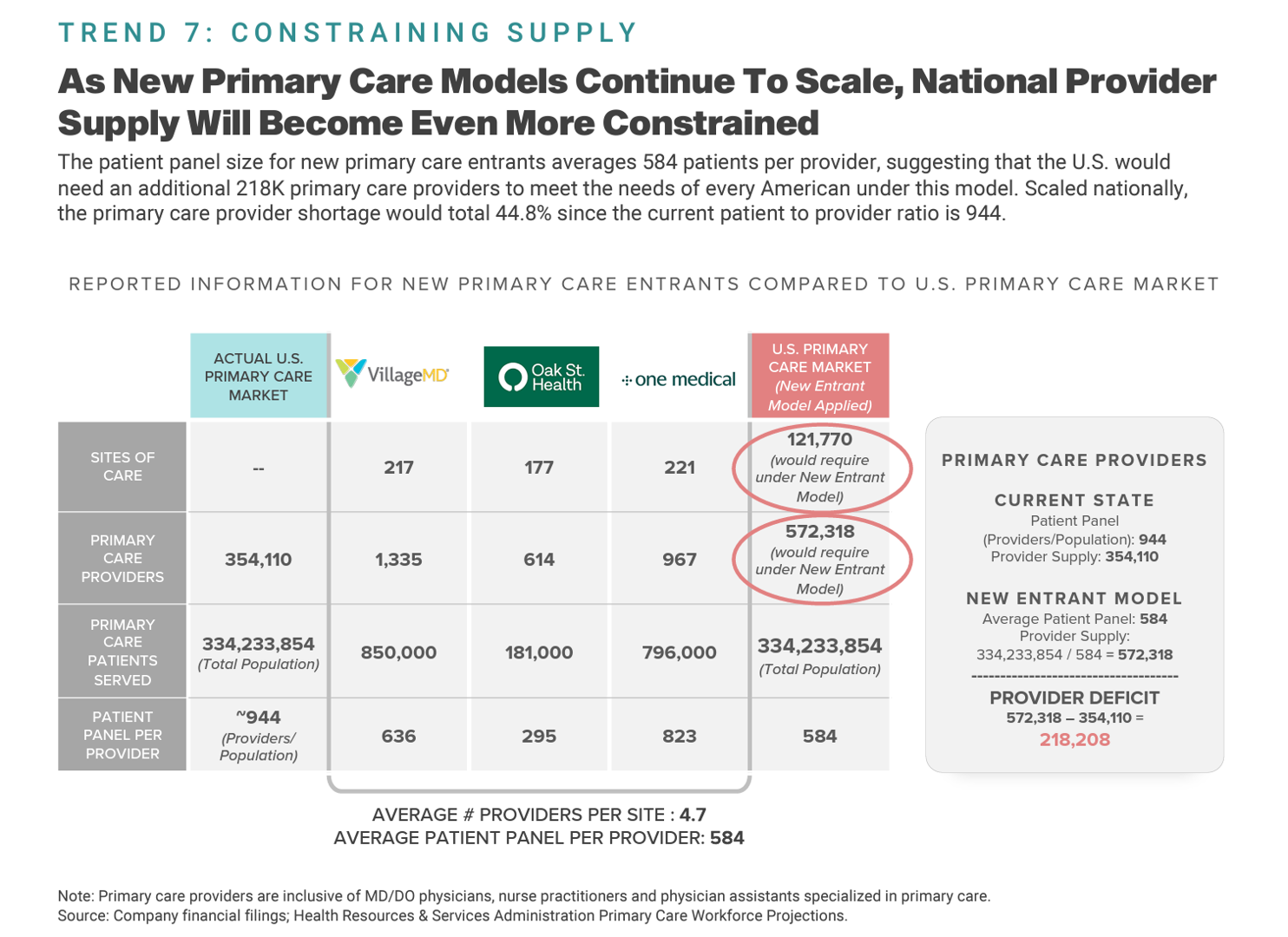
In U.S. health care’s negative-sum game, stakeholders who survive and win that game will have to deliver value-for-money, we learn from Trilliant Health’s 2023 Trends Shaping the Health Economy Report. “Report” is one word for this nearly 150-page compendium of health care data that is an encyclopedic treasure trove for health service researchers, marketers, strategists, journalists, and those keen to explore questions about the current state of health care in America. As Sanjula Jain points out in the Report’s press release, the publication resembles another huge report many of us appreciated for
The Healthcare Financial Experience is a Stressful One: the Convergence of our Medical, Retail, and Financial Lives
One in two consumers in the U.S. feel their well-being or healing was negatively impacted by difficulty paying for their medical care. Welcome to the convergence of patients’ health care life with financial and retail lives, we learn from the 2024 Healthcare Financial Experience Study from Cedar. And that patient’s positive clinical experience can absolutely reverse the consumer’s perception of the provider, noted by this quote from OSU’s Chief Financial Officer Vincent Tammaro: “We’ve cured you of your ailment, but we’ve harmed you financially.” That’s a form of financial toxicity that
Slip Slidin’ Away: the Reputations of Pharma and Healthcare in the U.S. Decline in the Latest Gallup Poll
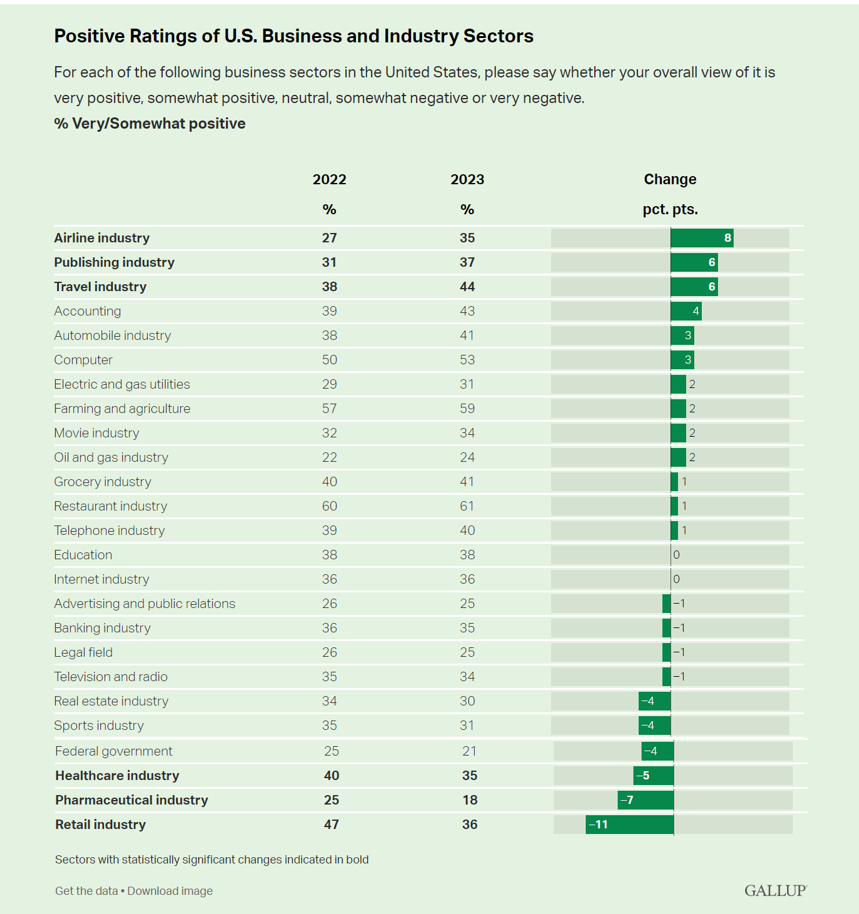
Oh, how quickly people forget…and slow to forgive. U.S. consumers’ positive views for healthcare, pharma and retail have significantly fallen in just one year, the latest annual Gallup poll of industry rankings in America found as of August 2023. This stat for the pharma industry was the lowest Gallup ever recorded for the sector since 2001. I can’t help hearing Paul Simon’s lyrics to Slip Slidin’ Away….”you know the nearer your destination, the more you’re slip slidin’ away” when it comes to health citizens’ perceptions of pharma and the healthcare
“Healthcare Isn’t Healthy:” the Global Challenge of Health Equity, and Calls-to-Action
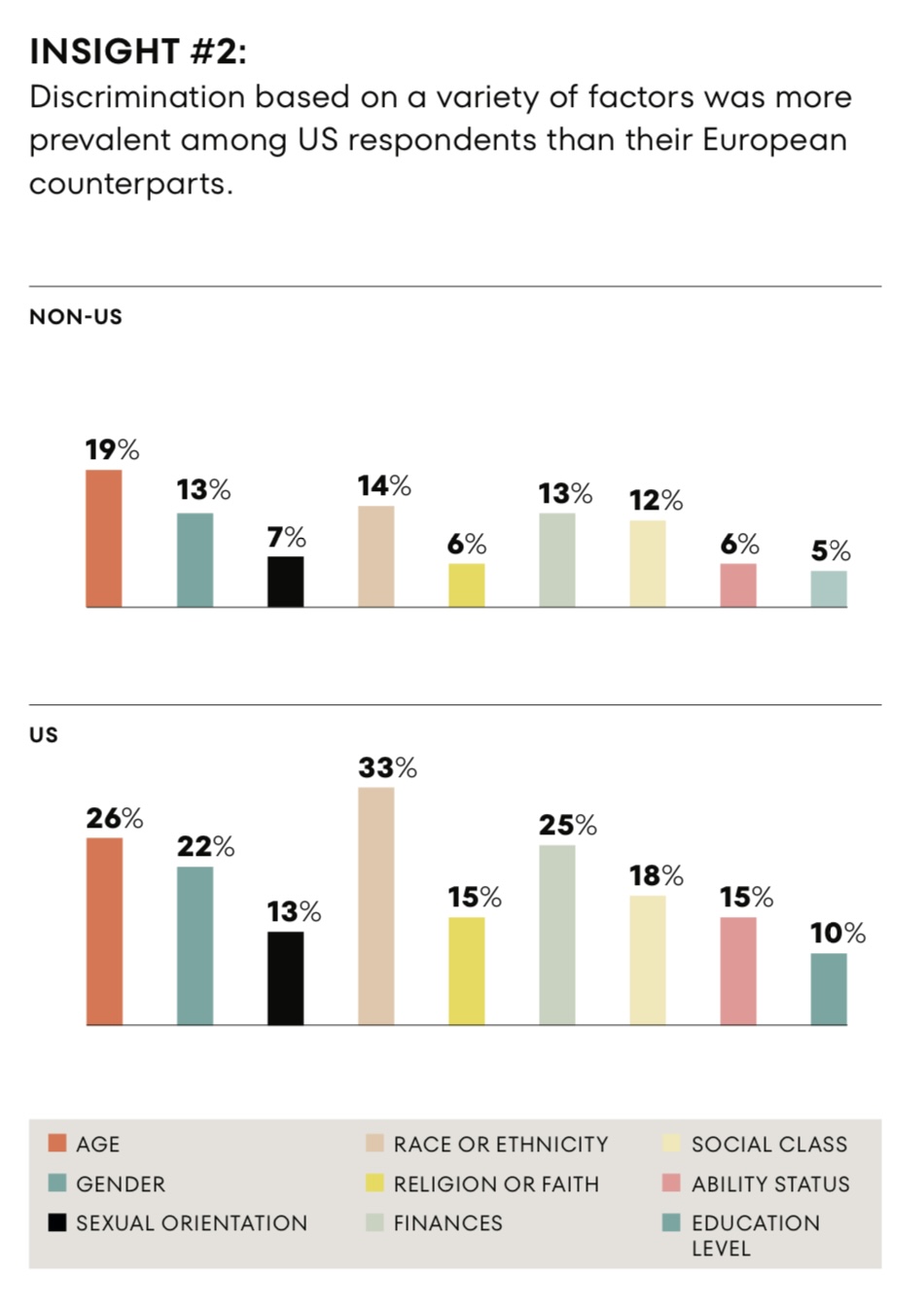
Discrimination in health care is reported by more people in the U.S. than in Germany, Spain, or the U.K., we learn in the research reported in The Intersection of Health Equity in Communities & Business Strategy: A Call-to-Action, from Omnicomm PR Group (OPRG) and Atlantic Insights. The study was conducted among 6,000 people living in Germany, Spain, the United Kingdom and the United States, fielding 1,500 interviews in each of the four countries in March 2023. The U.S. survey sample included 375 people identifying as Black, White, Hispanic, or
For Public Health, U.S. Consumers See Opioids, Obesity, and Guns Top 3 Public Health Threats – But Lowering Healthcare & Drug Costs is Job 1 for Government
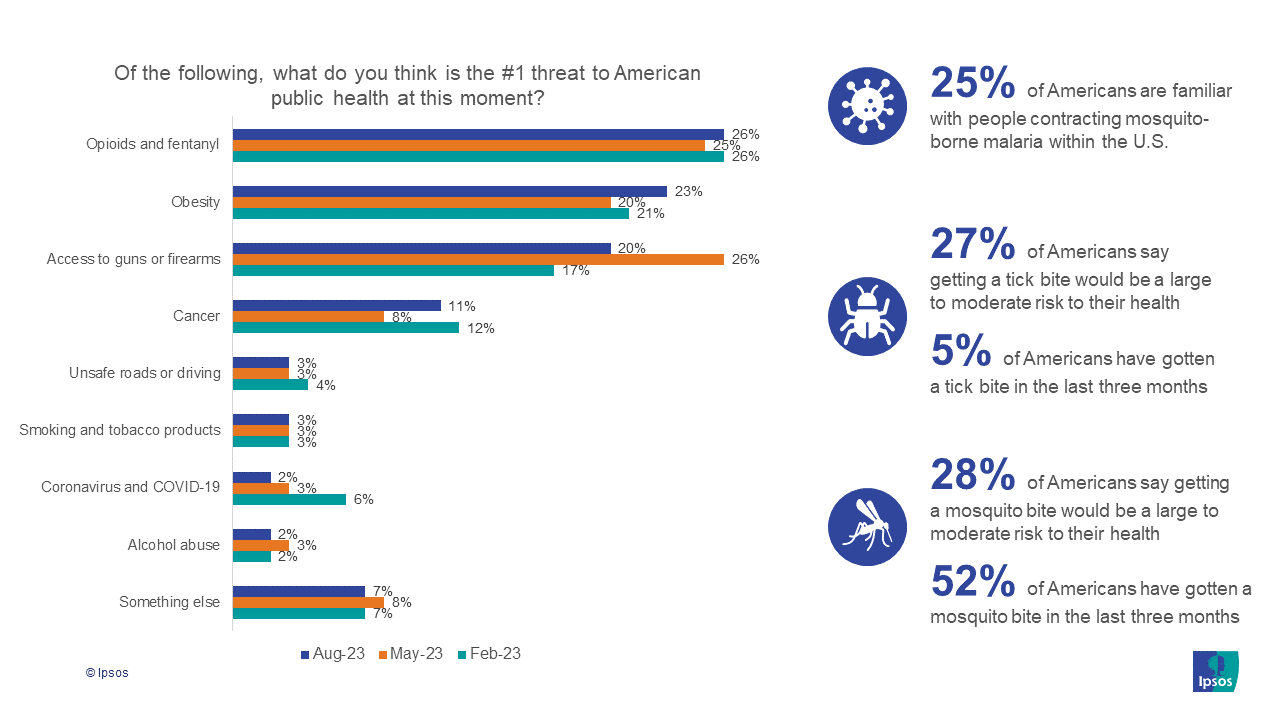
Americans cite opioids and fentanyl, obesity, and access to guns and firearms as the top three public health challenges this summer of 2023, according to the new Axios/Ipsos American Health Index. As for government priorities dealing with public health, though, U.S. health citizens say the top priority should be lowering the costs of health care and prescription drugs. Once again, we see evidence that U.S. consumers bundle their financial wellbeing — in this instance, costs of medical services and medicines — into peoples’ overall sense of health for themselves as individuals and for
Because of Winn-Dixie, Will ALDI Expand Its Healthcare Footprint? Not Likely Through Pharmacy….

This week ALDI, the global food discount group, announced they would acquire Winn-Dixie and Harveys Supermarket stores. In response to the deal, Supermarket News said that ALDI “is shaking up the grocery sector with its acquisition” of the Winn-Dixie chain. That statement was focused on the overall food chain landscape, where Winn-Dixie has played a significant role in the traditional brick-and-mortar grocery business. ALDI has generally served a value-oriented segment of consumers, which industry analyst have categorized as a separate food channel based on consumer segmentation. In addition to the overall “shaking up” of the
Large Employers Expect More Employees Will Experience Prolonged Health Impacts Due to COVID-19. and a Note About Telehealth Engagement
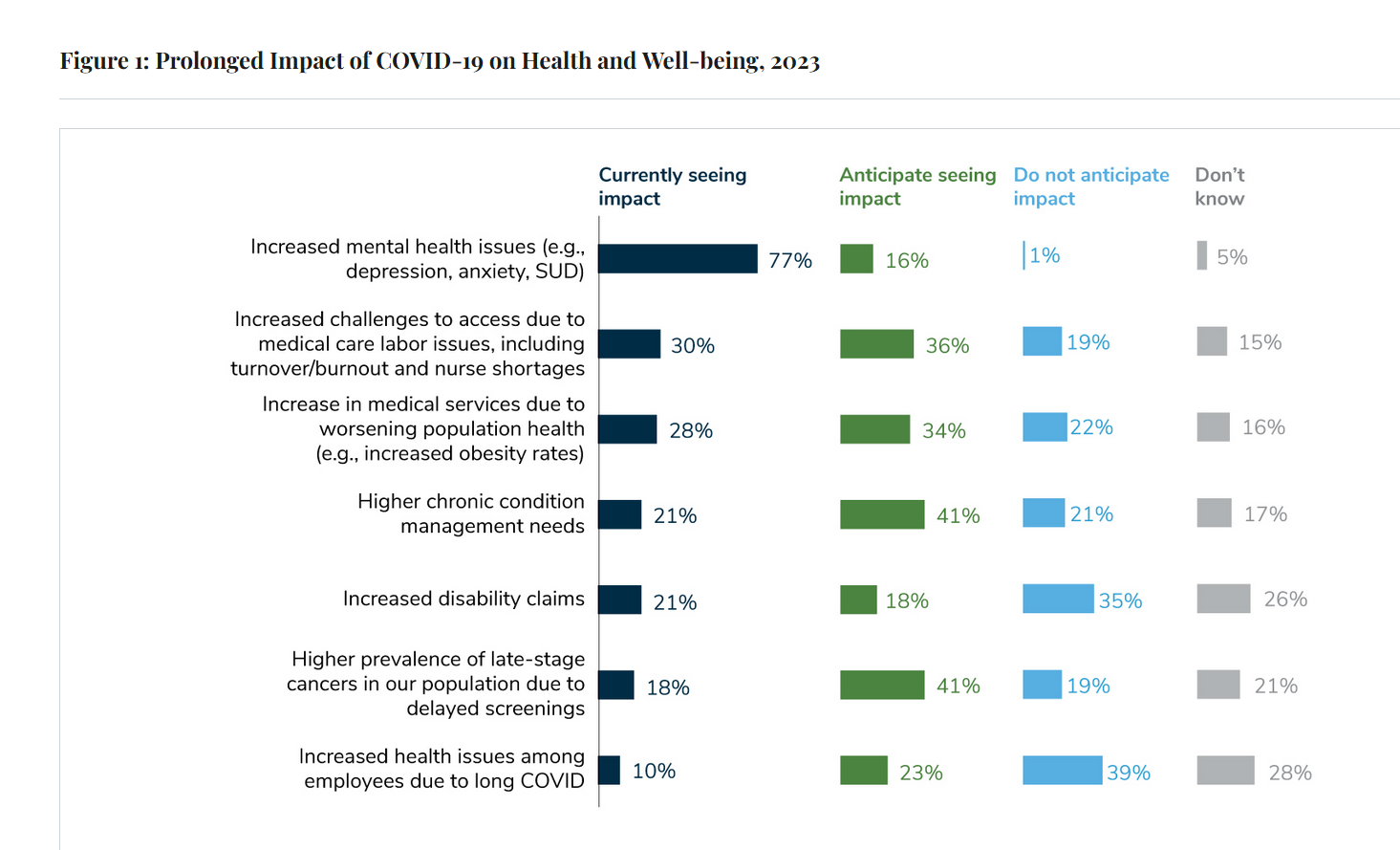
Due to their delayed return to medical services and diagnostic testing in the COVID-19 pandemic era, U.S. employees are expected to sustain serious health impacts that will drive employers’ health care costs, envisioned in the 2024 Large Employer Health Care Strategy Survey from the Business Group on Health (BGH). Dealing with mental health issues is the top health and well-being impact workers in large companies are addressing in 2023. Looking forward, large employers foresee their workers will be seeking care for chronic conditions and later-stage cancers that are diagnosed due to delayed screenings.
A Tale of Barbie, Beyonce and Taylor, the Economy and the Gynecologist
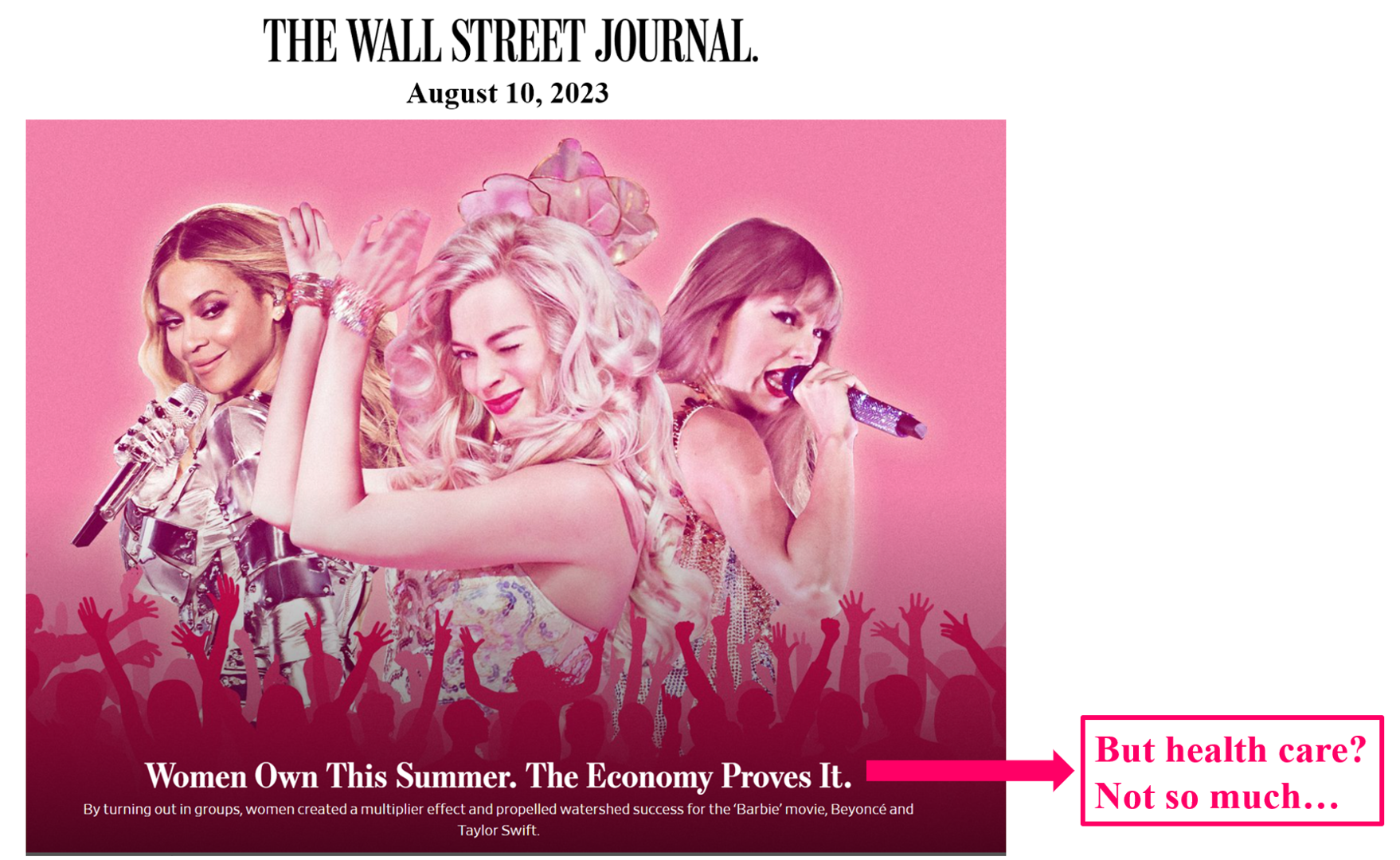
This weekend’s Wall Street Journal Saturday/Sunday edition featured a big story on the economic force of women in the summer of 2023, termed “the women’s multiplier effect” — that women’s spending is a powerful force in the U.S. economy (and as it turns out, in Sweden’s economy as well). The article was titled, “Women Own This Summer. The Economy Proves It,” and featured a Photoshopped image in various shades of pink with Margot Robbie as Barbie in the center, flanked by Beyonce to the left and Taylor Swift to the right. I’m
GNC Offers “Free Healthcare” — Telehealth, Generic Meds, and Loyalty in the Retail Health Ecosystem
The retail health landscape continues to grow, now with GNC Health offering a new program featuring telehealth and “curated set” of 40+ generic prescription drugs commonly used in urgent care settings. The services are available to members of GNC’s new-and-improved loyalty program, GNC PRO Access, which is priced at a fixed fee of $39.99 for one year’s membership. This is available to consumers 18 years of age and older. “As a trusted brand in the health and wellness space, we are thrilled to expand our efforts in helping our customers Live Well by offering
Happy 75th Birthday, NHS – Through A U.S. Health Care Lens
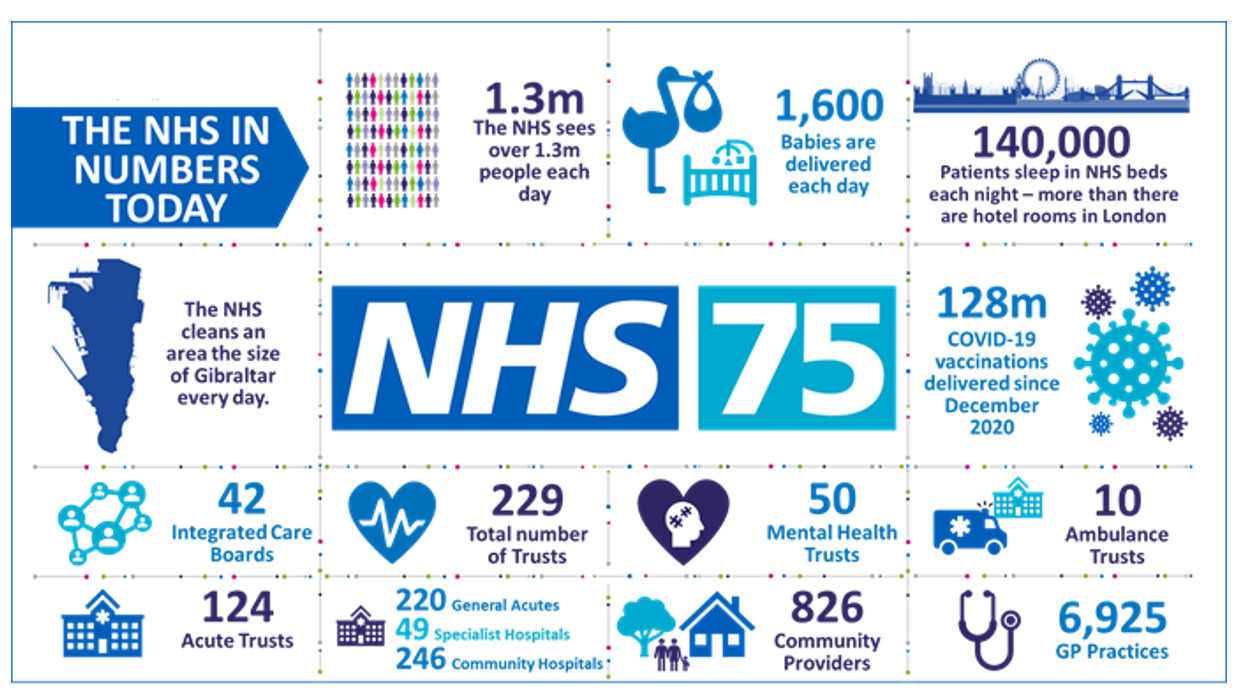
The UK’s National Health Service (NHS) turns 75 today. The NHS was the brainchild of Minister of Health Aneurin Bevan; he wrote in a statement to doctors and nurses in The Lancet on July 3, 1948, “My job is to give you all the facilities, resources, apparatus and help I can, and then to leave you alone as professional men and women to use your skill and judgement without hindrance.” This week in The Lancet, the editors assert, “The founding principles of the NHS put into practice 75 years ago are at risk of
The Cost of Treating Patients is On the Rise: PwC Goes What’s Behind the 2024 Medical Spending Numbers
Health care cost trend will spike up another percentage point to 7.0% in 2024, according to the annual report from the PwC Health Research Institute, Medical cost trend: Behind the numbers 2024. Every year, the PwC HRI team goes behind those numbers to assess cost inflators and deflators which underpin annual medical inflation. As the first line chart illustrates, the peak of medical trend in the last 18 years was in 2007 when the U.S. saw double-digit cost growth of nearly 12%. Here’s a link to PwC’s 2007 study looking behind the
Technologies That Bolster Health Will Be Baked Into the Fourth Industrial Revolution: Listening to the World Economic Forum

The technologies that will drive the Fourth Industrial Revolution have health baked into most of them, based on the Top 10 Emerging Technologies of 2023, a flagship report from the World Economic Forum, Two of the ten technologies making up this forecast directly speak to health and health care” AI-facilitated healthcare, and The metaverse for mental health. But seven of the remaining eight all address health somewhere in their discussions, and even the tenth non-obvious tech — #3, sustainable aviation fuel — would resonate with many researchers working on the opportunity
The Latest KFF Poll on Consumer Experiences with Health Insurance Speaks Volumes About Patients’ Administrative Burden
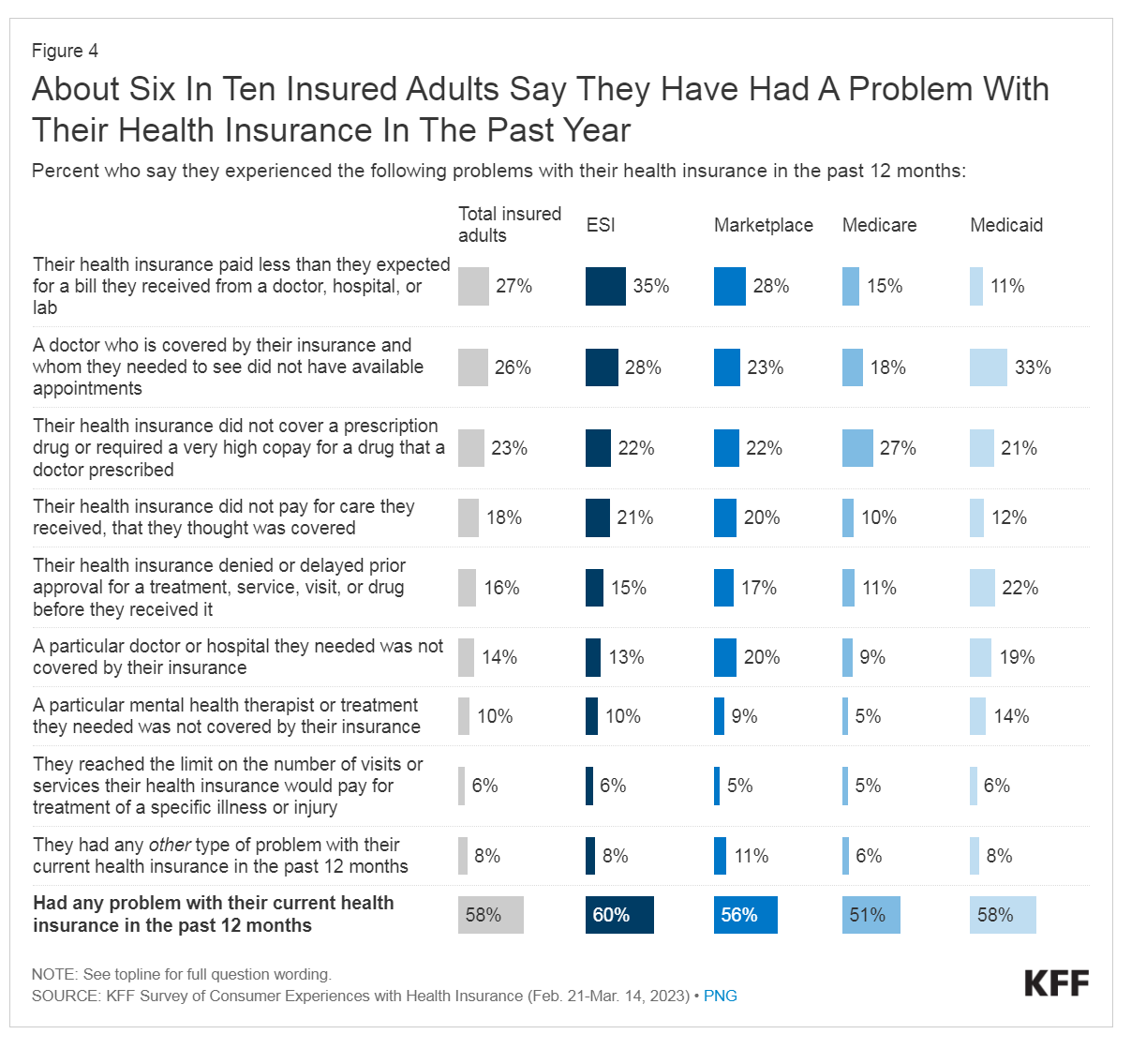
People love being health-insured, but their negative experiences with health plans create serious burdens on patients-as-consumers. And those burdens impact even more people who are unwell than healthier folks. The 2023 Kaiser Family Foundation Survey of Consumer Experiences with Health Insurance updates our understanding of and empathy for insured peoples’ Patient Administrative Burdens (PAB). For this study, KFF polled 3,605 U.S. adults 18 and over in February and March 2023 who had health insurance across different plan types. Over the past several years, I’ve come to appreciate the concept of PAB by listening to and learning from colleagues Dr, Grace
The State of Healthcare in America, State-By-State
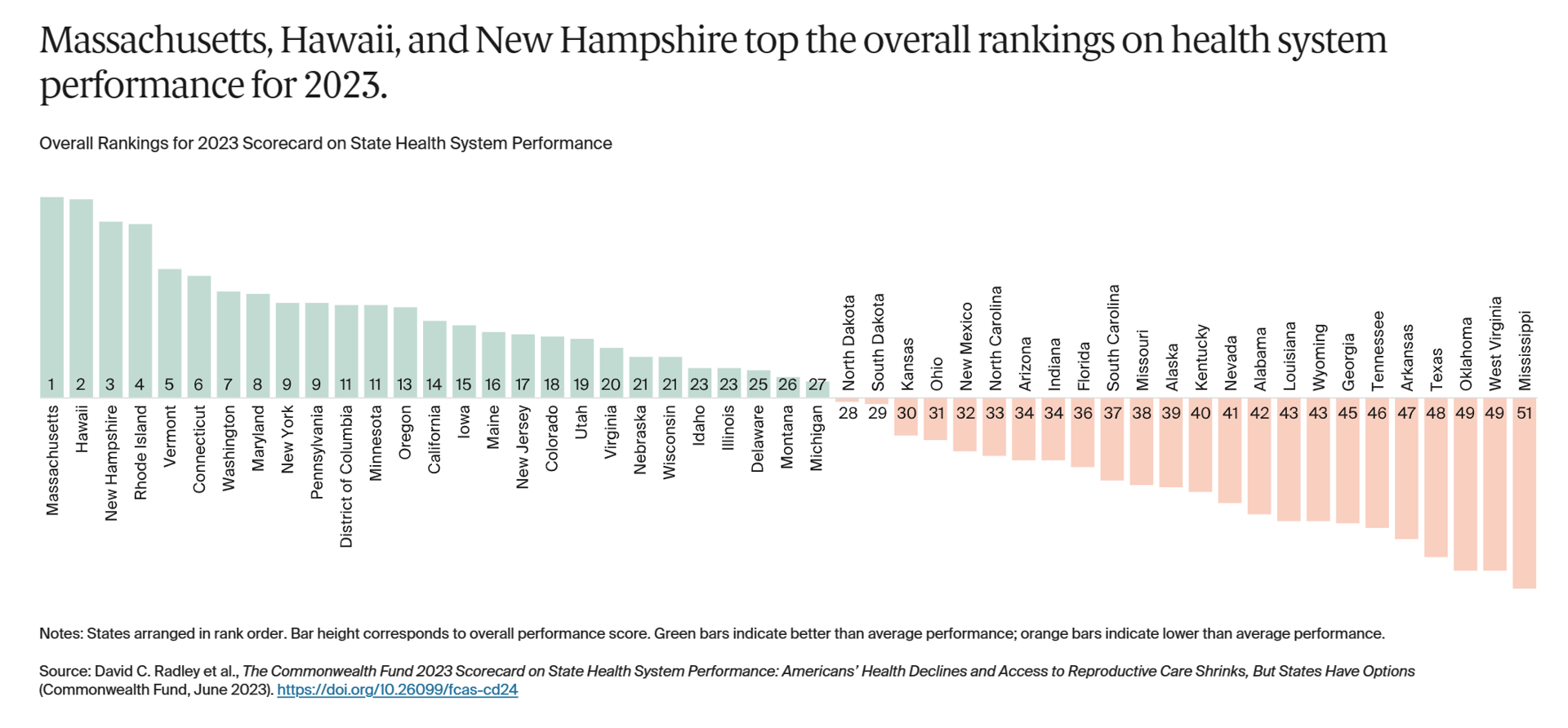
If you live in Massachusetts, Hawaii, and New Hampshire, you win a kind of state lottery for public health and well-being, based on this year’s read of the 2023 Scorecard on State Health System Performance from The Commonwealth Fund. Here’s a picture of the annual study’s top-line findings, a roster of the fifty U.S. states ranked by a mash-up of health system indicators. As Annie Burkey of FierceHealthcare succinctly summed it up, the “Commonwealth Fund gives healthcare in southeastern states failing grades across the board.” I’ll give you more details about the Top and Bottom
Patients-As-Health Care Payers Define What a Digital Front Door Looks Like
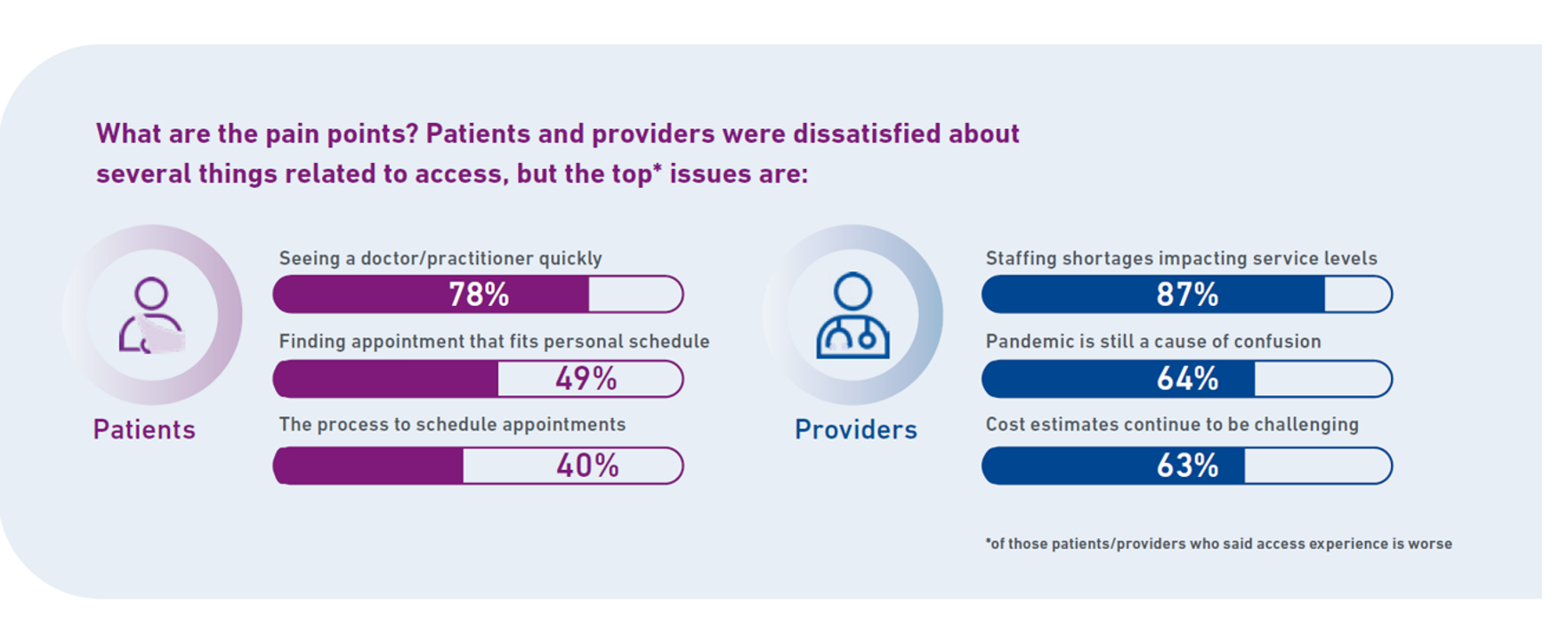
In health care, one of the “gifts” inspired by the coronavirus pandemic was the industry’s fast-pivot and adoption of digital health tools — especially telehealth and more generally the so-called “digital front doors” enabling patients to access medical services and personal work-flows for their care. Two years later, Experian provides a look into The State of Patient Access: 2023. You may know the name Experian as one of the largest credit rating agencies for consumer finance in the U.S. You may not know that the company has a significant footprint
What $31,065 Can Buy You: a Toyota Corolla Cross Hybrid, a Year at Gnomon School, or Healthcare for a Family of 4 in America
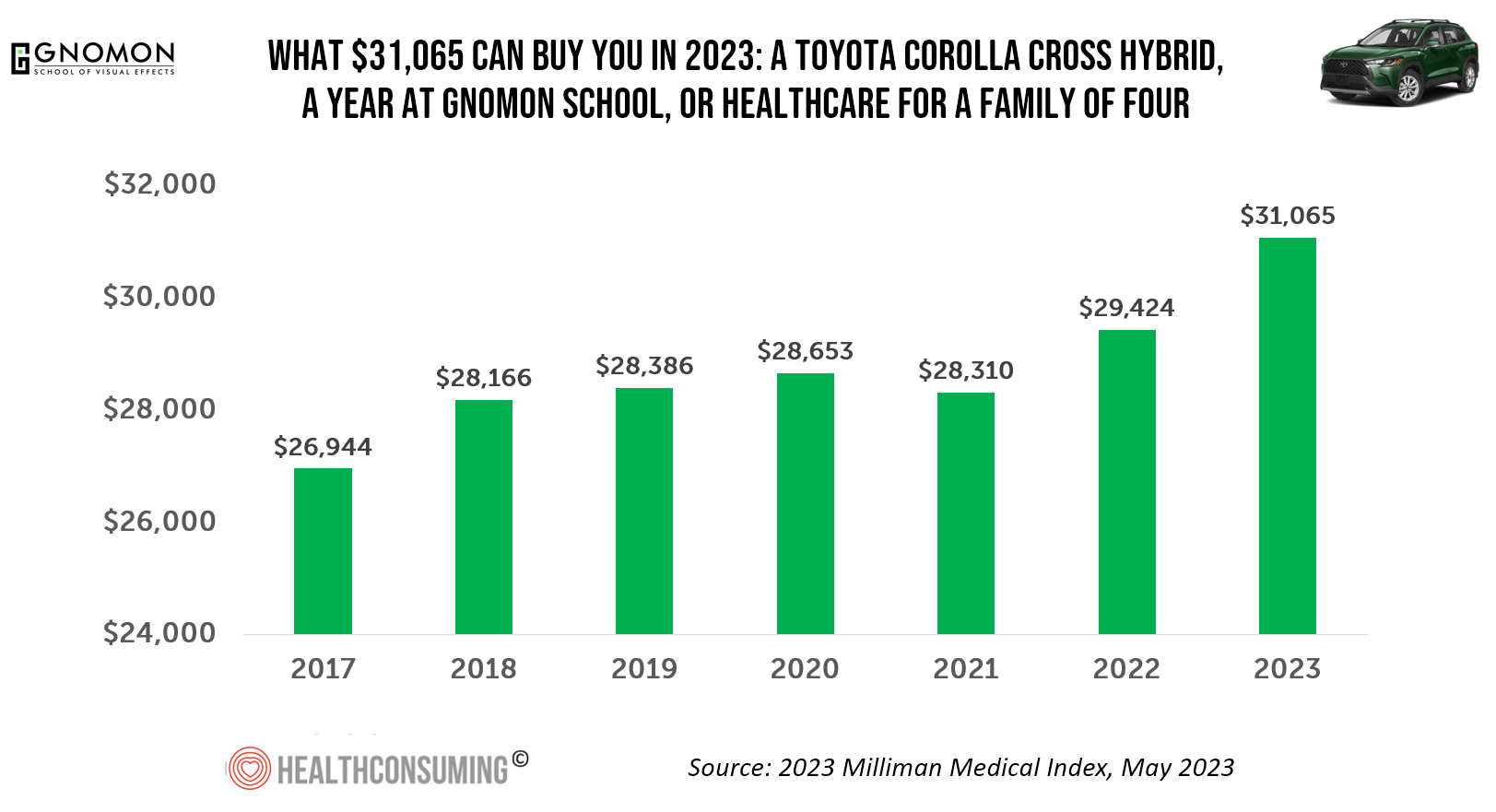
“Healthcare costs came roaring back in 2021” after falling in 2020. In 2023, that roaring growth in health care costs continues with expected growth of 5.6%. For 2023, you could take your $31K+ and buy a Toyota Corolla Cross Hybrid auto, fund a year at the Gnomon School in Hollywood toward a degree in animation or game design, or buy healthcare for your family of 4. Welcome to this year’s annual look at health care costs for a “typical” U.S. family explained in the 2023 Milliman Medical Index (MMI).
Retail Clinics’ Growing Role in Health Care and Prescription Drug Sales
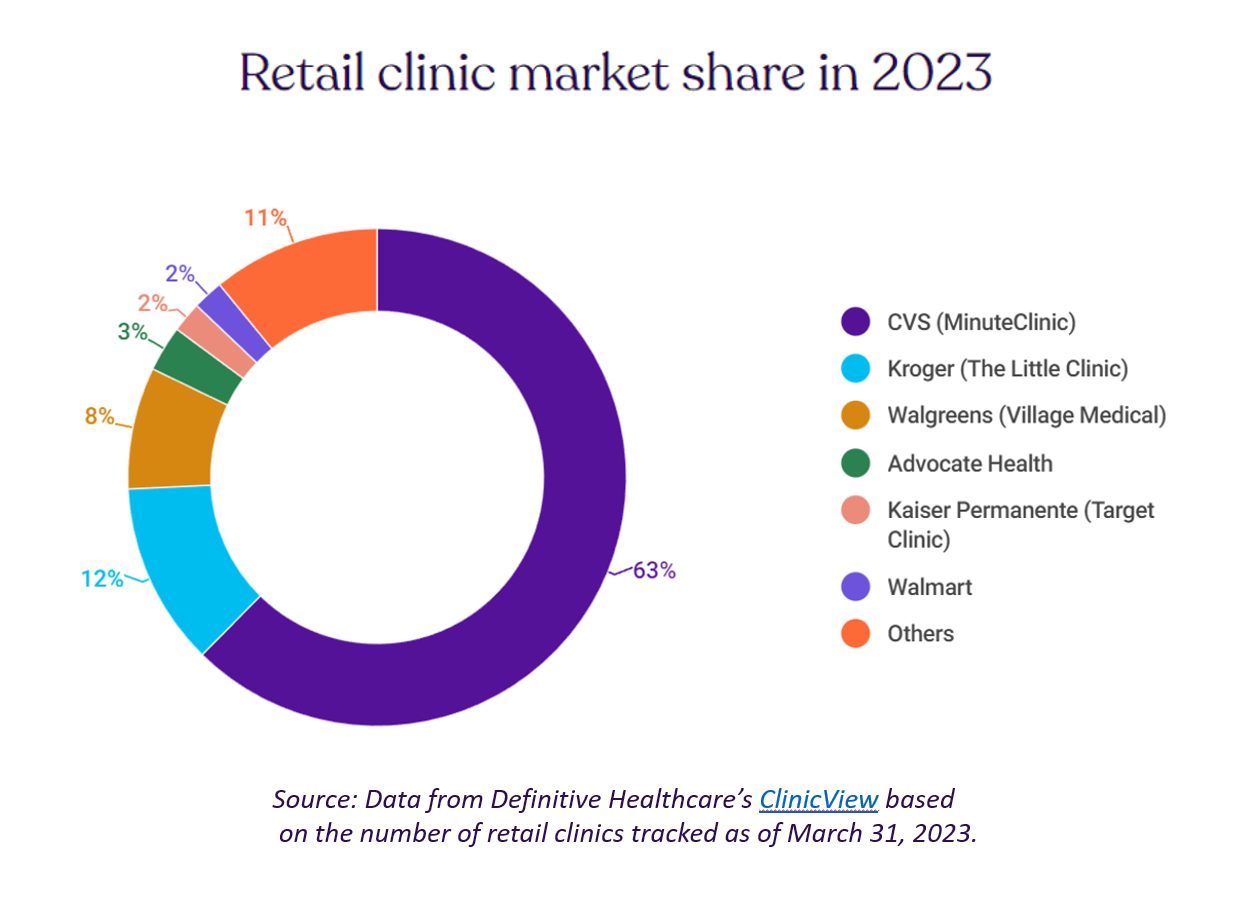
“It seemed like an odd pairing: shampoo and a throat swab,” observes a new report on the growth of retail health from Definitive Healthcare. But retail clinics are no longer, as the paper explains, “an experiment of a few grocery stores….they’re becoming a major force in the U.S. healthcare system,” asserts the thesis of Retailers in healthcare: A catalyst for provider evolution. While the use of emergency departments fell by 1% in the past five years, the use of retail clinics expanded by 70%, Definitive Healthcare calculated. Most retail clinics are owned by
Medical Debt: “The Debt of Necessity” – A Current U.S. Picture from the CFPB
On April 11, 2023, three of the largest U.S. consumer credit rating companies — Equifax, Experian and TransUnion — planned to remove medical bill collections that were under $500 from consumers’ credit reports. The Consumer Financial Protection Bureau (CFPB) calculated that these medical bill “erasures” under $500 impacted nearly 23 million consumers and eliminated medical collections totally for 15.6 million people in the U.S. according to CFPB’s recently-published Data Point report. For some context, it’s useful to know that the CFPB was created as part of the Dodd-Frank Wall Street Reform and Consumer Protection Act passed by Congress and signed
Virtual Health Care Can Reduce Carbon Emissions: the Environmental ROI on Telehealth
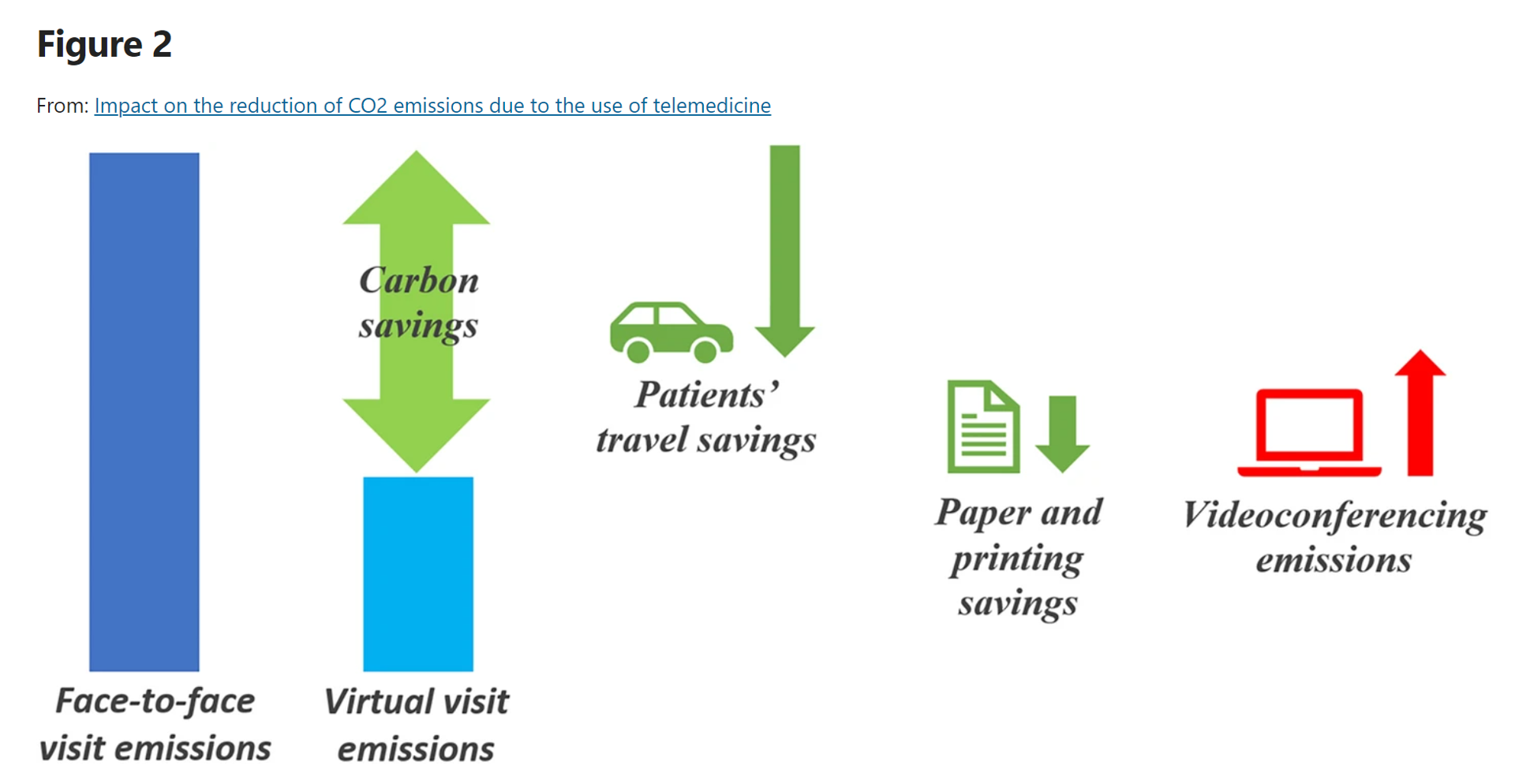
As implemented in the COVID-19 era and its immediate wake, the most obvious environmental benefits offered by telehealth visits replacing in-person patient encounters have been achieved through reduced patient travel, considering The Role of Virtual Consulting in Developing Environmentally Sustainable Health Care, a systematic literature review published in the Journal of Medical Internet Research. This study, led by researchers at the University of Oxford, UK, and the University of Oslo, Norway, identified over 1,600 scientific papers, narrowing the most rigorous and relevant to 23 papers focusing on virtual consulting and carbon emissions. This is an important question for two major
Women’s Health on Her Own Terms – “She Knows” What She Needs

Despite some improvement in the representation of women by cinema, TV shows, and brands, distortions in media remain that are risks to women receiving appropriate health care. Breaking through taboos of weight, reproductive services, and mental health are the top 3 factors preventing women from getting proper care, according to Health On Her Terms, a research study from WPP and Ogilvy partnering with SeeHer, an organization of collaborations from media, technology, business, education, and other sectors (including over 7,000 brands) focused on the accurate portrayal of women and girls in society. Taglined as “The Marketer’s Hippocratic Oath to Women, the
Health Care Financing: How Inflation and Health Care Prices Could Hit the U.S. Consumer
In the U.S. in 2021, per person health care spending increased by nearly 15%, reversing 2020’s spending decline of 3.5% in the first year of the COVID-19 pandemic. The latest Health Care Cost and Utilization Report from the Health Care Cost Institute (HCCI) details health spending in 2021, dissecting the change in terms of utilization of services and prices by category. That’s a big rise over consumers’ household inflation for food, energy, and other kitchen-table considerations, prompting me to look for additional context from a recent paper published by the OECD on Health care financing in times of high inflation,
Consumers Expect Every Company to Play a Meaningful Role in “My Health” – New Insights from the 2023 Edelman Trust Barometer

People have expanded their definitions of health in 2023, with mental health supplanting physical health for the top-ranked factor in feeling healthy. Welcome to the Edelman Trust Barometer Special Report: Trust and Health, released this week, with striking findings about how the economic, post-pandemic life, pollution and climate change all feed mis-trust among citizens living in 13 countries — and their eroding trust for health care systems. While these factors vary by country in terms of relative contribution to citizen trust, note that in the U.S., social polarization plays an outsized role in factors that “make us
More Consumers Expect Health/Care Companies to Be Purpose-Ful Versus All Other Industries
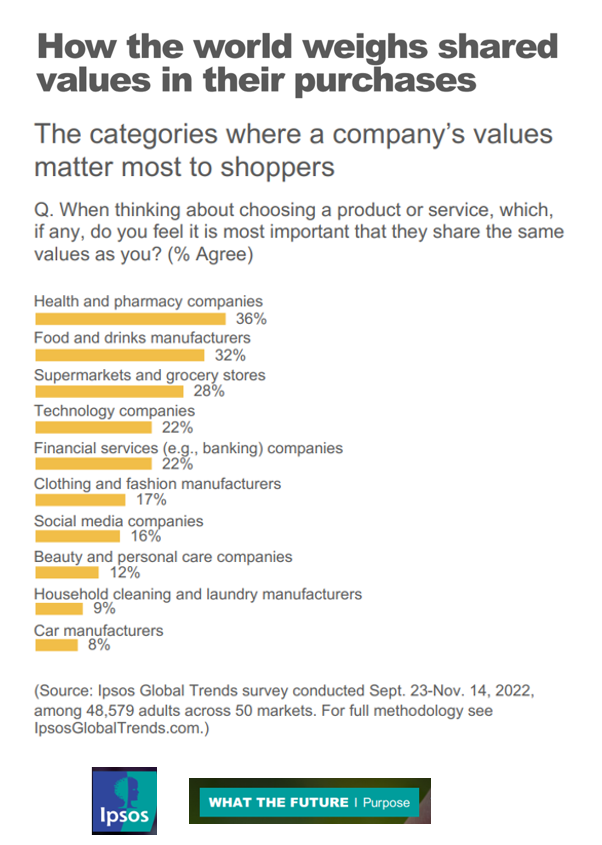
If your organization serves health consumers, patients, and caregivers, and you’re asking them to spend money on your services or products, then you’ll do well to be clear on your values and sense of purpose. In the latest Ipsos look into the future of “Purpose,” we find that consumers look most to health and pharmacy companies for shared values, compared with other industries people patronize such as food and grocery, technology and banks. To understand where Ipsos is coming from on this aspect of ESG, we’ll start with their territory map
Don’t Mess with Medicare and Medicaid, Washington: They Remain Popular with Americans Across Party ID
A majority of the U.S. public does not want politicians to “up-end” government-funded health programs, according to the Kaiser Family Foundation’s March 2023 Health Tracking Poll. Social Security, Medicare, and Medicaid all garner most partisans’ support whether identifying as Democrat, Independent, or Republican, KFF found in their monthly poll of U.S. voters ages 18 and over. The survey was conducted online and by telephone among 1,271 U.S. adults between March 14-23, 2023. Among all the important findings in this well-timed poll, I’ll point to the issue of public
Food-as-Medicine Update: How SNAP Members Face Greater Chronic Illness and a “Hunger Cliff”
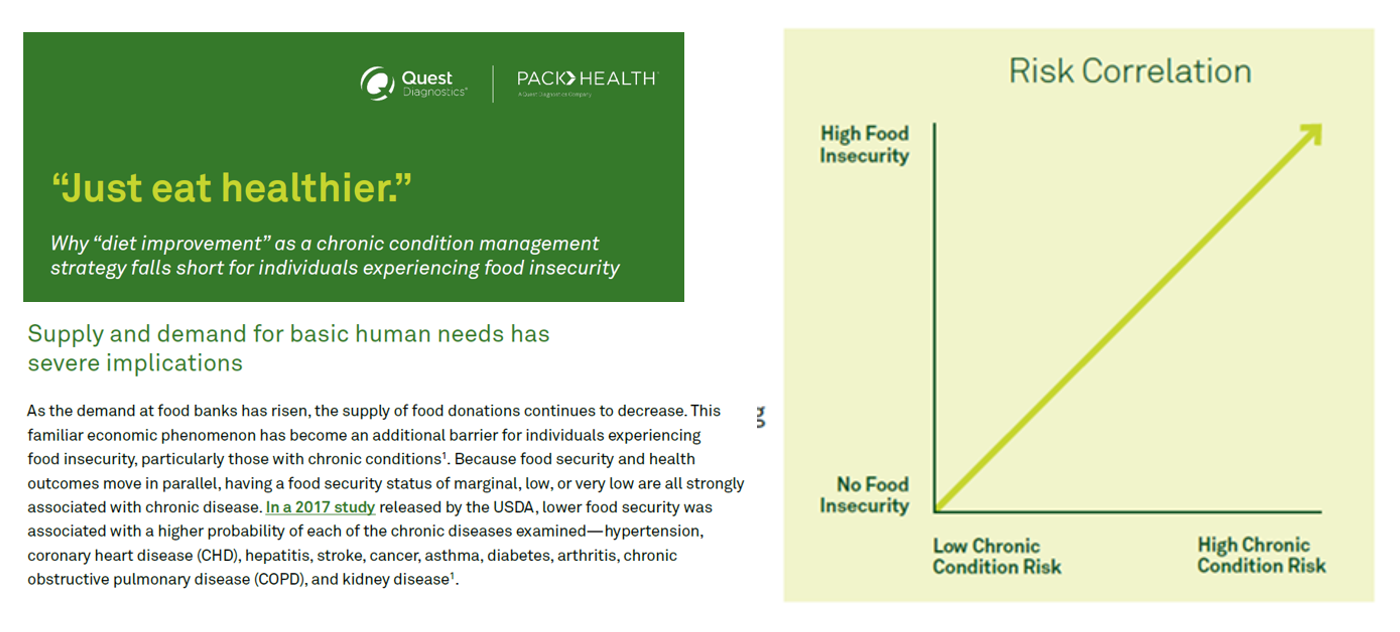
The pandemic worsened food insecurity for many people in the U.S., putting more people at risk for not only hunger but for chronic diseases that can be managed with access to nutritious, fresh food. In Helping SNAP Consumers During Economic Headwinds from Numerator, we get a current read on food security, the SNAP program, and the challenges of chronic health management that are intimately tied. To set some context on this current challenge to peoples’ health, the U.S. is facing the official end of the pandemic emergency on May 11, 2023. At that point, support for government-sponsored programs that have supported
The Patient Is Still the Payor – And May Skip Paying for Prevention (Eyes on the ACA & Texas)
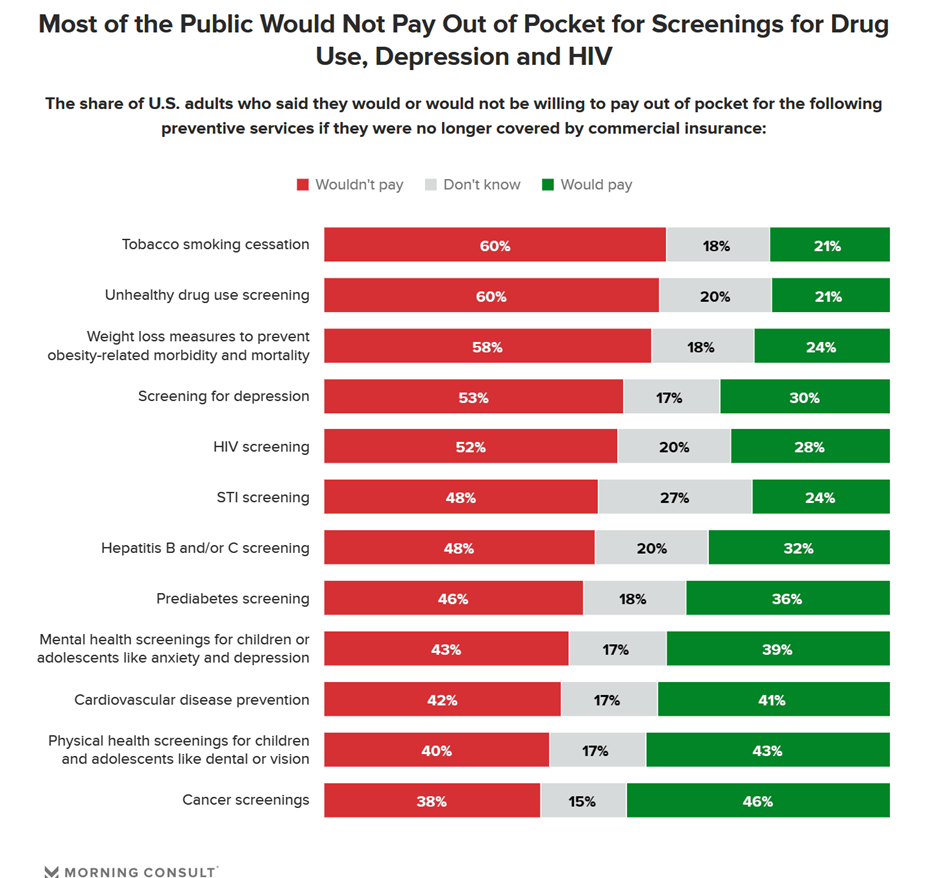
Many health citizens in the U.S. would likely skip receiving preventive health care services if the Affordable Care Act’s (ACA) coverage for them goes away, a Morning Consult survey found. The first chart illustrates the top-line of this research: that most U.S. adults would not pay out of pocket for several preventive services including tobacco cessation, drug use screening, weight loss measures to prevent obesity-related illnesses, as well as screening for depression or HIV. One of the key benefits embedded in the ACA was “free” without co-pay shares for preventive care. These
We Are All Health Consumers Now – Toluna’s Latest Look at Consumers’ Health & Well-Being
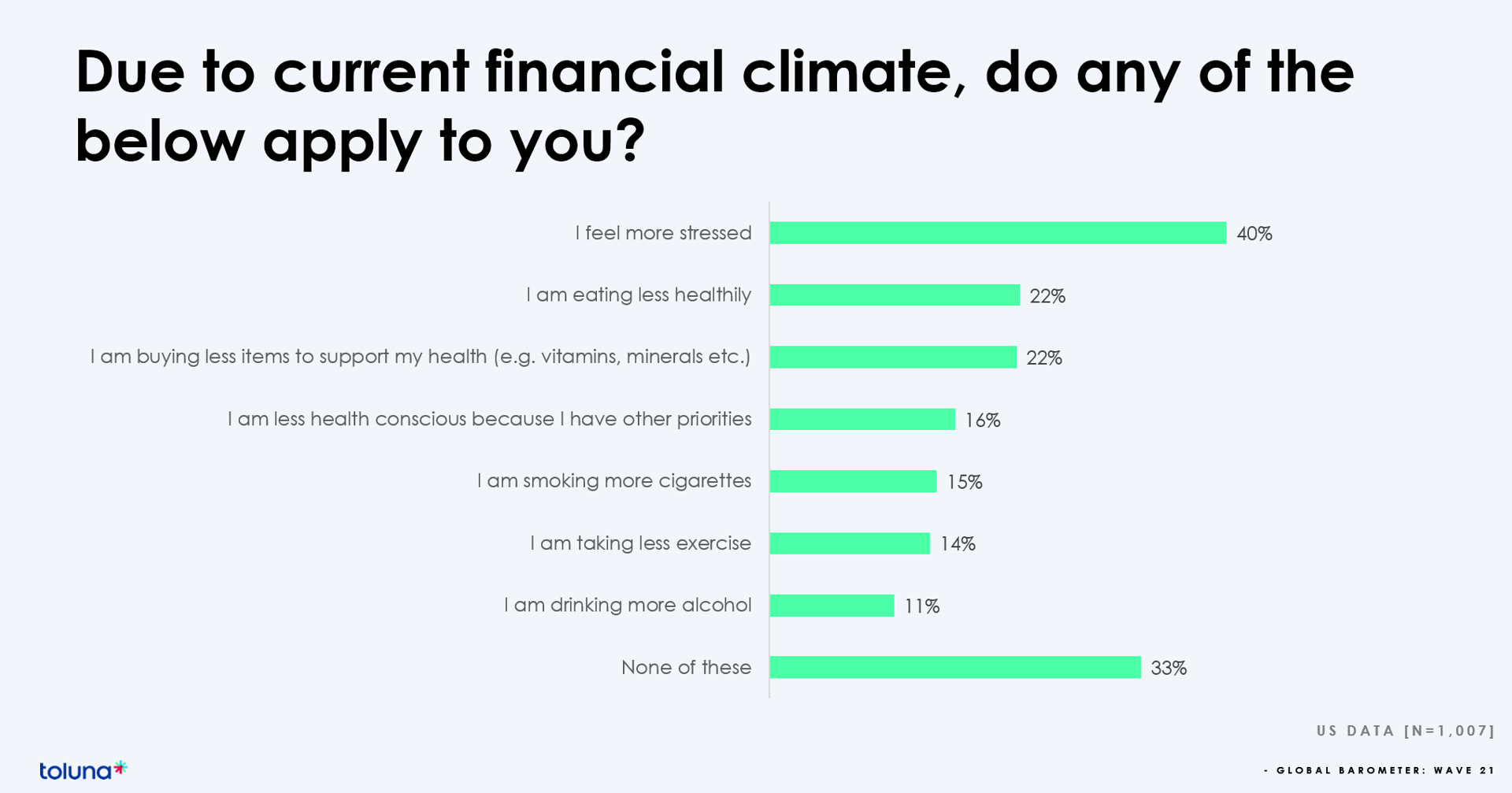
The challenging financial climate at the start of 2023 is impacting how people, globally, are perceiving, managing, and spending money on health and well-being, based on the latest (Wave 21) Global Consumer Barometer survey conducted by Toluna, a sister company of Harris Interactive. Globally, one-third of health citizens the world over are confronting greater stress levels due to the higher cost of living in their daily lives. One in two people say that rising cost of living is negatively impacting their health and well-being. On the positive side, one in three people believe
The Reputation of Pharma Among U.S. Consumers Is Tied More to Pricing Than to Innovation
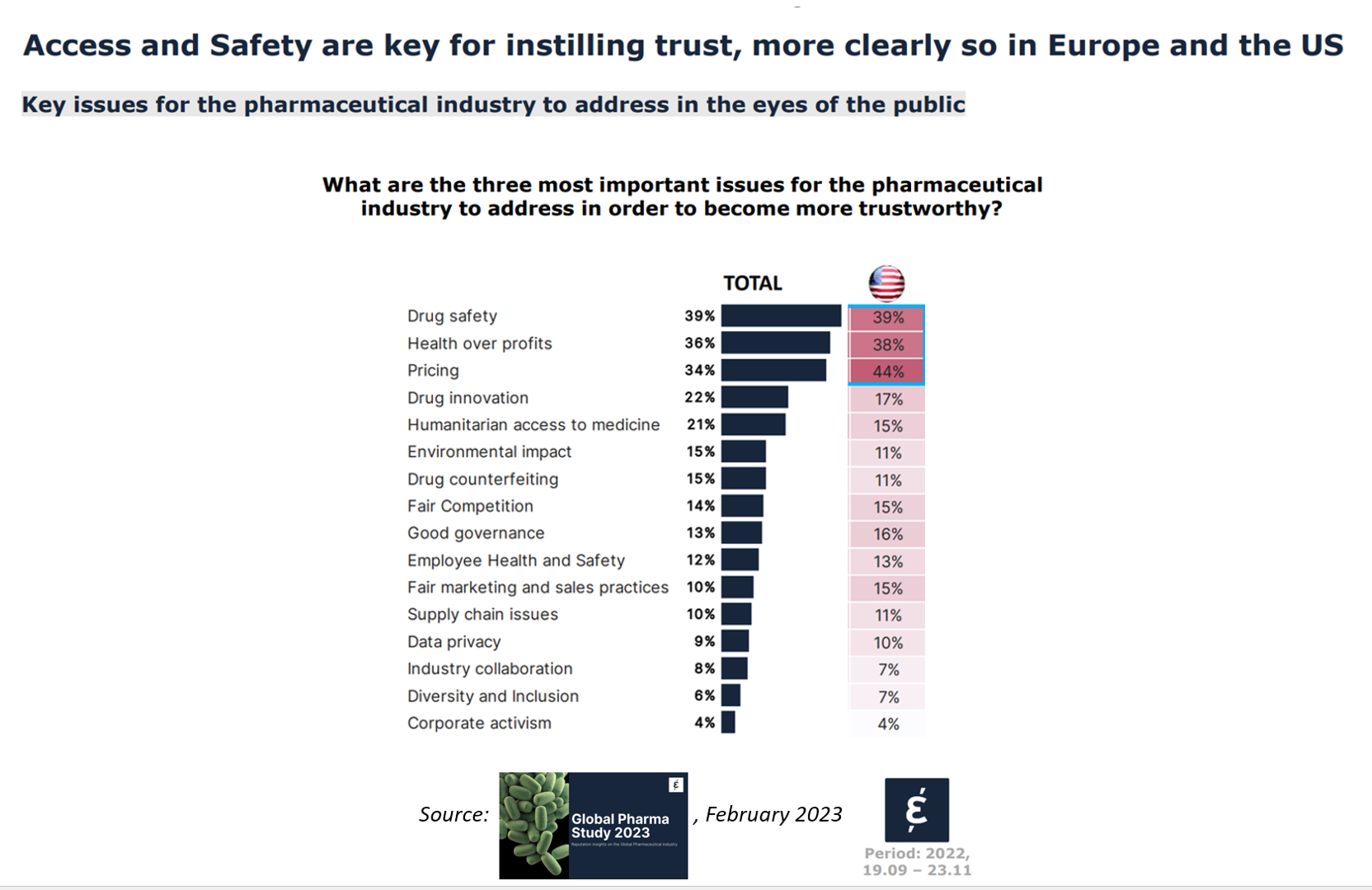
In the U.S., price and the cost of medicines is tied to how people feel about the pharma industry, evidenced in the Global Pharma Study 2023 from Caliber. Caliber, a reputation and corporate strategy consultancy, fielded survey research among over 17,000 health consumers including U.S. adults between 18 and 75 years of age as well as health citizens living in Brazil, China, France, Germany, Japan, and the UK. Caliber assessed the reputation of 16 industries, globally, finding that pharma ranked 10th among the 16, just below automotive and just above chemicals (and well
The US Healthcare System Outspends and Underperforms While Most People Live Paycheck to Paycheck
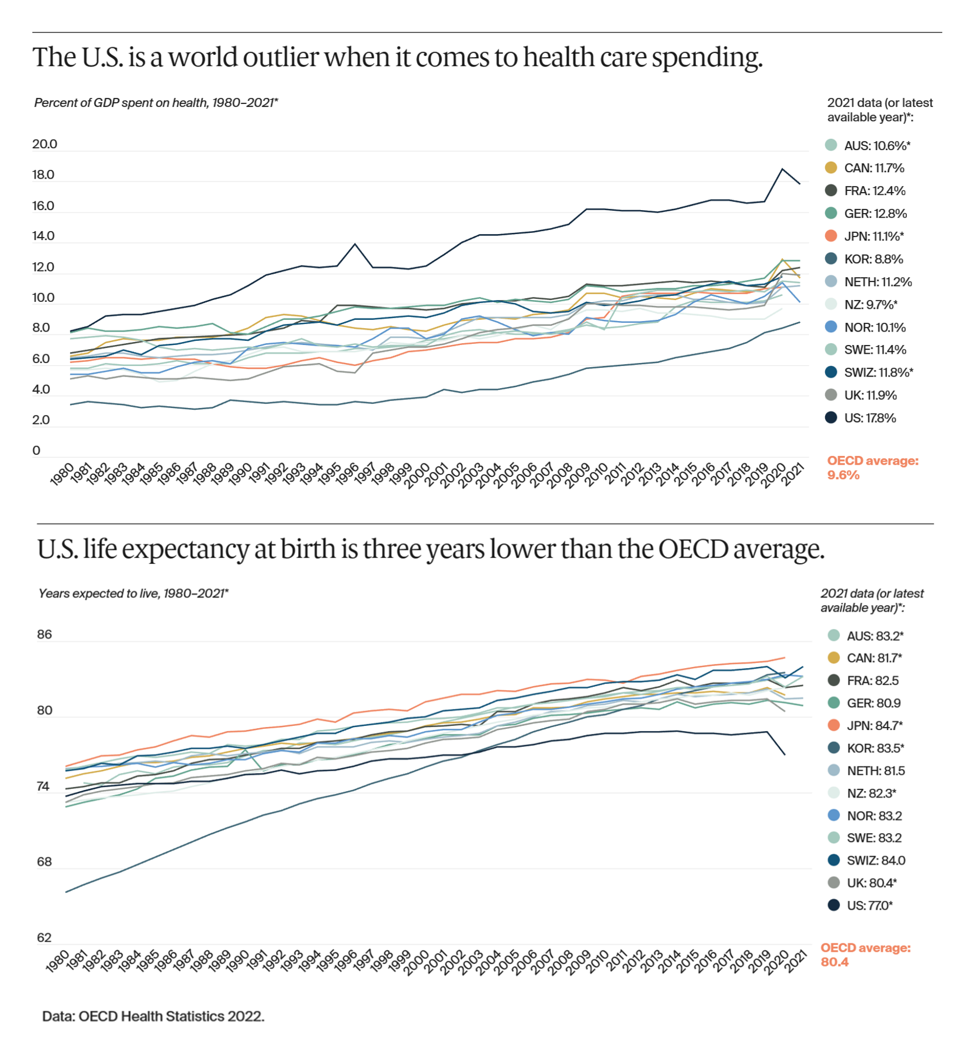
The U.S. is an outlier in the world for high health care spending, as well as in low achievement for life expectancy at birth — 3 years less than that in peer OECD countries — discussed in U.S. Health Care from a Global Perspective, 2022: Accelerating Spending, Worsening Outcomes, the latest look into American health system performance in a global context from The Commonwealth Fund. Another study published in JAMA this week talks about the Organization and Performance of US Health Systems, calling out the fact that, “Small quality differentials combined with large price differentials suggests that health systems have
What Are Patients Looking for in a Doctor? It Depends on Who You Ask…and Their Race
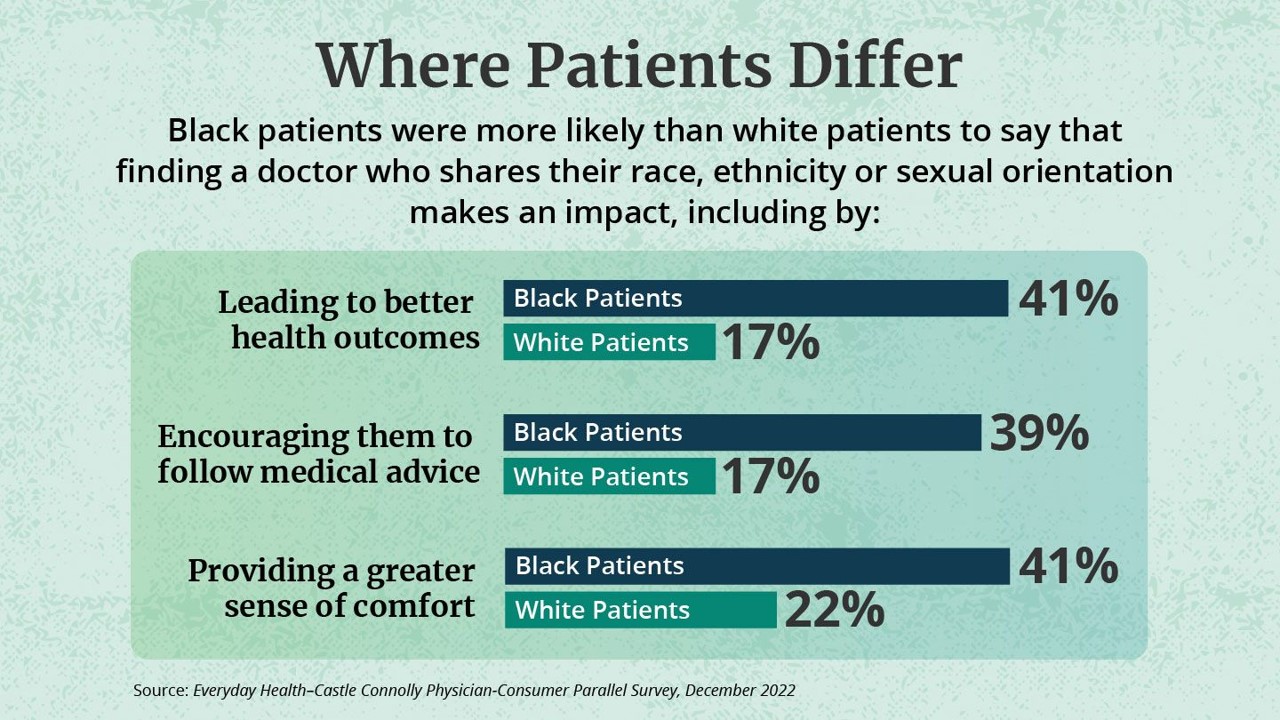
While the same proportion of Black and White patients say they are looking for a doctor with empathy and compassion, there are relatively large differences between patients based on their race, found in the Everyday Health-Castle Connolly Physician-Consumer study. The survey was conducted in December 2022 among a group of 1,001 U.S. consumers and 277 Castle Connolly health care professionals. As the first bar chart illustrates “where patients differ, “Black people were nearly twice as likely as white people (41 percent versus 22 percent) to completely agree that they would be more comfortable and
Quick, Accessible, Inexpensive Health Care – A Retail Health Update from Amazon and Dollar General

Two announcements this week add important initiatives to patients’ growing choices that speak to their consumer-sides’ sense of value and personal healthcare cost-containment: Amazon launched RxPass, a generic medicines subscription service; and, Dollar General promoted its mobile health service powered by DocGo on demand for health visits, “right outside the store.” These two programs come from outside of the legacy health care system of so-called incumbents — hospitals, health systems, health insurance — leveraging two brand-names beloved to many consumers for convenience, price transparency, and sheer cost. First, check out Amazon Pharmacy’s RxPass. Amazon
Record Numbers of People in the U.S. Putting Off Medical Care Due to Cost – A New “Pink Tax” on Women?
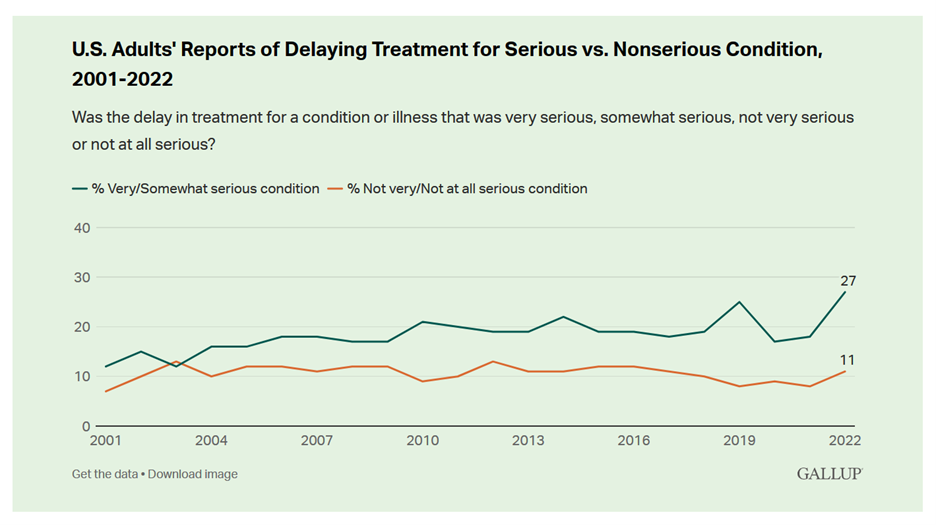
More people in the U.S. than ever have put off medical care due to cost, according to Gallup’s latest poll of patients in America. Gallup conducted the annual Health and Healthcare poll U.S. adults in November and December 2022. This was the highest level of self-rationing care due to cost the pollster has found since its inaugural study on the topic in 2001. This was also the most dramatic year-on-year increase of postponing treatment due to cost in the study’s history. Note the substantial difference in women avoiding
Digital Health Funding Updates from FINN + Galen and Silicon Valley Bank – Context for JPM2023
As we enter the week’s brainstorms and deal-making prospects this week at the annual JP Morgan meet-up for healthcare, I’m kicking off Health Populi’s posts this week by diving into two major reports published in sync with this meeting that’s so pivotal and important for the digital health community: the Silicon Valley Bank (SVB) 2022 Annual Report on Healthcare Investments and Exits and the 2022 Global State of Digital Health Report from FINN Partners and Galen Growth SVB notes that venture funding in healthcare fell in terms of both deals and dollars each quarter
In 2023, We Are All Health Consumers in Search of Value
Every health/care industry stakeholder will be in search of value in 2023, I explain in my latest post written on behalf of Medecision. In this essay, I forecast what’s ahead for hospitals, digital health innovators and investors, employers, pharma, and patients-as-consumers — all firmly focused on value in the new year. “Inflation may make consumers and the healthcare system sicker,” Deloitte expects, signaling a sort of “unrest” for the healthcare ecosystem. One of the most telling data points I include in my assessment of 2023 comes from GSR Ventures, which polled major health care investors on
When Household Economics Blur with Health, Technology and Trust – Health Populi’s 2023 TrendCast

People are sick of being sick, the New York Times tells us. “Which virus is it?” the title of the article updating the winter 2022-23 sick-season asked. Entering 2023, U.S. health citizens face physical, financial, and mental health challenges of a syndemic, inflation, and stress – all of which will shape peoples’ demand side for health care and digital technology, and a supply side of providers challenged by tech-enabled organizations with design and data chops. Start with pandemic ennui The universal state of well-being among us mere humans is pandemic ennui: call it languishing (as opposed to flourishing), burnout, or
Dollar General & CHPA Collaborate to Bolster Health Consumers’ Literacy and Access for OTC Pain Meds and Self-Care
Health is “made” where we live, work, play, pray, learn….and shop. I spend a lot of time these days in the growing health/care ecosystem where retail health is broadening to address social determinants and drivers of health – namely food, transportation, broadband access, education, environment, and financial wellness – all opportunities for self-care and health engagement. For many years, I have followed the activities of CHPA, the Consumer Healthcare Products Association, and have participated in some of their conferences. Their recent announcement of a collaboration with Dollar General speaks to the growing role of self-care for all people.
Consumers Are Feeling Their Healthcare Cost of Living – Research from Qualtrics
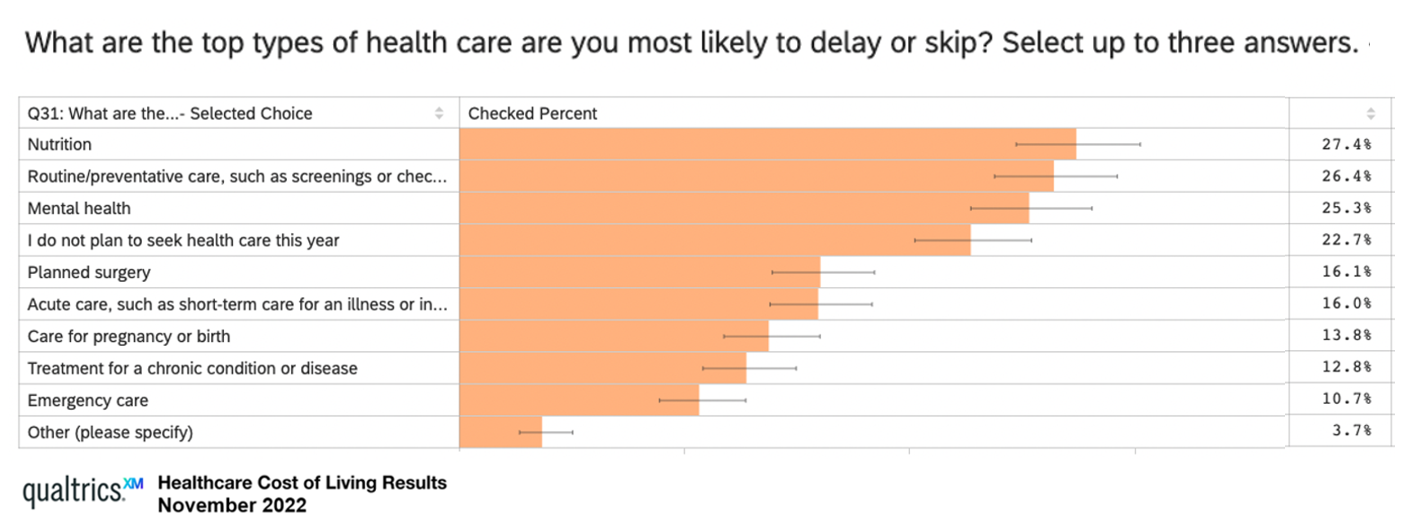
Rising costs are the #1 reason U.S. health consumers are avoiding or delaying health care, replacing concerns about COVID-19, based on survey research from Qualtrics. The company’s Healthcare Cost of Living survey research learned that 48% of U.S. adults chose to defer health care in 2022, split by 31% of consumers skipping care due to cost concerns, and, 17% of people delaying care who had concerns about the coronavirus. Note the types of care delayed or skipped: Over 27% of people delayed care related to nutrition 26% delayed routine or preventive care, such as screenings or
Dr. Santa Intends to Deliver Consumer Health-Tech for the 2022 Holidays
Even as consumers’ confess a tighter spending economy for 2022 holiday shopping, peoples’ intent to buy wearable tech for health and fitness and other wellness devices appear on gifting lists in the U.S., according to the 29th Annual Consumer Technology Holiday Purchase Patterns report from the Consumer Technology Association (CTA). In general, technology will be a top-selling category for 2022 holiday gift-giving, somewhat tempered by inflation and the increased cost of living that challenge household budgets in the fourth quarter of 2022. Tech spending will be down about 6% in 2022 according to CTA’s
In Search of Clinical Effectiveness, But “Investment Exuberance?” Not So Much. Insights From FINN Partners and Galen Growth at HLTH 2022

While venture funding for digital health technology declined globally by 35% in the first three quarters of 2022 compared with 2021, this marks a “return to normal” based on the assessment in the Global State of Digital Health Report from FINN Partners and Galen Growth, published today and launched during the HLTH 2022 conference. The report analyzes data from over 12,000 digital health ventures tracked by Galen Growth’s HealthTech Alpha platform. The first chart illustrates the change in venture funding by therapeutic area, showing downturns in four of the five areas called
Thinking Value-Based Health Care at HLTH 2022 – A Call-to-Action
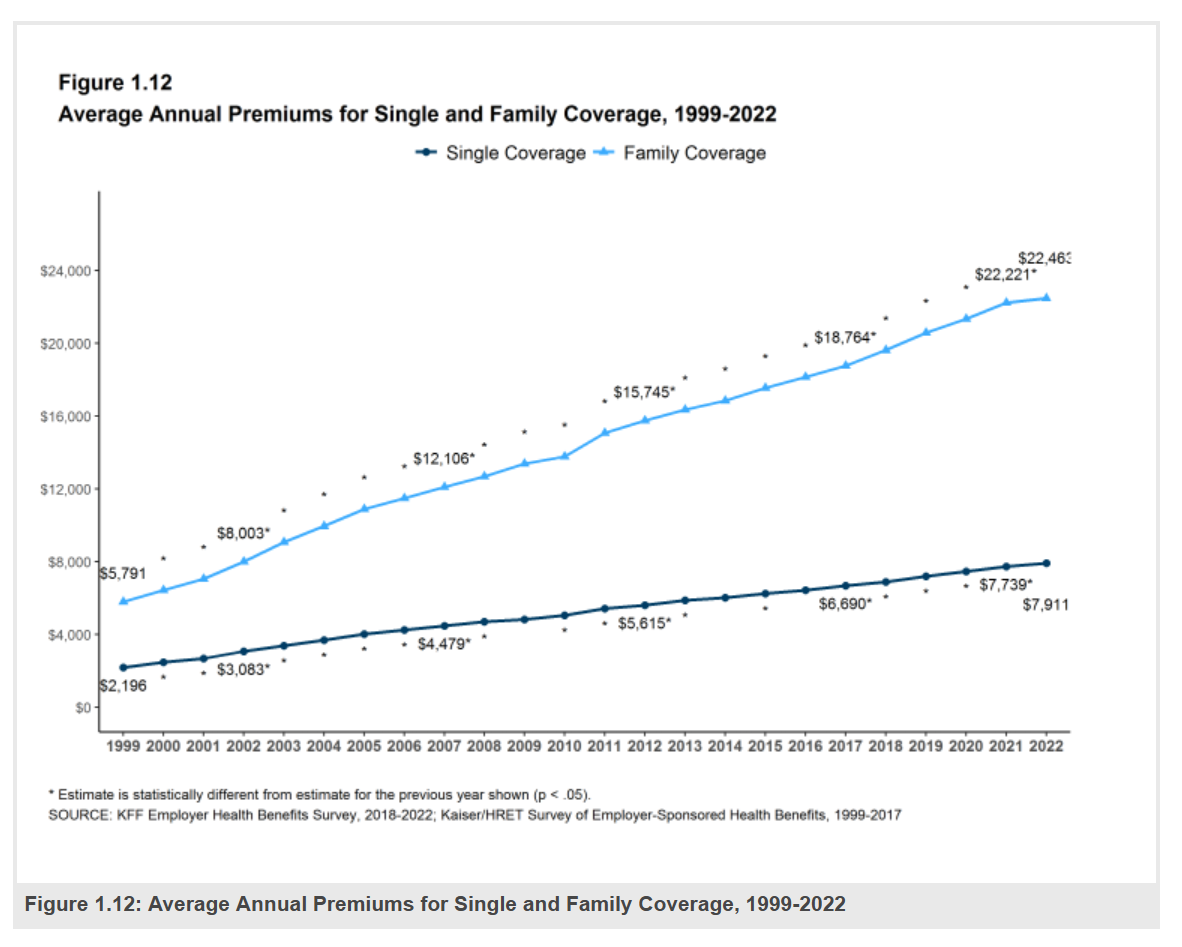
The cost of health insurance for a worker who buys into a health plan at work in 2022 reached $22,463 for their family. The average monthly mortgage payment was $1,759 in mid-2022. “When housing and health both rank as basic needs in Maslow’s hierarchy, what’s a health system to do?” I ask in an essay published today on Crossover Health’s website titled Value-Based Care: Driving a Social Contract of Trust and Health. The answer: embrace value-based care. Warren Buffett wrote Berkshire Hathaway shareholders in 2008, asserting that, “Price is what you pay. Value
$22,463 Can Get You a Year of College in Connecticut, a Round of Ref Work in the Stanley Cup Playoffs, or Health Benefits for a Worker’s Family
Employers covering health insurance for workers’ families will face insurance premiums reaching, on average, $22,463. That is roughly what a year at an independent college in Connecticut would cost, or a round of pay for a ref in the Stanley Cup playoffs. With that sticker-shock level of health plan costs, welcome to the 2022 Employer Health Benefits Survey from Kaiser Family Foundation, KFF’s annual study of employer-sponsored health care. Each year, KFF assembles data we use all year long for strategic and tactical planning in U.S. health care. This mega-study looks at
How Will the “New” Health Economy Fare in a Macro-Economic Downturn?

What happens to a health care ecosystem when the volume of patients and revenues they generate decline? Add to that scenario a growing consensus for a likely recession in 2023. How would that further impact the micro-economy of health care? A report from Trilliant on the 2022 Trends Shaping the Health Economy helps to inform our response to that question. Start with Sanjula Jain’s bottom-line: that every health care stakeholder will be impacted by reduced yield. That’s the fewer patients, less revenue prediction, based on Trilliant’s 13 trends re-shaping the U.S. health
Health Care Costs Are a Driver of Health Across All of America – Especially for Women
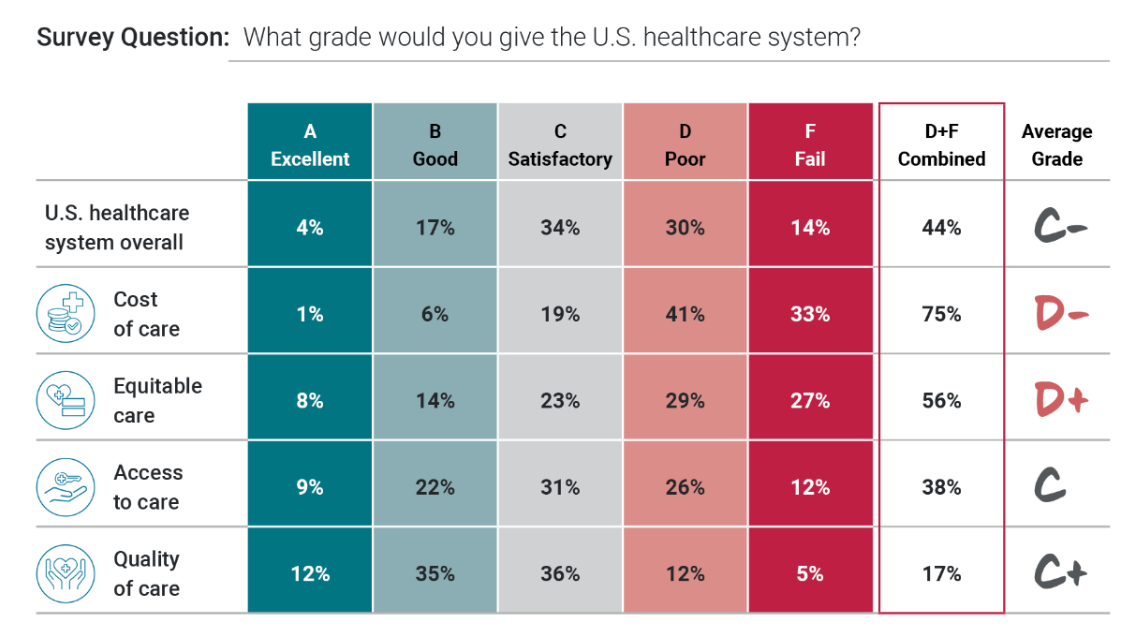
Three in four people in America grade health care costs a #fail, at grade “D” or lower. This is true across all income categories, from those earning under $24,000 a year to the well-off raking in $180K or more, we learn in Gallup’s poll conducted with West Health, finding that Majorities of people rank cost and equity of U.S. healthcare negatively. Entering the fourth quarter of 2022, several studies were published in the past week which reinforce the reality that Americans are facing high health care costs, preventing many from seeking necessary medical services, and hitting under-served health citizens even harder
Connected Wellness Growing As Consumers Face Tighter Home Economics
“Consumers are using the Internet to take their health into their own hands,” at least for 1 in 2 U.S. consumers engaging in some sort of preventive health care activity online in mid-2022. The new report on Connected Wellness from PYMNTS and Care Credit profiles American health consumers’ use of digital tools for health care promotion and disease prevention. The bottom-line here is that the most connected 10% of consumers were 1.65 times more likely to be engaged in preventive digital health activities than the average person. Peoples’ engagement with digital health
The Patient As the Payer: Self-Pay, Bad Debt, and the Erosion of Hospital Finances
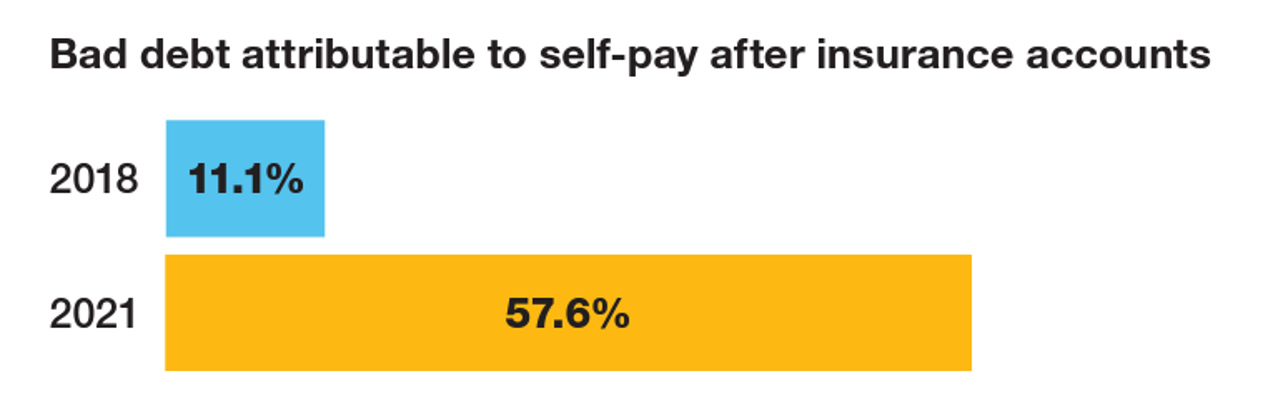
“The odds are against hospitals collecting patient balances greater than $7,500,” the report analyzing Hospital collection rates for self-pay patient accounts from Crowe concludes. Crowe benchmarked data from 1,600 hospitals and over 100,00 physicians in the U.S. to reveal trends on health care providers’ ability to collect patient service revenue. And bad debt — write-offs that come out of uncollected patient bill balances after “significant collection efforts” by hospitals and doctors — is challenging their already-thin or negative financial margins. The first chart quantifies that bad debt attributable to patients’ self-pay payments
The More Chronic Conditions, the More Likely a Patient Will Have Medical Debt
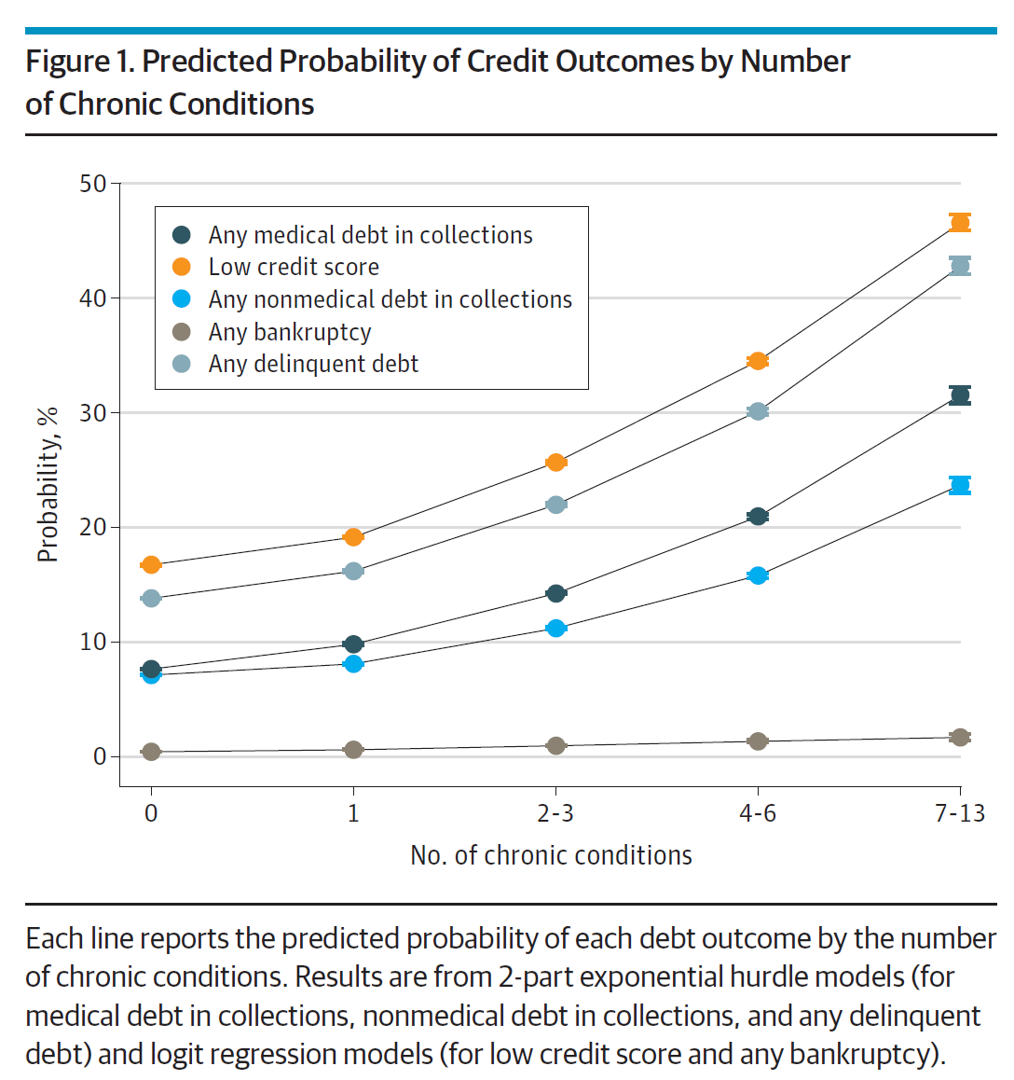
There is a direct association between a person’s health status and patient outcomes and their financial health, quantified in original research published this week in JAMA Internal Medicine. Researchers from the University of Michigan (my alma mater) Medical School and Institute for Healthcare Policy and Innovation analyzed two years of commercial insurance claims data generated between January 2019 and January 2021, linking to commercial credit data from January 2021 for patients enrolled in a preferred providers organization in Michigan. The first chart illustrates the predicted probability of credit outcomes based on the
Americans Rationing Healthcare in the Inflationary Era; Out-of-Pocket Expenses Are the Concern
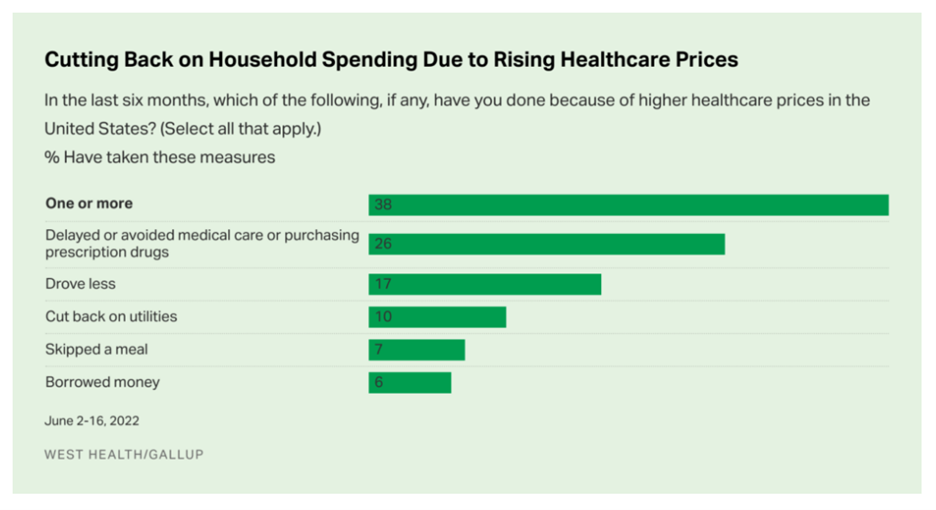
Nearly 100 million people in the U.S. cut back on healthcare due to costs in the first half of 2022, according to the latest poll on health care costs form Gallup and West Health, gauging Americans’ financial health in June 2022. That’s the month when inflation in the U.S. reached 9.1%, a 40-year high. Among Americans’ cuts to household spending was the most common medical self-rationing behavior, delaying or avoiding care or purchasing prescription drugs, the survey found. Nearly 4 in 5 people in the U.S. had delayed care or prescription meds between January
Gas ‘N Healthcare – How Transportation Links to Health Care Access and Financial Health
Some patients dealing with cancer at Mercy Health’s Lourdes Hospital have been supplied with gas cards. This gesture is enabling families to get to medical appointments around Paducah, Kentucky where, this week, car drivers faced regular gas priced at an average of $4.16 a gallon compared with $2.92 one year ago. Here’s the Hospital’s Facebook page featuring their gratitude to FiveStar Food Mart, the American Cancer Society, and the Mercy Health Foundation. “By providing cancer patients with gas cards, the cancer care team at Mercy Health Lourdes Hospital in Paducah hopes to mitigate financial challenges
More Americans Trust Small Biz and the Military than the Medical System, Gallup Finds
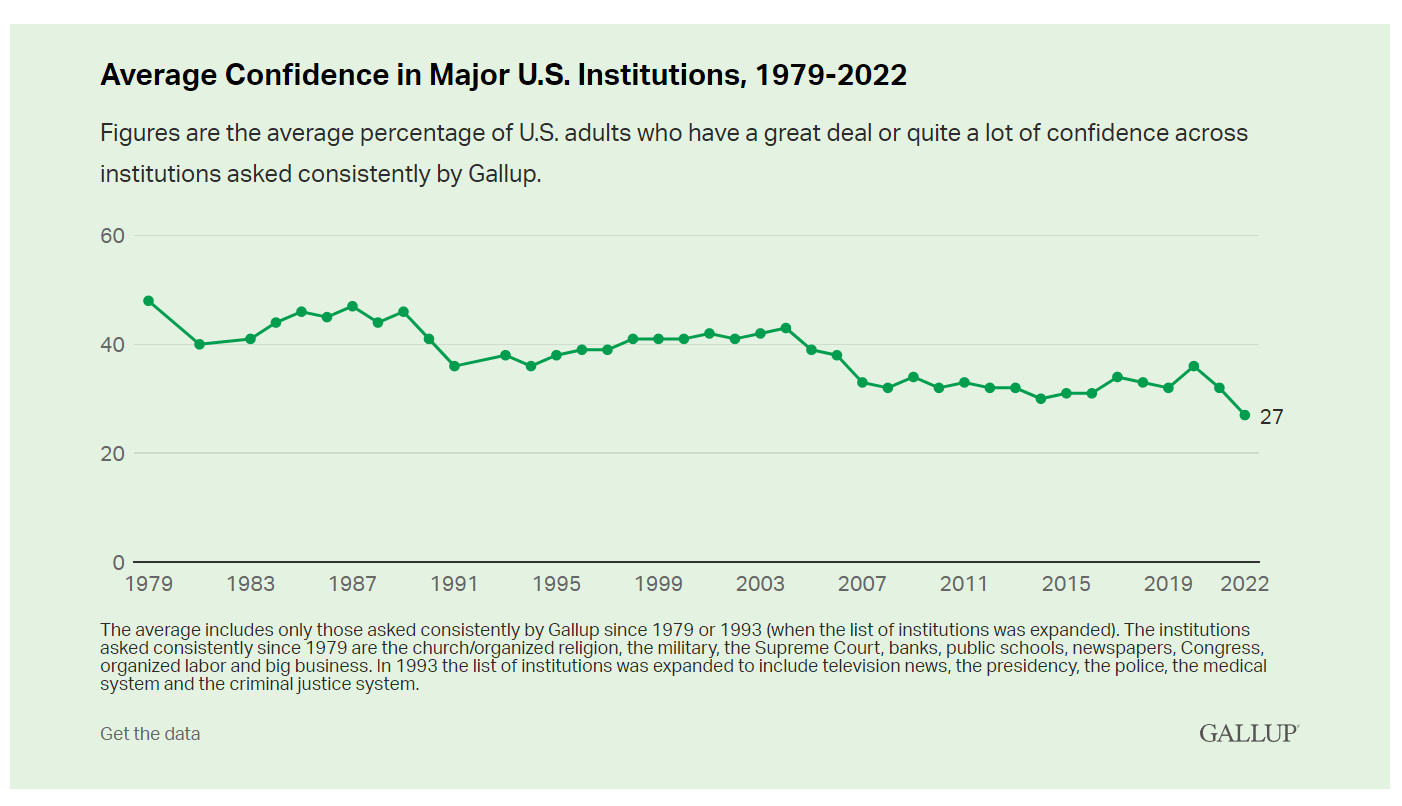
The most trusted institutions in the U.S. are small business and the military, the only two sectors in which a majority of Americans have confidence. Americans’ trust in institutions hit new historic lows in 2022, Gallup found in its latest poll of U.S. sentiment across all major sectors. Today, more Americans have faith in the police than in the medical system, according to a Gallup poll finding that Confidence in U.S. Institutions Down; Average at New Low. published this week of Independence Day 2022. Confidence runs from a higher of 68% for
The Unbearable Heaviness of Inflation: Will Consumers’ Financial Stress Erode Their Health?
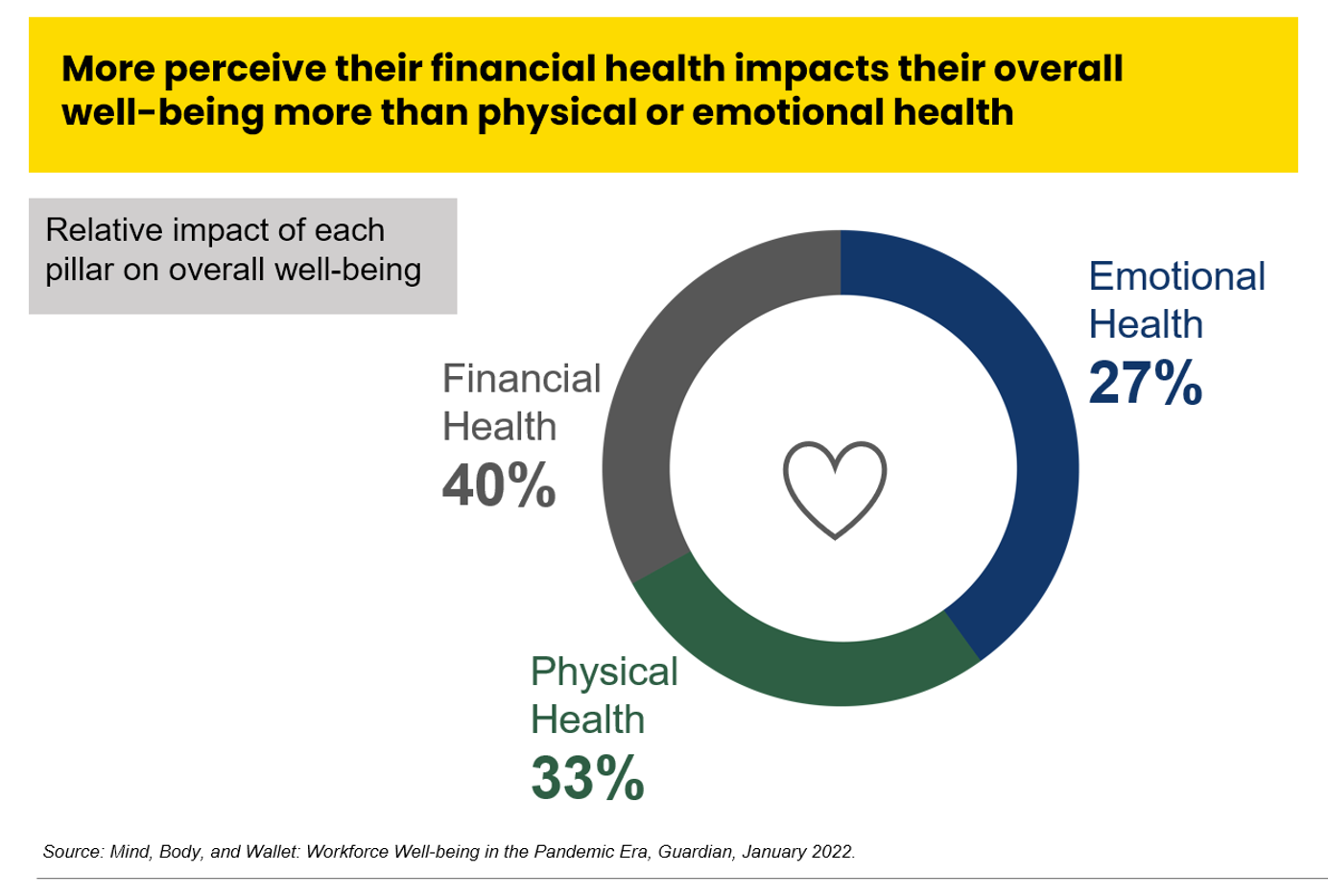
“Inflation is the big story,” the economics team at Morning Consult told us yesterday in a call on “How to Think Like An Economist.” While I already thought I did that, Team @MorningConsult updated us on the current state of consumers and what’s weighing most heavily on their minds…inflation being #1. An hour after the Morning Consult session, I brainstormed the topic of consumers-as-payers of medical bills and prescription drugs with GoodRx strategy leaders. In my data wonkiness, inflation certainly played a starring role in setting the stage for Mind, Body and Wallet — the title of one of the sources
Only in America: Medical Debt Is Most Peoples’ Problem, KHN and NPR Report
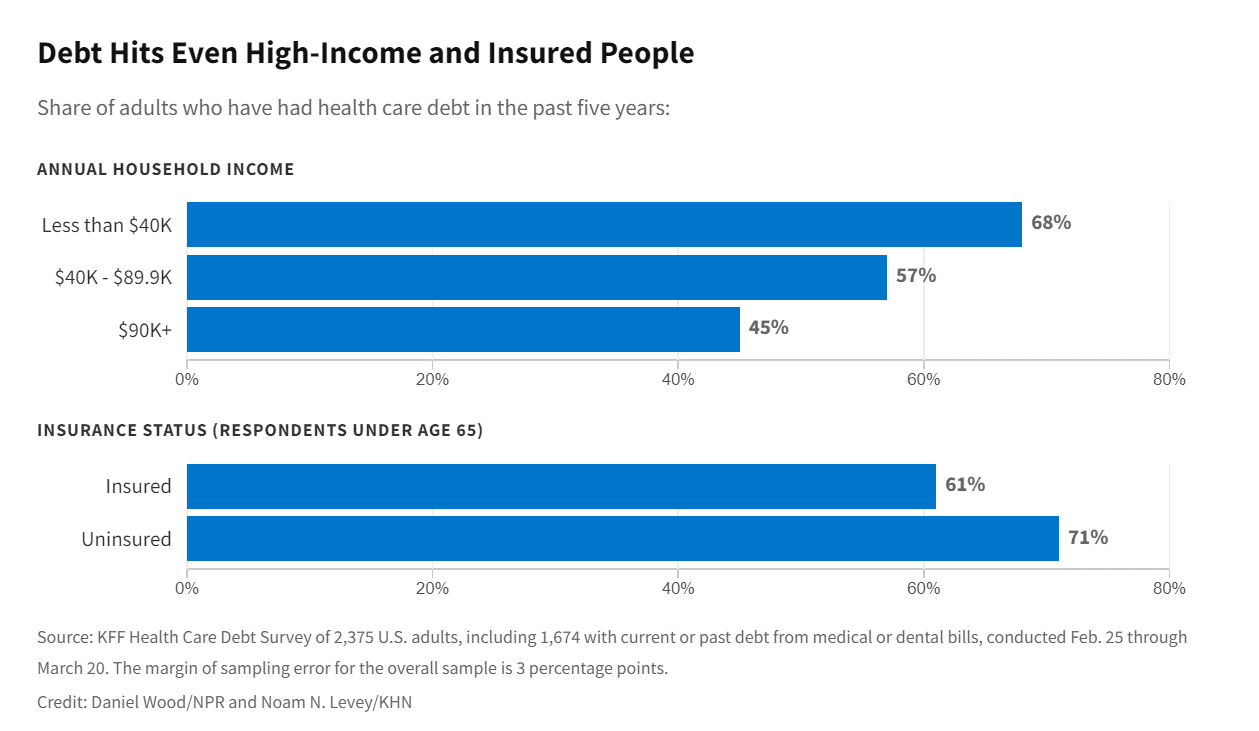
When high-deductible health plans became part of health insurance design in America, they were lauded as giving patients “more skin in the game” of health care payments. The theory behind consumer-directed care was that patients-as-consumers would shop around for care, morph into rational consumers of medical services just as they would do purchasing autos or washing machines, and shift the cost-curve of American health care ever downward. That skin-in-the-game has been a risk factor for .some patients to postpone care as well as take on medical debt — the strongest predictor of which is dealing with multiple chronic conditions. “The
Consumers Intend to Invest in Technology — With Budget and Value in Mind
Consumers continued to invest in and use several technologies that supported self-care at home in 2021, with plans to purchase connected health devices, sports and fitness equipment in the next year. But these purchases will be made with greater attention to budget and value consumer mindsets firmly focused on (and stressed by) inflation. The 24th Annual Technology Ownership & Market Potential Study from the Consumer Technology Association (CTA) tells us that Americans in 2022 will have to manage challenging economic headwinds, shopping for technology is preparing people for their new normal —
The Care Crisis – Robots Won’t Save Us
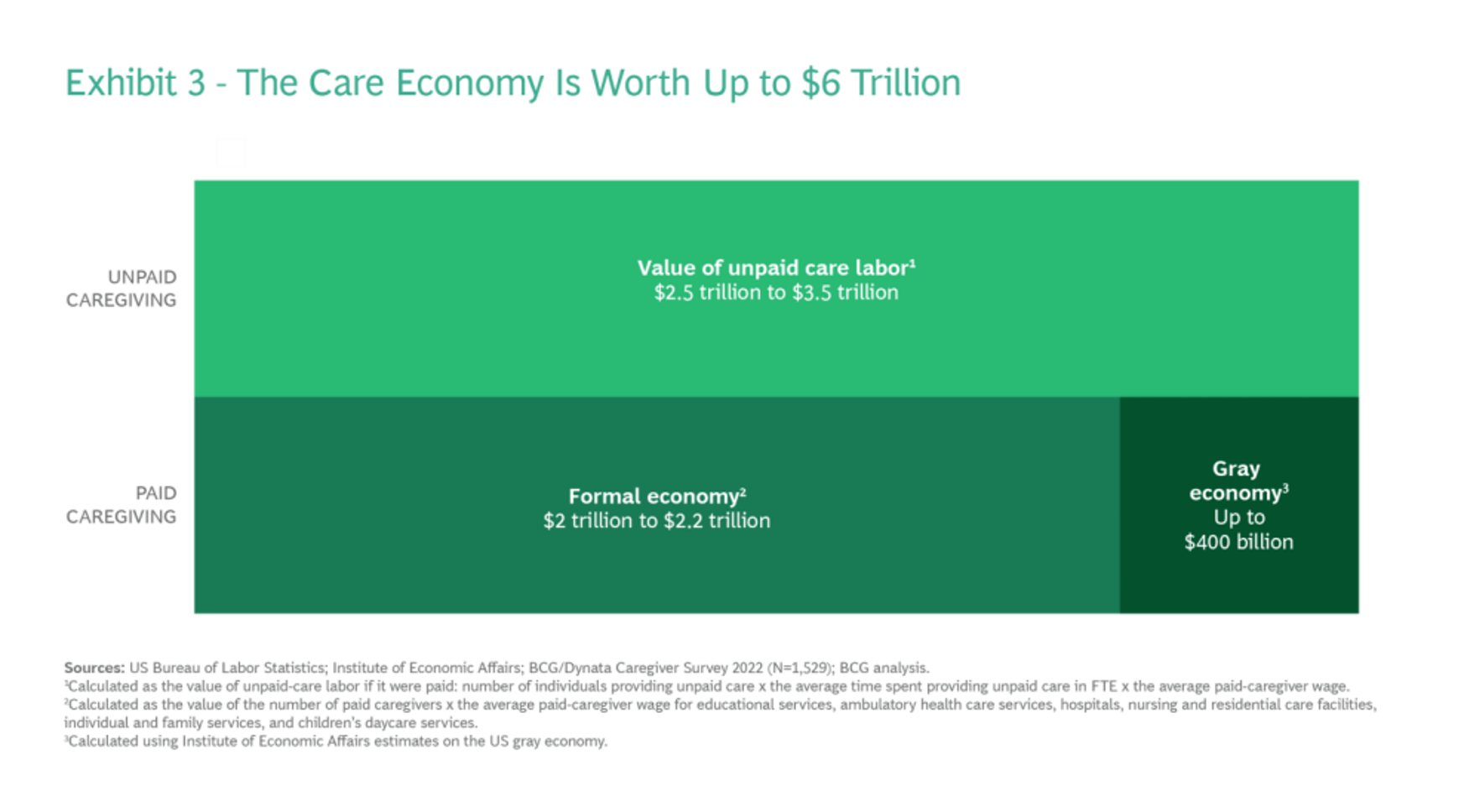
Among the many lessons we should and must take emerging out of the COVID-19 pandemic, understanding and addressing the caregiver shortage-cum-crisis will be crucial to building back a stronger national economy and financially viable households across the U.S. And if you thought robots, AI and the platforming of health care would solve the shortage of caregivers, forget it. Get smarter on the caregiver crisis by reading a new report, To Fix the Labor Shortage, Solve the Care Crisis, from BCG. You’ll learn that 9 of 10 new care-sector jobs will be in-person for
What If Costco Designed the Prescription Drugs Sales Model?
The good news about prescription drugs, in the context of medical spending in the U.S., is that 9 in 10 medicines prescribed are generics. They comprise only 3% of all U.S. healthcare spending. But there’s bad news about prescription drugs in the context of medical spending in America. U.S. Consumers Overpay for Generic Drugs, a new paper from the Leonard Schaeffer Center for Health Policy & Economics asserts, with recommendations to address the intermediaries who benefit from the way Americans currently pay for medicines. Generics are “an American success story,” the authors call out, bringing
A New Chevy Equinox SUV, a Year in Grad School, or Health Care for Four – The 2022 Milliman Medical Index
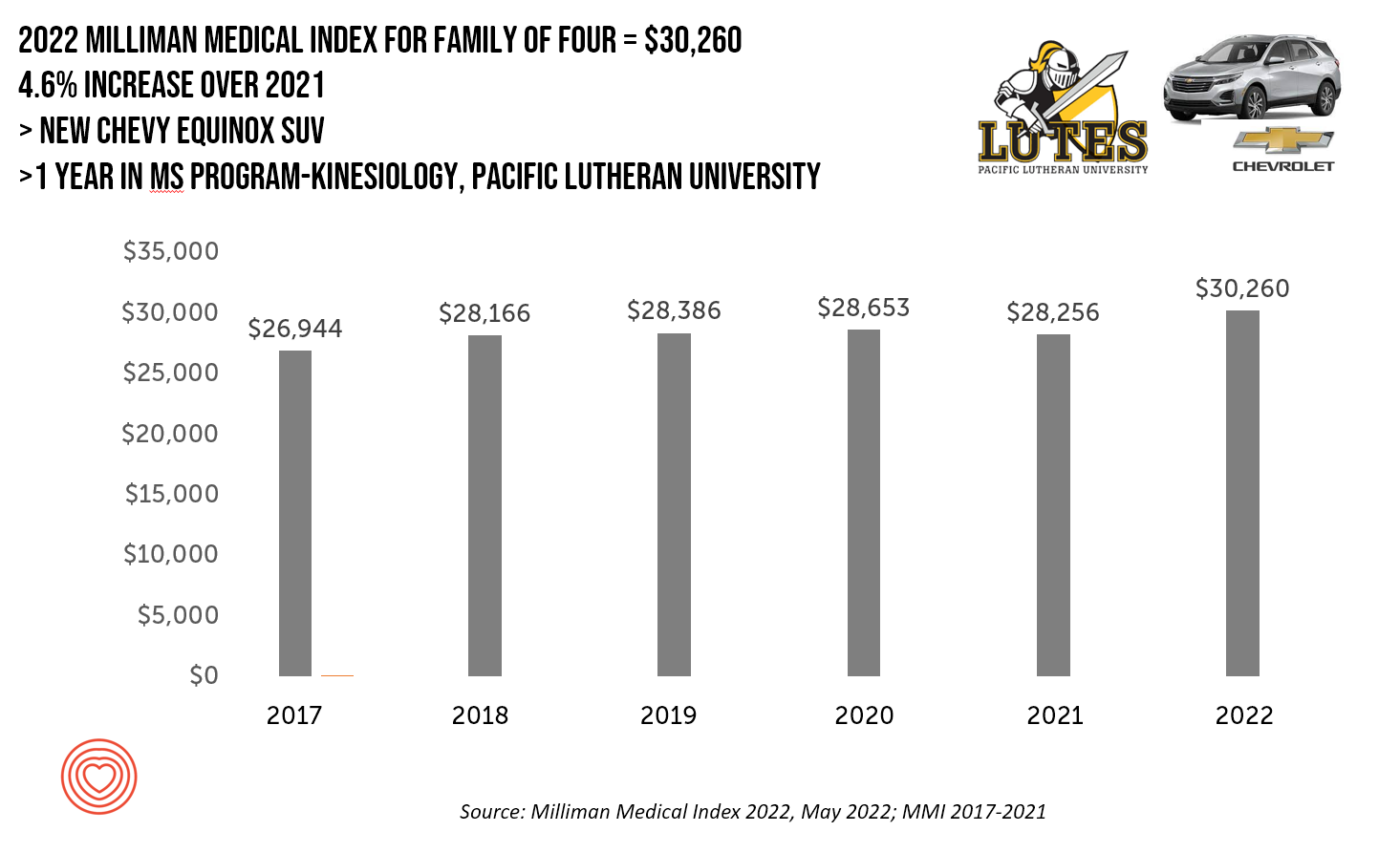
A new Chevy Equinox SUV, a year in an MS program in kinesiology at Pacific Lutheran U., or health care for a family of four. At $30,260, you could pick one of these three options. Welcome to this year’s 2022 Milliman Medical Index, which annually calculates the health care costs for a median family of 4 in the U.S. I perennially select two alternative purchases for you to consider aligning with the MMI medical index. I have often picked a new car at list price and a year’s tuition at a U.S. institution of
The Patient as Consumer and Payer – A Focus on Financial Stress and Wellbeing
Year 3 into the COVID-19 pandemic, health citizens are dealing with coronavirus variants in convergence with other challenges in daily life: price inflation, civil and social stress, anxiety and depression, global security concerns, and the safety of their families. Add on top of these significant stressors the need to deal with medical bills, which is another source of stress for millions of patients in America. I appreciated the opportunity to share my perspectives on “The Patient As the Payer: How the Pandemic, Inflation, and Anxiety are Reshaping Consumers” in a webinar hosted by CarePayment on 25 May 2022. In this
How Trust and Geopolitics Will Impact Health and Business – Edelman 2022 Trust Barometer at the World Economic Forum in Davos

When we think about the state of Trust in in mid-2022, there is some good news: Trust is rising (at least in democratic countries, while falling in autocratic ones). The bad news: the gap in Trust has dramatically widened between higher-income people compared with those earning lower-incomes, globally. And that gap is “tinder” that can be quickly sparked into a socio-political fire in countries around the world, Richard Edelman cautioned today when introducing the latest look at the 2022 Edelman Trust Barometer, focusing on geopolitics and business. We have never seen numbers like this
Stress Is Playing A Big Role in Consumers’ Food Habits: Food-As-Medicine Update from IFIC
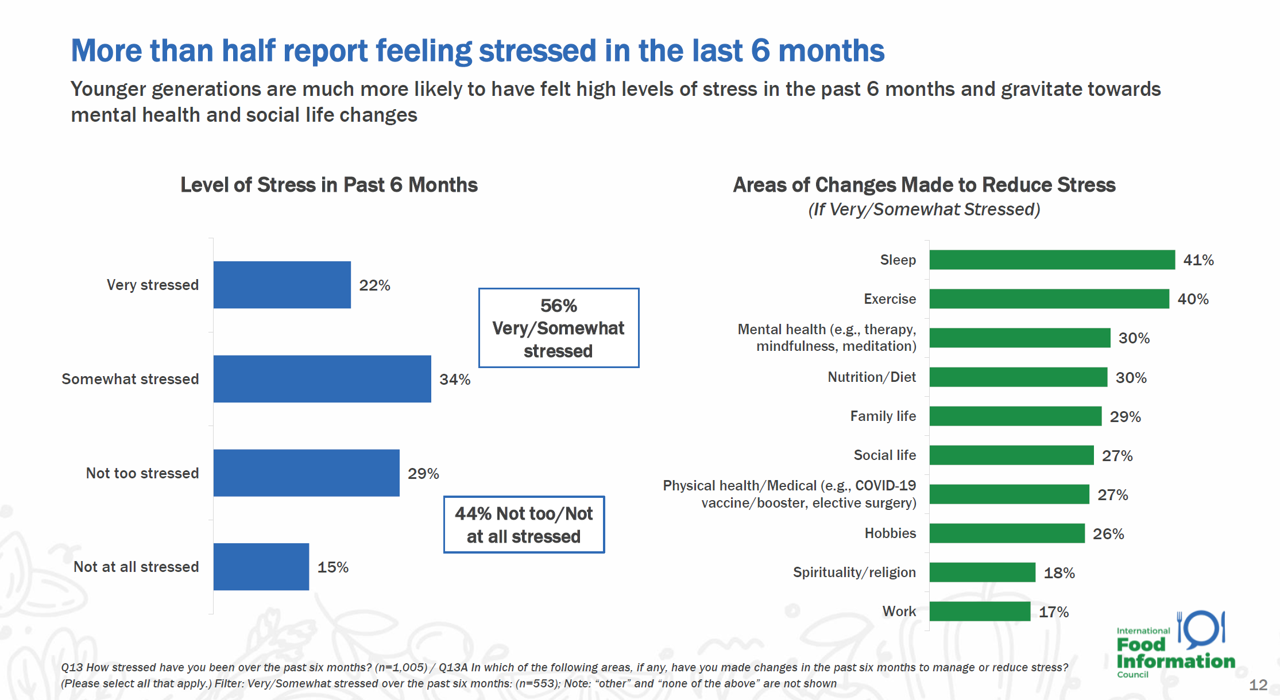
The COVID-19 pandemic accelerated consumers, globally, to take on more DIY roles as well as self-care for health and well-being. In addition, anxiety and stress are mainstream across demographics and have impacted the way people select and consume food, based on findings in the 2022 Food and Health Survey from the International Food Information Council (IFIC). In this 17th annual consumer survey, IFIC points to two underlying macro trends that are re-shaping peoples’ relationship with food and health: the pandemic’s impact, and “significant” generational shifts in taste, consumption, and values about nutrition and sustainability.
People Thinking More About the Value of Health Care, Beyond Cost
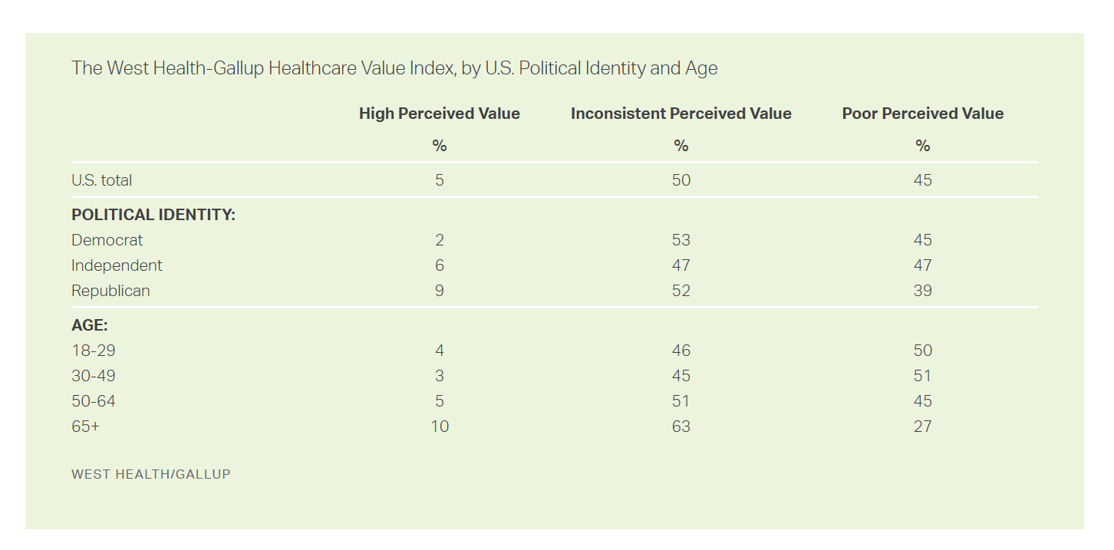
The rate of people in the U.S. skipping needed health care due to cost tripled in 2021. This prompted West Health (the Gary and Mary West nonprofit organizations’ group) and Gallup to collaborate on research to quantified Americans’ views on and challenges with personal medical costs. This has resulted in The West Health-Gallup Healthcare Affordability Index and Healthcare Value Index. The team’s research culminated in the top-line finding that some 112 million people in the U.S. struggle to pay for their care. That’s about 4.5 in 10 health citizens. Furthermore, 93% of people
Patients Look Beyond the Pandemic to Pharma for Engagement, Innovation, and Integrity
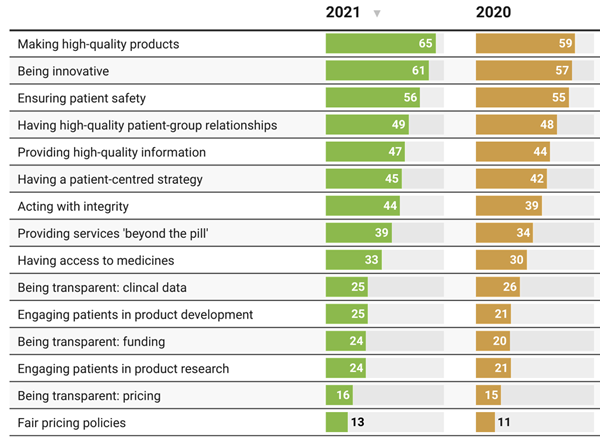
The COVID-19 pandemic has impacted patients who were already deeply engaged with their own health care before the coronavirus emerged. Compared with a year ago, more patients and their advocates are seeking quality therapies, innovation, engagement, and integrity from pharmaceutical companies, based on research published today from PatientView. PatientView, based in the UK, has collaborated with over 40,000 patient advocacy organizations globally marking over 10 years doing this research. The eleventh annual report on the Corporate Reputation of Pharma was conducted among 2,150 patient groups between November 2021 and February 2022, covering health citizens in Europe (with 1,229 organizations), North
How Business Can Bolster Determinants of Health: The Marmot Review for Industry

“Until now, focus on….the social determinants of health has been for government and civil society. The private sector has not been involved in the discussion or, worse, has been seen as part of the problem. It is time this changed,” asserts the report, The Business of Health Equity: The Marmot Review for Industry, sponsored by Legal & General in collaboration with University College London (UCL) Institute of Health Equity, led by Sir Michael Marmot. Sir Michael has been researching and writing about social determinants of health and health equity for decades, culminating publications
How the Pandemic, Inflation and Ukraine Are Re-Shaping Health Consumers – Learnings from dunnhumby
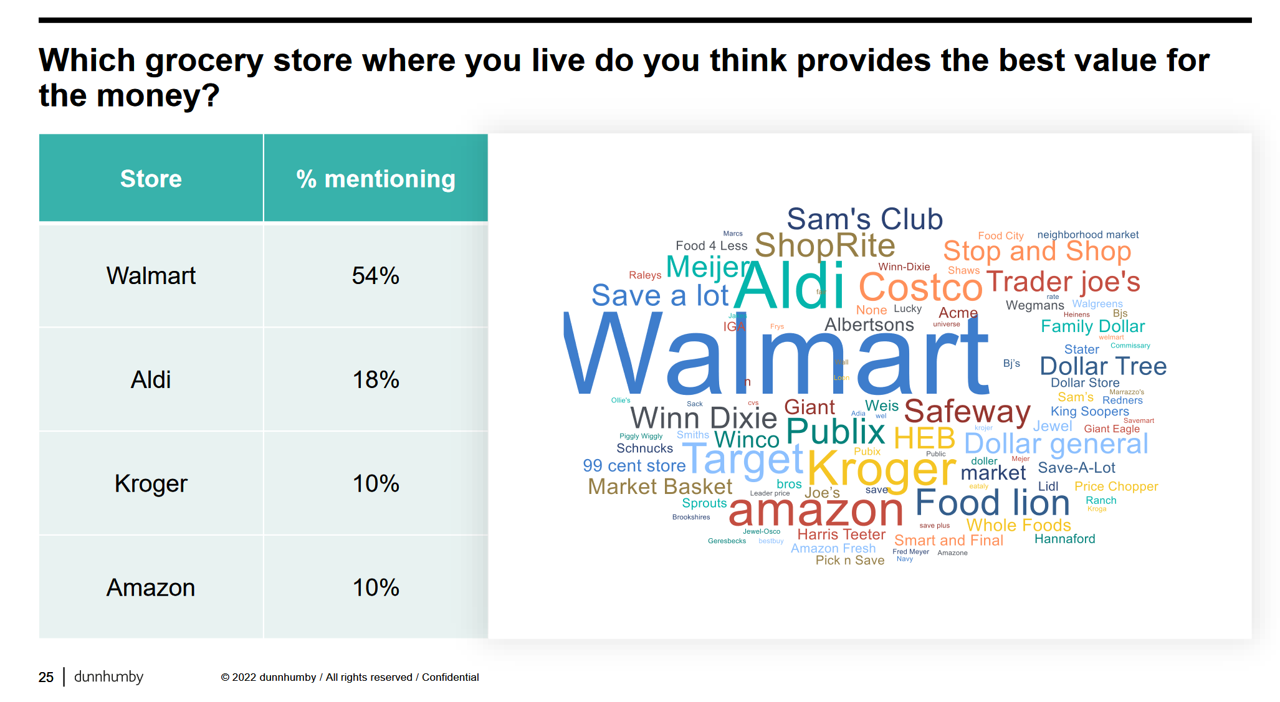
Too many dollars, stimulated by an influx of COVID-19 government stimulus, are chasing too few goods in economies around the world. Couple this will labor, material shortages, and disrupted supply chains, the exogenous shock of the Ukraine crisis amplifying cost increases and shortage driving higher prices for food and commodities, and global consumers are faced with strains in household budgets. This is impacting grocery stores and. through my lens, will impact health consumers’ spending, as well. In their discussion of Customer First Retailer Responses to Inflationary Times, dunnhumby, retail industry strategists, covered an update on inflation with the top-line that
In the New Inflationary Era, Gas and Health Care Costs Top Household Budget Concerns
Inflation and rising prices are the biggest problem facing America, most people told the Kaiser Family Foundation March 2022 Health Tracking Poll. Underpinning that household budget concern are gas and health care costs. Overall, 55% of people in the U.S. pointed to inflation as the top challenge the nation faces (ranging from 46% of Democrats to 70% of Republicans). Second most challenging problem facing the U.S. was Russia’s invasion into Ukraine, noted by 18% of people — from 14% of Republicans up to 23% of Democrats. The COVID-19 pandemic has fallen far down Americans’ concerns list tied third place with
McKinsey’s Six Shifts To Add Life to Years — and One More to Consider
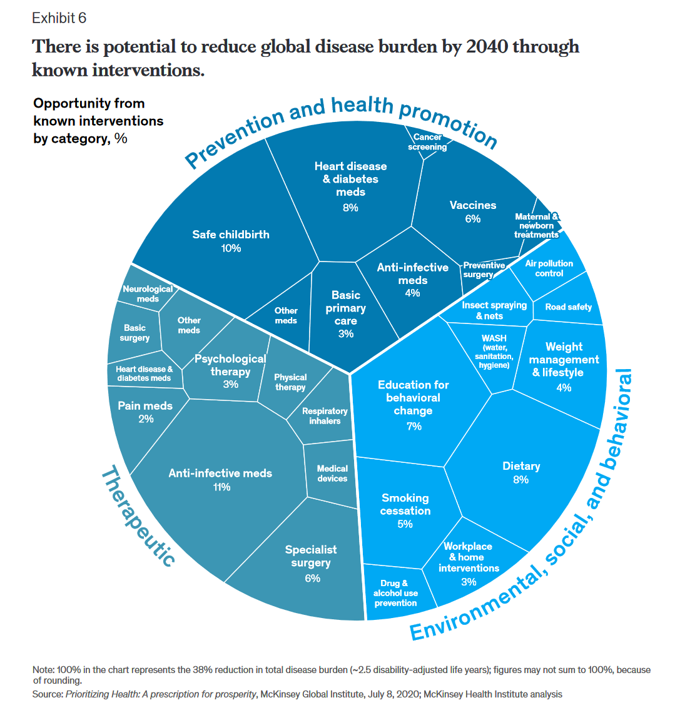
People spend one-half of their lives in “less-than-good health,” we learn early in the paper, Adding years to life and life to years from the McKinsey Health Institute. In this data-rich essay, the McKinsey team at MHI sets out an agenda that could help us add 45 billion extra years of higher-quality life equal to an average of six years per person (depending on your country and population demographics). The first graphic from the report illustrates four dimensions of health and the factors underneath each of them that can bolster or diminish our well-being: personal behaviors (such as sleep and diet),
The Financial Toxicity of Health Care Costs: From Cancer to FICO Scores
The financial toxicity of health care costs in the U.S. takes center stage in Health Populi this week as several events converge to highlight medical debt as a unique feature in American health care. “Medical debt is the most common collection tradeline reported on consumer credit records,” the Consumer Financial Protection Bureau called out in a report published March 1, 2022. CFPB published the report marking two years into the pandemic, discussing concerns about medical debt collections and reporting that grew during the COVID-19 crisis. Let’s connect the dots on: A joint announcement this week from three major credit agencies,
Food Insecurity, Energy Prices, and Medical Debt Spike in February 2022
There’s a trifecta cost challenge hitting U.S. household budgets in February 2022, highlighted in a poll from Morning Consult: inflationary spikes for housing, food, and energy, and the COVID-19 Omicron variant forcing health care costs up for some consumers driving medical debt up. This further underscores the reality that medical spending in the U.S. is taking shape as a consumer service or good, competing with — potentially crowding out — other household line items like food and increasingly costly petrol to fill gas tanks. Or taken the other way, gas and food crowding out health care spending, leading to either
The Wellness Economy in 2022 Finds Health Consumers Moving from Feel-Good Luxury to Personal Survival Tactics
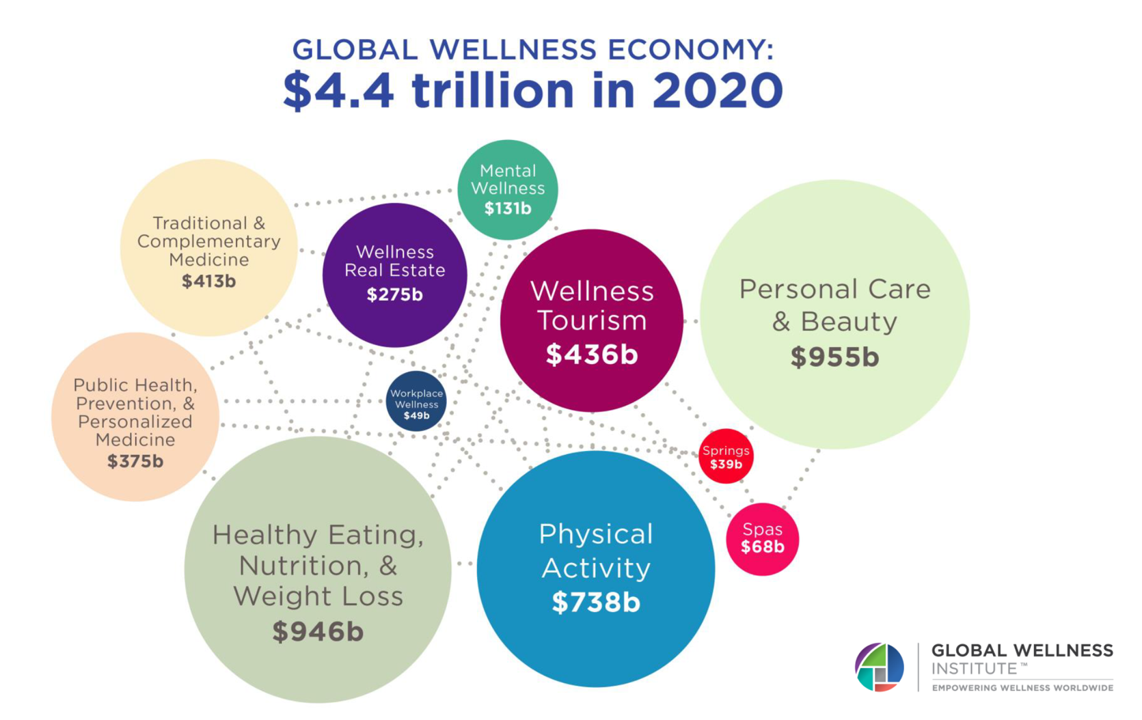
The Future of Wellness in 2022 is, “shifting from a ‘feel-good’ luxury to survivalism as people seek resilience,” based on the Global Wellness Institute’s forecast on this year’s look into self-care and consumer’s spending on health beyond medical care — looking beyond COVID-19. GWI published two research papers this week on The Future of Wellness and The Global Wellness Economy‘s country rankings as of February 2021. I welcomed the opportunity to spend time for a deep dive into the trends and findings with the GWI community yesterday exploring all of the data, listening through my health economics-consumer-technology lens. First, consider
Will “Buy Now, Pay Later” Financing Help Health Consumers Pay Their Medical Bills?
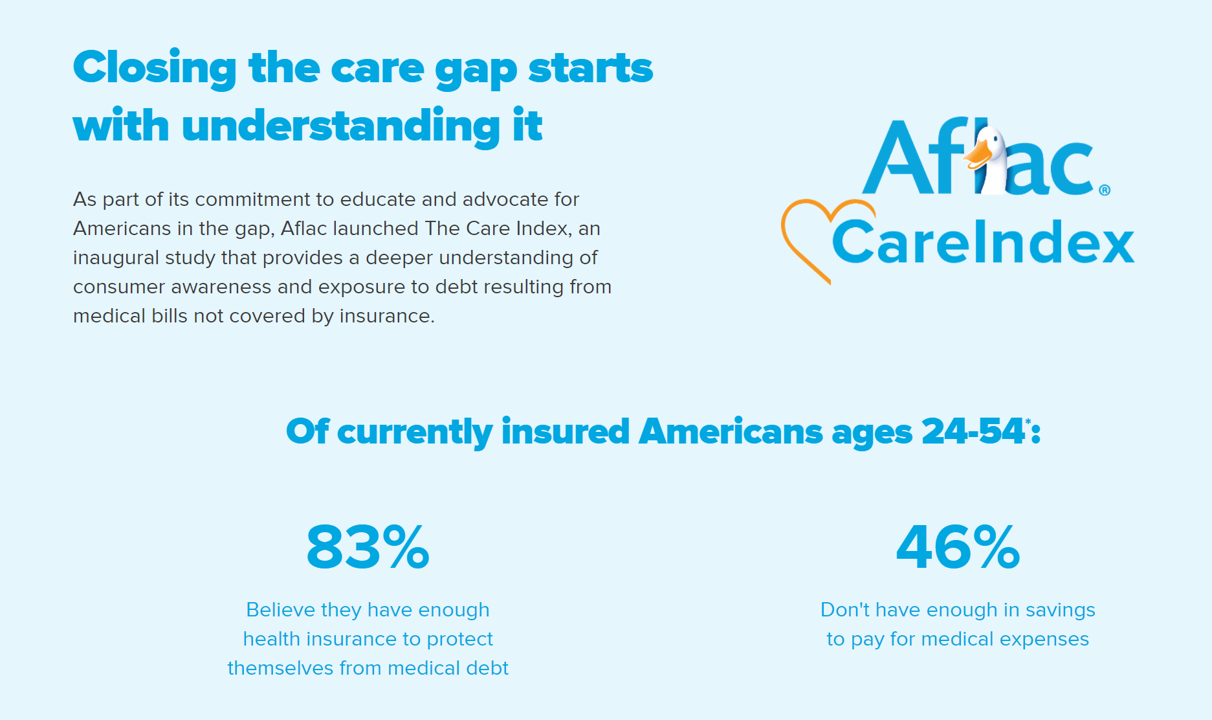
Aflac, our favorite duck-mascot-representing company, has launched the Close the Gap initiative featuring spokesman Deion Sanders, one of the good guys in the Football Hall of Fame. Recognizing the fact that nearly one-half of insured Americans don’t have enough in savings to pay for medical expenses, the company established the Aflac Care Index to educate and advocate for peoples’ health and financial security — including those people who have health care coverage. While U.S. consumers are facing historically high levels of inflation for household spending on food, petrol, and home goods, health consumers will be dealing with greater out-of-pocket spending based
The Trust Deficit Is Bad for Health: A Health/Care Lens on the 2022 Edelman Trust Barometer
“Health is the cornerstone to our core needs, thereby the cornerstone to trust.” So wrote Kirsty Graham, Global Leader of Sectors and Global Chair of Health at Edelman, in an essay explaining the 2022 Edelman Trust Barometer. If it’s January, it must be time for the World Economic Forum in Davos, the annual setting for Edelman’s launch of the company’s Trust Barometer. While WEF is mostly virtual this year due to the pandemic, Edelman has released the survey of global citizens’ views on trust in institutions right on-time and in full and sobering detail. I welcome and dig into the
The 2022 Health Populi TrendCast for Consumers and Health Citizens
I cannot recall a season when so many health consumer studies have been launched into my email inbox. While I have believed consumers’ health engagement has been The New Black for the bulk of my career span, the current Zeitgeist for health care consumerism reflects that futurist mantra: “”We tend to overestimate the effect of a technology in the short run and underestimate the effect in the long run,” coined by Roy Amara, past president of Institute for the Future. That well-used and timely observation is known as Amara’s Law. This feels especially apt right “now” as we enter 2022,
Aflac Finds Health Care and Financial Stress will “Dampen 2021 Holiday Magic” in U.S. Households
Most U.S. householders that experienced COVID-19 expect their 2021 December holidays will be impacted in terms of reducing their holiday gift or decor spending, canceling holiday travel plans to see family or friends, or canceling holiday events, according to the 2021 Aflac Health Care Issues Survey. Aflac polled 1,003 U.S. adults in September 2021 to gauge Americans’ financial health perspectives approaching the end of Year 2 of the COVID-19 pandemic in America. Families with children feel particularly strapped for the 2021 holiday season: while they will be less likely to reduce holiday spending, one-half are concerned about medical expenses compared with
Health Citizens Link Their Views on Democracy, the Economy and the Pandemic
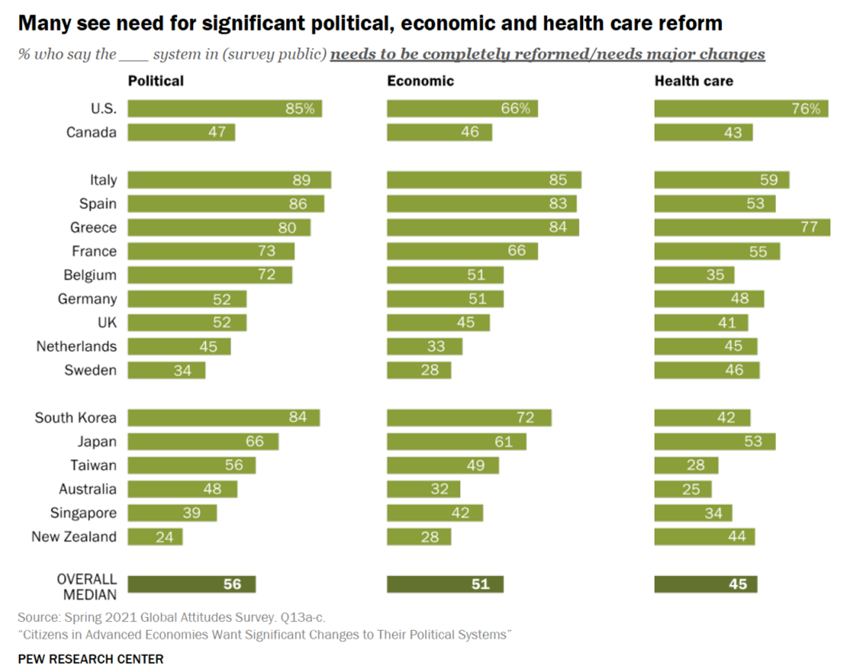
The pandemic has put health care top-of-mind for health citizens the world over. As the public health crisis continues its up-and-downticks around the globe, people are connecting health care to their national economies and politics, based on a global survey from the Pew Research Center, Citizens in Advanced Economies Want Significant Changes to Their Political Systems. For this analysis, the Pew research team assessed the views of some 2,600 health citizens living in 17 developed countries in February 2021. The study report was published in late October 2021. Shown in the first bar chart, the majority of people in at least
The Cost to Cover Health Insurance for a Family in America Is $22,221
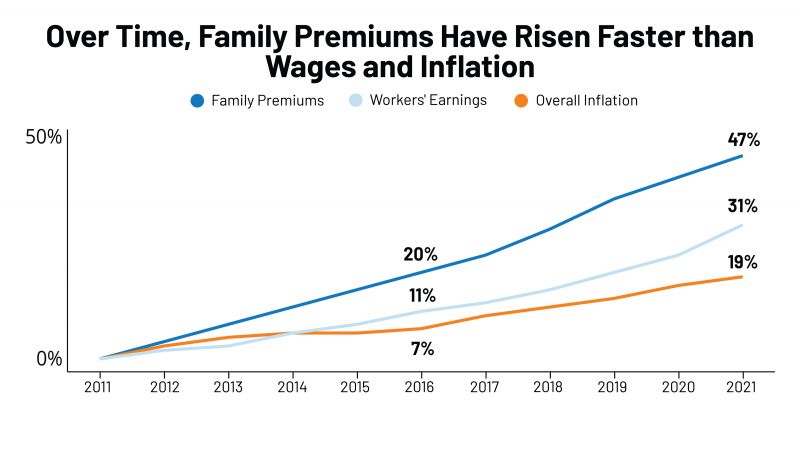
Even with growing inflation in the U.S. and post-pandemic job growth in 2021, the cost of health insurance premiums rose faster than either the price of goods or wages. That family health plan premium reached $22,221, an increase of 22% since 2016, we learn in the annual report from Kaiser Family Foundation, 2021 Employer Health Benefits Survey. This report is our go-to encyclopedia of statistics on health insurance year-after-year, surveying companies’ annual health insurance strategies for coverage and tactics for managing spending and workers’ health outcomes. This 2021 update takes into account the impacts and influence of COVID-19 on workers’
Effective Health Spending Is An Investment, Not a Cost: the Bottom-Line from OECD Health at a Glance 2021
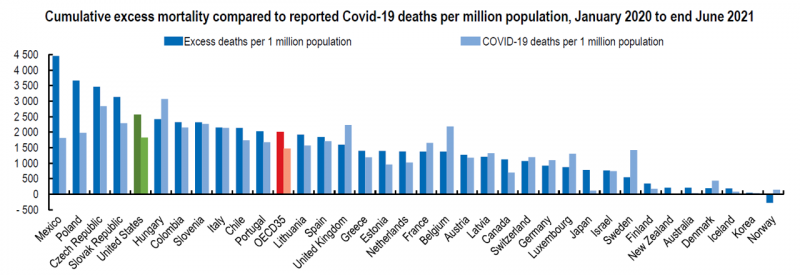
“The pandemic has shown that effective health spending is an investment, not a cost to be contained: stronger, more resilient health systems protect both populations and economies,” the OECD states in the first paragraph of the organization’s perennially-updated report, Health at a Glance 2021. This version of the global report incorporates public health data from the “OECD35,” 35 nations from “A” to “U” (Australia to United States) quantifying excess deaths experienced during the COVID-19 pandemic, the obesity epidemic, mental and behavioral health burdens, and health care spending, among many other metrics. The first chart illustrates that calculation of excess deaths,
Health Consumers, Health Citizens, and Wearable Tech – My Chat with João Bocas

The most effective, engaging, and enchanting digital health innovations speak to patients beyond their role as health consumers and caregivers: digital health is at its best when it addresses peoples’ health citizenship. I had the great experience brainstorming the convergence of digital health, wearable tech, user-centered (UX) design, and health citizenship with João Bocas, @WearablesExpert, in a on his podcast. And if those topics weren’t enough, I wove in the role of LEGO for our well-being, “playing well,” and inspiring STEM- and science-thinking. João and I started our chat first defining health citizenship, which is a phrase I first learned from
“Complexity is Profitable” in U.S. Healthcare – How to Save a Quarter-Trillion Dollars
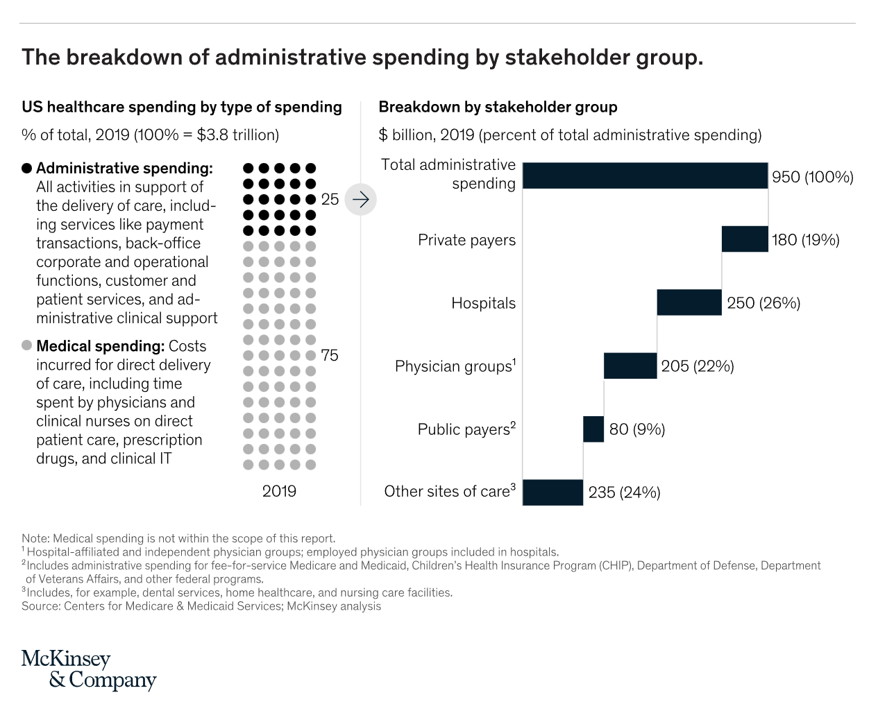
In the U.S., “Health care is complicated because complexity is profitable.” So explain Bob Kocher, MD, and Anuraag Chigurupati, in a viewpoint on Economic Incentives for Administrative Simplification, published this week in JAMA. Dr. Kocher, a physician who is a venture capitalist, and Chigurupati, head of member experience at Devoted Health, explain the misaligned incentives that impede progress in reducing administrative spending. This essay joins two others in the October 20, 2021 issue of JAMA which highlight administrative spending in American health care: Administrative Simplification and the Potential for Saving a Quarter-Trillion Dollars in Health Care by Nikhil Sahni, Brandon
Support for Drug Price Negotiation Brings Partisans Together in the U.S.
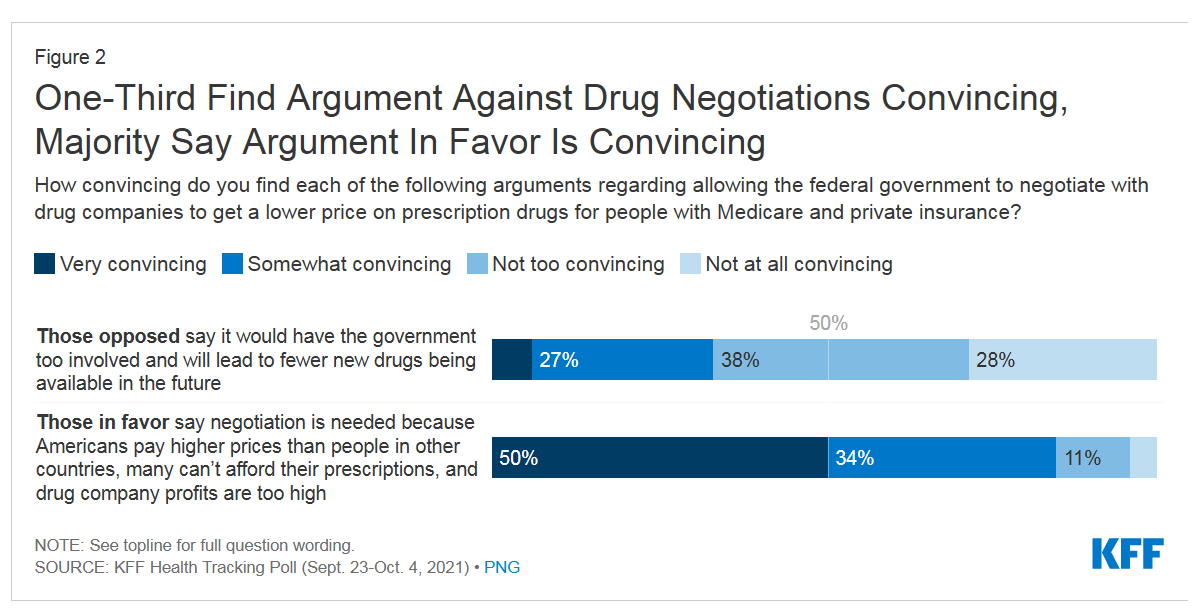
Most U.S. adults across political parties favor allowing the Federal government authority to negotiate for drug prices — even after hearing the arguments against the health policy. Drug price negotiation, say by the Medicare program, is a unifying public policy in the current era of political schisms in America, based on the findings in a special Kaiser Family Foundation (KFF) Health Tracking Poll conducted in late September-early October 2021. Overall, 4 in 5 Americans favor allowing the Federal government negotiating power for prescription drug prices, shown in the first chart from the KFF report. By party, nearly all Democrats agree
Why Is So Much “Patient Experience” Effort Focused on Financial Experience?
Financial Experience (let’s call it FX) is the next big thing in the world of patient experience and health care. Patients, as health consumers, have taken on more of the financial risk for health care payments. The growth of high-deductible health plans as well as people paying more out-of-pocket exposes patients’ wallets in ways that implore the health care industry to serve up a better retail experience for patients. But that just isn’t happening. One of the challenges has been price transparency, which is the central premise of this weekend’s New York Times research-rich article by reporters Sarah Kliff and
Nurses and Aides Are Beloved and Deserve Higher Pay; and a Spotlight on the Filipinx Frontline
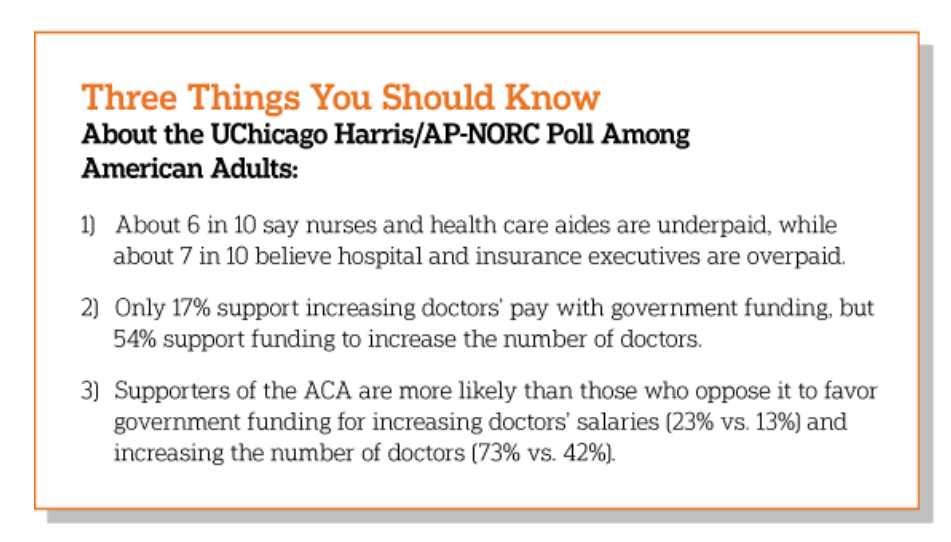
A majority of Democrats, Independents, and Republicans agree that nurses are underpaid. Most Americans across political parties also believe that hospital executives are overpaid, according to a poll from The Associated Press-NORC Center for Public Affairs Research. The survey analysis is aptly titled, Most Americans Agree That Nurses and Aides Are Underpaid, While Few Support Using Federal Dollars to Increase Pay for Doctors, . Insurance executives are also overpaid, according to 73% of Americans — an even higher percent of people than the 68% saying hospital execs make too much money. In addition to nurses being underpaid, 6 in 10
Doctors’ Offices Morph into Bill Collectors As Patients Face Growing Out-Of-Pocket Costs
In the U.S., patients have assumed the role of health care payors with growing co-payments, coinsurance amounts, and deductibles pushing peoples’ out-of-pocket costs up. This has raised the importance of price transparency, which is based on the hypothesis that if patients had access to personally-relevant price/cost information from doctors and hospitals for medical services, and pharmacies and PBMs for prescription drugs, the patient would behave as a consumer and shop around. That hypothesis has not been well proven-out: even though more health care “sellers” on the supply side have begun to post price information for services, patients still haven’t donned
Medical Debt in the U.S. Greater in States That Did Not Expand Medicaid
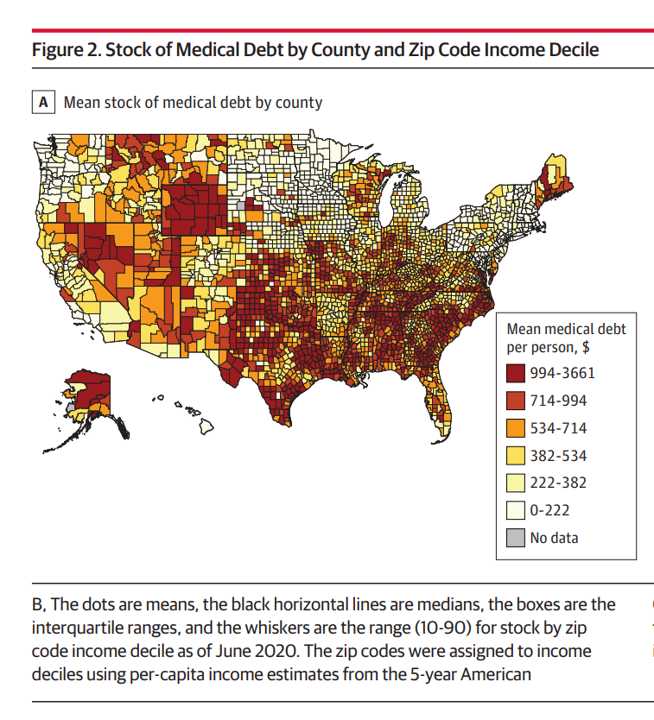
The level of medical debt in America exceeded debt of other types in 2020. Furthermore, the flow of medical debt was greater among health citizens living in states that did not expand Medicaid as part of the Affordable Care Act, compared with patients who reside in Medicaid expansion states, according to an original research essay, Medical Debt in the US, 2009-2020 published in JAMA on 20 July 2021. The first line chart illustrates the trends in medical debt in collections by state expansion of Medicaid, with the bottom darkest line representing debt in collections in Medicaid expansion states from the
Digital Inclusion As Upstream Health Investment
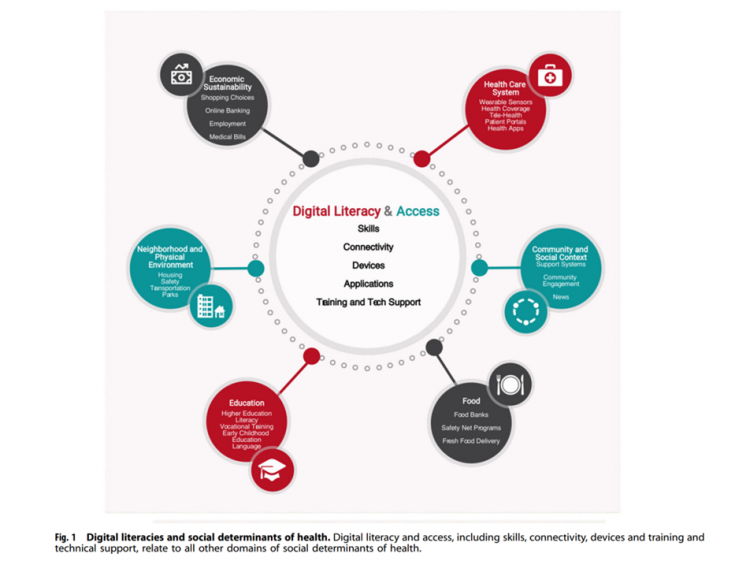
Without access to connectivity during the pandemic, too many people could not work for their living, attend school and learn, connect with loved ones, or get health care. The COVID-19 era has shined a bright light on what some of us have been saying since the advent of the Internet’s emergence in health care: that digital literacies and connectivity are “super social determinants of health” because they underpin other social determinants of health, discussed in Digital inclusion as a social determinant of health, published in Nature’s npj Digital Medicine. On the downside, lack of access to digital tools and literacies
Aduhelm and Alzheimer’s Disease: A Potential Medicare Budget-Buster Puts A Blazing Light on Health Care Costs and Innovation
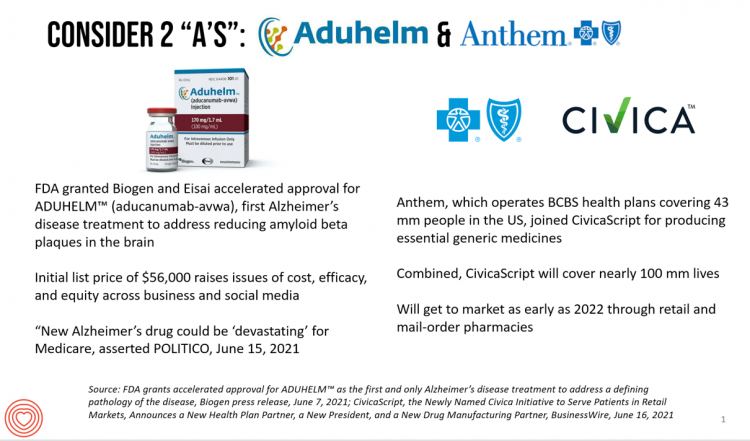
The FDA’s approval of the first therapy to treat Alzheimer’s Disease in over twenty years brought attention to a not-yet-convened debate of U.S. health care costs and spending, innovation, and return-on-the-investment (as well as “for whom” do the returns accrue). In my latest post for Medecision, I explore different angles on the Aduhelm and Alzheimer’s discussion, covering: The macro- and micro-economics of Alzheimer’s and the $56,000 list price for the drug The FDA regulatory process and aftermath U.S. consumers’ bipartisan support for drug price regulation through Medicare negotiation and private/commercial sector adoption Congressional legislation addressing the price of medicines in





 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.